
DR P. MARAZZI / Science Photo Library
Many patients will present to community pharmacies with oral and dental emergencies, especially outside of their dentist’s opening hours.
This article — the second of three on dental emergencies — discusses hard tissue conditions and follows on from a previous article on soft tissue conditions[1]
.
The conditions and advice included in this article is not exhaustive. If pharmacy professionals are uncertain on how to manage a patient, advice should be obtained from relevant guidance. NHS 111 can provide urgent care advice, while emergency services should be contacted by dialling 999 in a life-threatening emergency.
- Toothache
- Toothache with sinus involvement
- Problem filling or crown
- Displacement of a tooth from its socket/chipped tooth
- Jaw pain
- Dry socket
Pain assessment
People presenting in community pharmacy with oral problems may often complain of pain and discomfort; therefore, a systematic approach to assessing pain is essential in evaluating the problem before providing appropriate advice. The mnemonic ‘SOCRATES’ is a useful approach in order to obtain a thorough pain history[2]
:
- Site — Where is the pain?
- Onset — When did the pain start?
- Character— Is the pain burning/tingling/electric shock-like/throbbing?
- Radiation — Does the pain move or spread elsewhere?
- Associated symptoms — Are there other problems (e.g. bad breath)?
- Time — How long does the pain last?
- Exacerbating/relieving factors — Does anything reduce the pain or make it worse?
- Severity — How severe is the pain on a pain scale of 1 to 10? (1 being the least painful and 10 being the worst).
Following this assessment, relevant pain management options can be offered and the patient can be signposted to appropriate ongoing care. The Table outlines some examples of the types of toothache presentations[3]
. Even if the patient is being referred onwards, or there is uncertainty on the management options, providing as much information about the problem to the next healthcare professional will help the patient to be triaged to the most appropriate professional.
| Type of dental pain | Summary | Characteristics | Management with pharmacist in interim to seeking dental advice | Management with dentist |
|---|---|---|---|---|
| Dentine hypersensitivity | Pain from exposed dentine in response to thermal, tactile or osmotic stimulus |
|
|
|
| Cracked tooth | A crack in the tooth that may extend into the pulp (which contains the blood and nerve supply to the tooth) or under the gum |
|
|
|
| Reversible pulpitis | Mild inflammation of the pulp of the tooth, often caused by dental decay |
|
|
|
| Irreversible pulpitis | Severe inflammation of the pulp of the tooth, often caused by dental decay |
|
|
|
| Acute periapical periodontitis | Inflammation around the apex of the root of the tooth, which may be caused by bacteria entering the pulp of the tooth |
|
|
|
| Acute periapical abscess | Infection of the root canal of the tooth, which may manifest as a collection of pus |
|
|
|
| Source: Oxford Handbook of Clinical Dentistry [3] , NHS Health Education England[4] , Scottish Dental Clinical Effectiveness Programme[5] | ||||
Toothache
Tooth decay or a fracture may result in irritation and infection of the nerve inside the tooth. This can manifest as a dull, aching pain which might disturb sleep and can be exacerbated by placing pressure on the tooth[3]
,[4]
.
Diagnosis
Questions to ask the patient:
- Is the pain a constant dull ache or short, sharp pain?
- What triggers the pain?
- Is there a broken tooth?
- Is there a lost filling or crown?
- Is your mouth or face swollen?
- Have you had a cold/sinus symptoms recently?
Advice
- If there is short, sharp pain, applying a desensitising toothpaste may provide some relief;
- A temporary dental filling kit may provide relief for a broken tooth or lost filling/crown;
- Paracetamol and ibuprofen can be taken as an alternate dose every 4–6 hours (dependent on dose and contraindications);
- Maintain good oral hygiene (e.g. brushing teeth twice a day);
- Avoid pain triggers (e.g. keep to a soft diet and avoid biting on the tooth).
This advice is only a temporary solution; therefore, patients must be advised to seek a dental assessment, even if the pain resolves. Further treatment for the tooth, including a nerve treatment or removal of the tooth, may be required[4]
.
