
Science Photo Library
As part of the five-year ‘Community pharmacy contractual framework’, a range of new services are being piloted in community pharmacy, including developing an early detection service for hypertension[1]
. Each year, the management of hypertension costs the NHS upwards of £2bn and complications associated with the condition contribute to further costs, particularly in relation to hospital stays and recuperation[2]
. According to Public Health England (PHE), more than one in four adults in England are affected by high blood pressure (BP), equivalent to 12.5 million people. More men than women are living with the condition (31% of men vs. 26% of women), yet, worryingly, nearly 6 million people in England are believed to have undiagnosed hypertension[2]
.
There are several lifestyle factors that increase a person’s risk of hypertension, which are detailed below. This article will discuss the evidence base for how diet and exercise could support patients in the self-management of their condition, and how pharmacists and their teams can deliver this healthy living advice.
Causes and risk factors
Non-modifiable risk factors for hypertension include gender, age, ethnicity and family history. For example, people from a black African-Caribbean background have a higher risk of hypertension than people of other ethnicities[2]
. Although the risk of developing hypertension increases with age, over 2.1 million people under the age of 45 years have high BP[2]
. Adults aged 40 years and over are advised to have their BP checked by a healthcare professional at least once every five years, or more often if their BP is considered to be high–normal[3]
. Depending on a patient’s BP reading, a community pharmacist should either advise them on diet and lifestyle changes to manage their BP, or refer them to their GP for further checks. A community pharmacist should only share confidential patient information with a GP if they have obtained the patient’s consent
[4]
.
Modifiable risk factors for hypertension include:
- Excess dietary salt intake;
- Being overweight or obese;
- Lack of exercise;
- Excessive alcohol consumption;
- High consumption of caffeine[2],[5],[6]
.
Elevated BP that cannot be linked to an identifiable cause is termed ‘primary hypertension’, while ‘secondary hypertension’, which accounts for 10% of hypertension cases, is often caused by an underlying medical condition or the use of particular medicines[7]
. Most commonly, secondary hypertension is associated with conditions such as kidney disease, obstructive sleep apnoea and thyroid disorders, as well as the use of medicines such as non-steroidal anti-inflammatory drugs and decongestants[7]
.
Symptoms
Hypertension is often referred to as the ‘silent killer’ because it is an asymptomatic condition for many people[8]
. For some people, the only way to determine if they have hypertension is by measuring their BP. For others, certain symptoms can indicate raised BP, such as shortness of breath, headaches, nosebleeds and issues with vision[3]
. Anyone experiencing these symptoms should be referred to their GP for further tests.
Diagnosis
Patients must have their BP measured in a clinical setting by a healthcare professional, such as a pharmacist, nurse or GP[9]
. The National Institute for Health and Care Excellence (NICE) suggests that if an in-clinic BP reading is 140/90mmHg or higher, a second BP reading should be taken during the same consultation. If there is a large difference between the first and second measurements, a third reading should be taken. The lower of the second and third BP readings should be noted as the in-clinic reading[9]
. It is important to take the BP reading on both arms to identify any differences between the two.
Testing BP in a clinical setting can be associated with the ‘white coat effect’ (i.e. the process of having their BP measured causes the patient’s BP to be raised). Therefore, patients who have an in-clinic BP measurement of between 140/90mmHg and 180/120mmHg should be offered ambulatory blood pressure (measuring BP on a continuous basis [ABP]) monitoring or home blood pressure (HBP) monitoring[9]
. These involve taking multiple BP readings over the course of the patient’s waking day, with an average value of these readings then noted as the patient’s BP[9]
.
During the process of confirming whether or not a patient has hypertension, NICE recommends that healthcare professionals investigate any target organ damage and use a validated tool (such as the QRISK tool) to carry out a cardiovascular risk assessment on the patient[10]
.
A patient is confirmed as having hypertension if they have an in-clinic BP reading of 140/90mmHg or higher and an ABP or HBP average reading of 135/85mmHg or higher[9]
. Their condition is then categorised into one of three stages:
- Stage 1 — in-clinic BP of between 140/90mmHg and 159/99mmHg, and an ABP or HBP average of between 135/85mmHg and 149/94mmHg;
- Stage 2 — in-clinic BP 160/100mmHg or higher, but less than 180/120mmHg, and subsequent ABP daytime average or HBP average BP of 150/95mmHg or higher;
- Stage 3 — in-clinic systolic BP of 180mmHg or higher, or in-clinic diastolic BP of 120mmHg or higher[9]
.
Patients aged over 40 years, who are not diagnosed as being hypertensive, should have their BP remeasured within the next five years.
Management
In general, patients with stage 2 or stage 3 hypertension will require drug therapy alongside lifestyle changes, while those with stage 1 hypertension may be able to manage their condition with lifestyle changes alone[9]
. Factors that result in someone with stage 1 hypertension requiring drug therapy include having one or more of the following: comorbidities (e.g. diabetes or kidney disease), being under the age of 40 years and having an estimated 10-year cardiovascular disease risk of 10% or more[9]
.
Non-pharmacological interventions
According to NICE guidelines, in the first instance, when a patient is hypertensive or pre-hypertensive, a change in diet and exercise is recommended[9]
. Interventions that address diet, exercise and weight have been found to be effective in reducing systolic BP and diastolic BP by 12.5mmHg and 7.9mmHg, respectively[11]
.
Eating healthily
Diet has a large impact on BP with high salt, caffeine and alcohol intakes being linked to high BP. Current recommendations suggest that salt intake should be limited to 6g per day[12]
. Caffeine consumption should not exceed 4 cups of coffee per day and alcohol consumption should be within the recommendations of 14 units per week (i.e. 6 pints of average-strength beer or 10 small glasses of low-strength wine), which includes 2 alcohol-free days[5],[6],[13]
.
According to the NHS, diet should be based around the ‘Eatwell guide’, published by PHE in 2016, which suggests that a large proportion of a person’s diet should include slow-release carbohydrates (e.g. wholegrain bread), as well as fruit and vegetables[14]
. People are also encouraged to eat protein and a small amount of dairy each day. Foods that are high in salt or sugar are not essential for a balanced diet and are therefore only recommended as treats (e.g. chocolate).
The guide also emphasises the importance of liquid calories[14]
. High-sugar drinks and alcohol all have a major impact on waistlines; for example, data suggest that a large glass of red wine contains around 260 calories, while a pint of beer contains around 170 calories[15]
. Choosing reduced calorie drinks (e.g. zero-sugar alternatives) can help with weight loss. In addition, the guide recommends eight glasses of water per day
[14].
PHE also aims to improve health literacy by trying to educate the public on how to interpret information on food and drink labels[14]
. Recent research has shown that there are low levels of health literacy among the public, meaning that people can find it difficult to interpret whether something is healthy or not[16]
. Food and drink labels can be confusing, meaning that people often choose unhealthy options, even if their intention is to be healthy.
Tools have been introduced to tackle issues with health literacy. For example, the Change4Life food scanner app allows members of the public to scan food and drink items[17],[18]
. The app then indicates whether a product is high in calories, fat, salt and sugar, and suggests healthier alternatives. Pharmacists can recommend simple tools like this to help the public make informed decisions about which food and drinks are healthy.
Exercising regularly
One of PHE’s priorities is to increase levels of physical activity across the population[19]
. Current guidelines suggest that people should aim to achieve 150 minutes of moderate-intensity exercise each week (e.g. brisk walking or volleyball) or 75 minutes of vigorous intensity exercise (e.g. running or playing football)[20]
. In addition to these types of exercises, which are often referred to as ‘cardio’, people should also aim for two days per week of muscle-building exercises to support strong bones and joints[20]
. PHE indicates that the benefits of exercise do not only reduce the risks of cardiovascular disease, but also many other health risks (see Figure 1).