Dental pain that is associated with a decayed or fractured tooth can lead to a dental swelling or abscess, which can occur inside the mouth or on the face. This requires an urgent dental assessment or emergency care if there is evidence of airway compromise[4],[5]
.
Toothache with sinus involvement
Orofacial pain (pain experienced in the mouth, jaws and the face) or pain of the upper teeth may occur concurrently with sinus complaints, making it difficult to identify the source of the discomfort (i.e. sinogenic, dental or both).
The maxillary sinus is the most common cause of an orofacial pain with a sinogenic component. Ciliated columnar epithelium lines the sinuses and produces mucus, which is moved by the action of cilia and eventually drains into the nasal space. Once in the nasal space, mucus passes into the nasopharynx and is swallowed. In sinus disease, reduced ciliary activity or an obstruction may impede this process and result in symptoms[6]
.
Diagnosis
Toothache accompanied by the following may suggest an acute sinusitis of the maxillary sinus[5],[6]
.
- Fever;
- Fatigue;
- Decreased sense of smell;
- Nasal obstruction or discharge;
- A concurrent or recent upper respiratory tract infection;
- Pain experienced in the face as a headache or a toothache (especially of the upper teeth) that increases when bending down.
Advice
Treatment of acute sinusitis includes topical nasal decongestants and saline irrigation of the nasal cavity. Unless there is evidence of pyrexia or spread of infection beyond the sinus, antibiotics are not indicated[6]
.
If sinus involvement is suspected, the patient should be advised to seek further assessment of their symptoms by their dentist or GP.
Problem filling or crown
A filling is designed to repair a cavity inside a tooth, usually caused by tooth decay. A crown is a type of cap that can completely cover a natural tooth and is used to prevent a tooth from cracking. Fillings and crowns vary in appearance depending on the material used, and might appear as metal (e.g. silver or gold) or white (to match the rest of the teeth).
Fillings and crowns fail for various reasons, including disease developing inside the tooth (e.g. decay or a crack) or a failure in the cement holding the filling or crown onto the tooth. If a filling or crown is broken or lost, the nerve inside the tooth becomes vulnerable to irritation or infection, which may or may not present as pain from the affected tooth[3]
.
Diagnosis
Questions to ask the patient:
- Is the tooth painful?
- Is the remaining tooth sharp or causing soreness inside the mouth?
- Does the crown fit back over the tooth comfortably without falling off?
Advice
Paracetamol and ibuprofen should be taken as an alternate dose every 4–6 hours (dependent on dose and contraindications). If there is an open cavity or fractured tooth, a temporary filling or crown repair kit can be used, however, a dental assessment is the best option in all cases for further assessment[4],[5]
.
If it is known or suspected that the patient has inhaled a piece of tooth, filling or restoration, the patients should be referred immediately to emergency care. A chest X-ray may be required owing to the risk of aspiration-related pneumonia[5]
.
Displacement of a tooth from its socket/chipped tooth
Avulsion (a tooth that has been completely lost from the mouth)[7]
is regarded as the most severe dento-alveolar injury, with some teeth eventually being lost owing to a failure to re-implant the tooth or failure of the tooth to successfully function following re-implantation.
The time a tooth is kept dry prior to replantation has a significant negative effect on the healing outcomes for the tooth. Therefore, the sooner the tooth is re-implanted, the better the long term outlook[8]
.
Diagnosis
Questions to ask the patient or parent/guardian:
- When and how did the accident happen?
- Is the tooth a primary (baby) or permanent (adult) tooth?
- Is the tooth or piece of tooth missing or has it been swallowed?
- Is the patient’s tetanus vaccination up to date? If not, consult with a GP for advice.
If the tooth or piece of tooth is unaccounted for, the patient should be sent immediately to emergency care. A chest X-ray may be required owing to the risk of aspiration-related pneumonia[5]
.