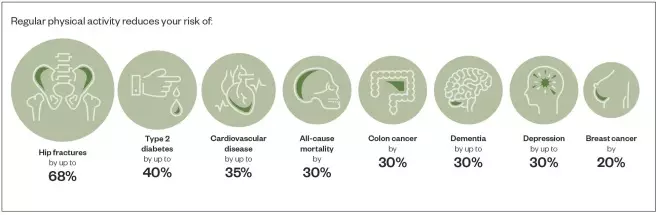
Figure 1: Health risks that can be reduced by regular physical activity
Source: Reproduced with permission from gov.uk (under Open Government Licence v3.0)[19]
Losing weight
The NHS has developed a free 12-week weight loss programme that aims to support the public to lose weight in line with NICE recommendations[21]
. Programme users are encouraged to stay within a defined daily calorie intake that is specific to them. Following the programme should result in weight loss of 0.5–1.0kg each week. The aim of the programme is to help users to lose 5–10% of their body weight over a 12-week period.
As mentioned previously, health literacy can be a challenge for many people; therefore, tools to help count calories while participating in the programme are important[16]
. The NHS recommends its calorie checker as well as the MyFitnessPal (Under Armour) app that allows users to keep track of their calorie intake and record their weight weekly[22],[23]
.
Other recommendations
The amount of sleep a person gets and how much stress they are under can also have an impact on their BP. Finding ways to relax and unwind can support patients to improve their lifestyle and feelings of general wellbeing, as well as reduce their BP[2]
.
Patients who smoke should be encouraged to stop and referred to smoking cessation services.
How community pharmacy can help
PHE has issued a ‘call to action’ for community pharmacy teams to support its agenda to reduce the number of people living with hypertension (see Figure 2)[2]
. The call says that pharmacy teams should:
- Offer opportunistic BP testing to their patients;
- Provide advice and support to encourage healthy lifestyles;
- Deliver the ‘NHS health check service’[2]
.
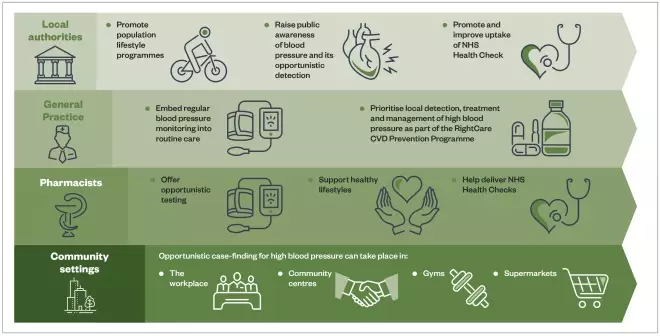
Figure 2: A call to action by Public Health England for different sectors to work together to reduce the number of people living with hypertension
Source: Reproduced with permission from: gov.uk (under Open Government Licence v3.0)[2]
Support public health campaigns
Given that one of the essential pharmacy services is to deliver public health campaigns each year, there is great scope for pharmacy teams to work with local commissioners to prioritise campaigns that encourage optimal BP[24]
. Campaigns that involve taking a patient’s BP, and demonstrating the salt, sugar, calorie and fat content of foods and drinks can help start conversations between the pharmacy team and those who need support in adopting a healthy lifestyle. These techniques can allow pharmacy teams to overcome the stigma of approaching someone with the suggestion that they may need to make changes to their lifestyle.
Support behavioural change
In addition, it is important that pharmacy teams understand the process of behavioural change to best support their patients to make lifestyle changes[25]
. The transtheoretical model of behaviour change, used most commonly by pharmacy teams in the smoking cessation service, explains that when making lifestyle changes patients can go through a process of several stages (e.g. planning, taking action and relapsing; see Figure 3)[26],[27]
. Pharmacy teams can support such patients by using motivational interviewing techniques (see Box) and positive encouragement.
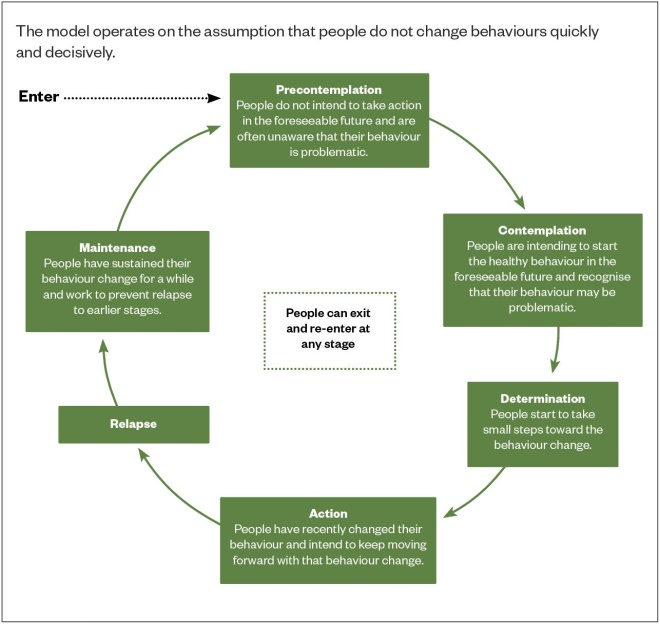
Figure 3: Transtheoretical (stages of change) model
Source: Boston University School of Public Health
[27]
Box: How to encourage patients to change their lifestyle
Express empathy for the patient
- Patients may feel overwhelmed to try and change all their behaviours at once. Encourage them to focus on one lifestyle change at a time, which can then be built on (e.g. focus on eating healthily first, then exercising more).
Be supportive and knowledgeable
- Patients who wish to exercise more may not be able to afford a gym membership. Encourage them to be more active in ways that are free (e.g. taking the stairs instead of the lift or going for a walk at lunchtime);
- For patients who wish to eat more healthily, even small changes can make a big difference (e.g. not adding salt when cooking, or steaming/grilling food rather than frying it).
Provide patients with additional resources
The following organisations can provide more advice and support:
- Blood Pressure UK (tel.: 020 7882 6218);
- British Heart Foundation (tel.: 0300 330 3311);
- Stroke Association (tel.: 0303 3033 100);
- Diabetes UK (tel.: 0345 123 2399).
The mobile apps mentioned in this article may also be of benefit to patients.
As the model for community pharmacy evolves and more community pharmacies become accredited as healthy living pharmacies, the role of the pharmacy team in supporting patients to reduce their BP will become even more important[28]
.
References
[1] Pharmaceutical Services Negotiating Committee. Pharmacy heart checks service pilot announced. 2019. Available at: https://psnc.org.uk/our-news/pharmacy-heart-checks-service-pilot-announced/ (accessed February 2020)
[2] Public Health England. Health matters: combating high blood pressure. 2017. Available at: https://www.gov.uk/government/publications/health-matters-combating-high-blood-pressure/health-matters-combating-high-blood-pressure (accessed February 2020)
[3] NHS Inform. High blood pressure (hypertension). 2019. Available at: https://www.nhsinform.scot/illnesses-and-conditions/heart-and-blood-vessels/conditions/high-blood-pressure-hypertension#symptoms-of-high-blood-pressure (accessed February 2020)
[4] Royal Pharmaceutical Society. Medicines, Ethics and Practice 43. London: Pharmaceutical Press; 2019
[5] Hartley TR, Sung BH, Pincomb GA et al. Hypertension risk status and effect of caffeine on blood pressure. Hypertension 2000;36(1):137–141. doi: 10.1161/01.hyp.36.1.137
[6] NHS. High blood pressure (hypertension) – Prevention. 2019. Available at: https://www.nhs.uk/conditions/high-blood-pressure-hypertension/prevention/ (accessed February 2020)
[7] Puar THK, Mok Y, Debajyoti R et al. Secondary hypertension in adults. Singapore Med J 2016;57(5):228–232. doi: 10.11622/smedj.2016087
[8] Forouzanfar MH, Alexander L, Bachman VFet al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386(10010):2287–2323. doi: 10.1016/S0140-6736(15)00128-2
[9] National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management management. NICE Guidance [NG136]. 2019. Available at: www.nice.org.uk/guidance/ng136 (accessed February 2020)
[10] QRISK3. 2019. Available at: https://www.qrisk.org/ (accessed February 2020)