If the patient or their parent/guardian has the tooth and it is a primary tooth, it should not be replanted. If it is a permanent tooth, it should be re-implanted into the mouth as soon as possible.
Advice
Pharmacy professionals can advise patients to take the following steps[7]
for a permanent tooth that has been knocked out (see Figure):
- Keep calm;
- Pick up the tooth up by the crown (the white part) and avoid touching the root (the yellow part);
- If the tooth is dirty, wash it briefly for 10 seconds under cold running water and reposition it;
- The patient/parent/guardian should re-implant the tooth then the patient should bite on a handkerchief to hold it in position.
If it is not possible to replant the tooth, place it in a glass of milk or a special storage media for avulsed teeth (e.g. Hanks’s balanced storage medium or saline)[7]
. Alternatively, the tooth can be transported in the mouth, keeping it between the molars and the inside of the cheek. If the patient is very young, this method could result in swallowing of the tooth; therefore, it is advisable to ask the patient to spit into a container and place the tooth in it. The tooth should not be stored in water[7]
,[8]
. The patient should be referred to their dentist immediately.
For a chipped permanent tooth, the patient should be referred to their dentist as soon as possible.
Other general advice to follow includes[7]
:
- Follow a soft diet;
- Avoid participation in contact sports;
- Brush the teeth with a soft toothbrush after each meal;
- Use a chlorhexidine (0.1%) mouth rinse twice daily for one week.
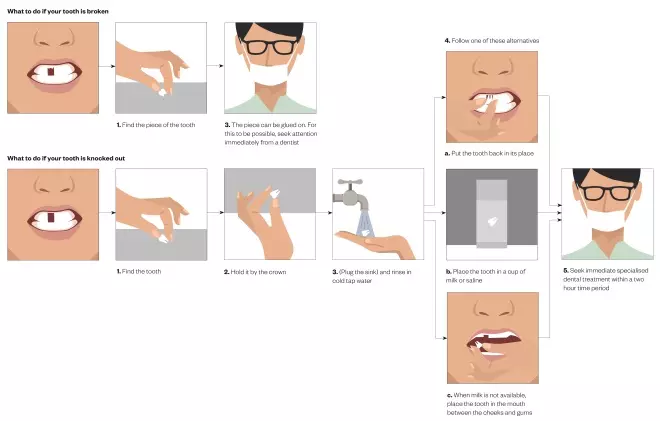
Figure 1: What to do when a tooth has broken or been knocked out
Source: JL / The Pharmaceutical Journal
Dental injuries and safeguarding
Safeguarding considerations should always be made when pharmacy professionals are presented with a cause of dental trauma because orofacial trauma occurs in at least 50% of children who have been physically abused[9],[10]
. A child with one injury may have further injuries that are not visible[9],[10]
.
During history taking, pharmacy professionals should consider whether[10]
:
- The injury could have been caused accidentally and, if so, how?
- The explanation for the injury fits the age and clinical findings;
- The explanation of the cause is consistent with the injury, and within the normally acceptable limits of behaviour;
- There has been any delay in seeking advice and the reasons;
- The story of the accident varies.
If there are concerns about a child and no satisfactory explanation for the dental injury, pharmacy professionals should contact the local authority for advice on raising concerns[11]
.
Jaw pain
The temporomandibular joint connects the lower jaw to the skull. The movement in this joint allows the mouth to open and close, and chew from side-to-side[12]
. Pain or stiffness in the jaw muscles can be a sign of dysfunction of the temporomandibular joint, which is a common phenomenon, with temporomandibular disorders being the third most common chronic pain disorder[13]
.
The cause of dysfunction of the joint is frequently multifactorial and symptoms may be acute or chronic. Overuse of the jaw, clenching or grinding the teeth and stress are implicated in the condition. It may also present following dental treatment (e.g. after having a lower wisdom tooth extraction). These factors can result in fatigue or spasm of the muscles around the joint[14]
.
Diagnosis
Questions to ask the patient:
- Are there noises from the joint (e.g. clicking or grating associated with movement)?
- Is mouth opening limited?
- Is there a concurrent headache or earache?
- Does chewing exacerbate the pain?
- Do you clench or grind your teeth?
- Has it been a particularly stressful time in their life?
- Is chest and jaw pain worse on exertion?
- Is there visual disturbance?
Patients over the age of 50 years old with visual disturbances, such as reduced vision, and pain in the temple area may be at risk of a giant cell (temporal) arteritis. In these cases, urgent medical care should be sought owing to the risk of vision loss[5]
.
Chest pain owing to angina or a myocardial infarction can radiate to the jaw; therefore, it is important to ask patients about any co-morbidities or history of heart problems[4]
. If angina or myocardial infarction is suspected, call 999.
Jaw pain of muscular origin should be managed conservatively in the interim prior to the patient seeking a dental assessment.
Advice
Suitable advice to offer the patient:
- Follow a soft diet for two weeks;
- Limit mouth opening when yawing or eating (e.g. by placing the fist under the chin);
- Avoid recurrent chewing habits, such as chewing gum or finger nail biting;
- Ibuprofen gel rubbed into the skin of the face or taken in tablet form can provide pain relief;
- Apply a warm or cold compress over the affected area;
- Massage sore areas of the face;
- Relaxation;
- Rest the jaw.
If these methods do not manage the symptoms, interventions, such as a bite guard or involvement from a dental specialist may be required[4],[5]
,[14]
.
Dry socket
Dry socket, formally known as ‘alveolar osteitis’, is the inflammation of a socket after a tooth is extracted. It may be considered both a soft- and hard-tissue condition with inflammation of the gums and delayed healing of the bony socket. This is particularly common in lower molar tooth extractions and those who smoke following an extraction are at increased risk[5]
.
The condition usually presents with pain in the extraction site, which can begin 24–48 hours after the tooth was removed. There may be tenderness in the region and an unpleasant smell or taste. Swelling can also develop[5]
.
Diagnosis
Questions to ask the patient:
- Has a tooth been removed recently in the region of the pain? If so:
- Have you followed after-care instructions following removal of the tooth?
- Have you smoked since the tooth was removed?
- Has a swelling been present?
If the patient has a swelling, determine whether they can swallow their own saliva and breathe normally. If there are any signs of airway compromise, the patient should attend A&E immediately[5]
.
Advice
Suitable advice to offer the patient:
- Paracetamol and ibuprofen should be taken as an alternate dose every 4–6 hours (dependent on dose and contraindications);
- Avoid smoking and alcohol;
- Maintain good oral hygiene;
- Rinse the area with warm salty water;
- Brush the teeth twice daily for two minutes, but avoid placing the toothbrush in the extraction socket.
Patients with a history of radiotherapy to the head and neck region or those with risk factors for medication-related osteonecrosis of the jaw (MRONJ) are at an increased risk of delayed healing or complications arising from the healing of a socket following a tooth extraction[15]
. The risk of MRONJ is increased in patients taking anti-resorptive or anti-angiogenic drugs. Implicated drugs include anti-resorptive drugs (e.g. the bisphosphonates and denosumab) and anti-angiogenic therapies (e.g. bevacizumab, sunitinib and aflibercept)[15]
.
The patient should seek assessment with a dentist as soon as possible. Following a dental examination, a dressing material may need to be placed into the socket to relieve the symptoms. If there are signs of spreading infection, systemic infection or if the patient is immunocompromised, a course of antibiotics may be indicated[5]
.
Useful resources
- NHS Health Education England — Managing dental and oral presentations in community pharmacy: https://www.lasepharmacy.hee.nhs.uk/dyn/_assets/_folder4/community-pharmacy/dental-fact-sheets/pharmacydentalfactsheetsfullset.pdf
- Scottish Dental Clinical Effectiveness Programme — Management of acute dental problems: guidance for healthcare professionals: http://www.sdcep.org.uk/wp-content/uploads/2013/03/SDCEP+MADP+Guidance+March+2013.pdf
- The Dental Trauma Guide —
IADT treatment guidelines for avulsion: https://dentaltraumaguide.org/free-dental-guides/permanent-teeth/avulsion/ - Scottish Dental Clinical Effectiveness Programme — Oral health management of patients at risk of medication-related osteonecrosis of the jaw: http://www.sdcep.org.uk/wp-content/uploads/2017/04/SDCEP-Oral-Health-Management-of-Patients-at-Risk-of-MRONJ-Guidance-full.pdf
References
[1] Virdee J & Amin K. Managing dental emergencies in community pharmacy: soft tissue conditions. Pharm J 2018;301(7917) doi: 10.1211/PJ.2018.20205325
[2] Orofacial Pain. Pain assessment. 2016. Available at: http://www.orofacialpain.org.uk/education/pain-assessment/ (accessed May 2019)
[3] Mitchell DA & Mitchell L. Oxford Handbook of Clinical Dentistry 6th edition. London: Oxford University Press; 2014
[4] NHS Health Education England. Managing dental and oral presentations in community pharmacy. 2018. Available at: https://www.lasepharmacy.hee.nhs.uk/dyn/_assets/_folder4/community-pharmacy/dental-fact-sheets/pharmacydentalfactsheetsfullset.pdf (accessed May 2019)
[5] Scottish Dental Clinical Effectiveness Programme. Management of acute dental problems: guidance for healthcare professionals. 2013. Available at: http://www.sdcep.org.uk/wp-content/uploads/2013/03/SDCEP+MADP+Guidance+March+2013.pdf (accessed May 2019)
[6] Bell GW, Joshi BB & Macleod RI. Maxillary sinus disease: diagnosis and treatment. Br Dent J 2011;210:113–118. doi: 10.1038/sj.bdj.2011.47
[7] Dental Trauma Guide. Avulsion. 2018. Available at: https://dentaltraumaguide.org/free-dental-guides/permanent-teeth/avulsion/ (accessed May 2019)
[8] PF Day & Gregg TA. Treatment of avulsed permanent teeth in children. 2012. Available at: https://www.bspd.co.uk/Portals/0/Public/Files/Guidelines/avulsion_guidelines_v7_final_.pdf (accessed May 2019)
[9] Becker DB, Needleman HL & Kotelchuck M. Child abuse and dentistry; orofacial trauma and its recognition by dentists. J Am Dent Assoc 1978;97:24–28. PMID: 28343
[10] Cairns AM, Mok JYQ & Welbury RR. Injuries to the head, face, mouth and neck in physically abused children in a community setting. Int J Paediatr Dent 2005;15:310–318. doi: 10.1111/j.1365-263X.2005.00661.x
[11] National Institute for Heath and Care Excellence (NICE). Child abuse and neglect clinical guideline [NG76]. 2017. Available at: https://www.nice.org.uk/guidance/ng76/chapter/Recommendations (accessed May 2019)
[12] Oral Health Foundation. Jaw problems and headaches. 2017. Available at: https://www.dentalhealth.org/jaw-problems-and-headaches (accessed May 2019)
[13] Prasad SR, Kumar NR, Shruthi H & Kalavathi S. Temporomandibular pain. J Oral Maxillofac Pathol 2016; 20:272–275. doi: 10.4103/0973-029X.185902
[14] Durham J, Aggarwal V, Davies S et al. Temporomandibular Disorders (TMDs): an update and management guidance for primary care from the UK Specialist Interest Group in Orofacial Pain and TMDs. The Royal College of Surgeons of England, 2013;22.
[15] Scottish Dental Clinical Effectiveness Programme. Oral Health Management of Patients at Risk of Medication-related Osteonecrosis of the Jaw. 2017. Available at: http://www.sdcep.org.uk/wp-content/uploads/2017/04/SDCEP-Oral-Health-Management-of-Patients-at-Risk-of-MRONJ-Guidance-full.pdf (accessed May 2019)