[11] Bacon SL, Sherwood A, Hinderliter A & Blumenthal JA. Effects of exercise, diet and weight loss on high blood pressure. Sports Med 2004;34(5):307–316. doi: 10.2165/00007256-200434050-00003
[12] Department of Health. Salt reduction – onwards and downwards! 2017. Available at: https://webarchive.nationalarchives.gov.uk/20180201175801/https://responsibilitydeal.dh.gov.uk/salt-reduction-onwards-and-downwards/ (accessed February 2020)
[13] Blood Pressure UK. Blood Pressure: drink less alcohol to avoid high blood pressure. 2017. Available at: http://www.bloodpressureuk.org/bloodpressureandyou/yourlifestyle/eatingwell/alcohol (accessed February 2020)
[14] NHS. The Eatwell Guide. 2019. Available at: https://www.nhs.uk/live-well/eat-well/the-eatwell-guide/ (accessed February 2020)
[15] Drinkaware. Calories in alcohol. 2019. Available at: https://www.drinkaware.co.uk/alcohol-facts/health-effects-of-alcohol/calories/calories-in-alcohol/ (accessed February 2020)
[16] Public Health England. Improving health literacy to reduce health inequalities. 2015. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/460710/4b_health_literacy-briefing.pdf (accessed February 2020)
[17] Google Play. Change4Life Food Scanner – Apps on Google Play. 2020. Available at: https://play.google.com/store/apps/details?id=com.phe.c4lfoodsmart&hl=en_GB (accessed February 2020)
[18] Apple. ‎Change4Life Food Scanner on the App Store. 2020. Available at: https://apps.apple.com/gb/app/change4life-be-food-smart/id1182946415 (accessed February 2020)
[19] Public Health England. Getting every adult active every day. Health Matters. 2019. Available at: https://www.gov.uk/government/publications/health-matters-getting-every-adult-active-every-day/health-matters-getting-every-adult-active-every-day (accessed February 2020)
[20] NHS Inform. Types of exercise. 2019. Available at: https://www.nhsinform.scot/healthy-living/keeping-active/getting-started/types-of-exercise (accessed February 2020)
[21] NHS. Start the NHS weight loss plan. 2019. Available at: https://www.nhs.uk/live-well/healthy-weight/start-the-nhs-weight-loss-plan/ (accessed February 2020)
[22] Apple. MyFitnessPal. Calorie Counter. 2019. Available at: https://apps.apple.com/us/app/myfitnesspal/id341232718 (accessed February 2020)
[23] Google Play. MyFitnessPal. Calorie Counter. 2019. Available at: https://play.google.com/store/apps/details?id=com.myfitnesspal.android&hl=en_GB (accessed February 2020)
[24] Pharmaceutical Services Negotiating Committee. Public Health (Promotion of Healthy Lifestyles). 2019. Available at: https://psnc.org.uk/services-commissioning/essential-services/public-health/ (accessed February 2020)
[25] National Institute for Health and Care Excellence. Behaviour change: general approaches. Public Health Guideline [PH6]. 2007. Available at: https://www.nice.org.uk/guidance/ph6/chapter/1-Public-health-need-and-practice (accessed February 2020)
[26] Prochaska JO & Velicer WF. The transtheoretical model of health behavior change. Am J Heal Promot 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38
[27] Boston University School of Public Health. The transtheoretical model (Stages of Change). 2018. Available at: http://sphweb.bumc.bu.edu/otlt/MPH-Modules/SB/BehavioralChangeTheories/BehavioralChangeTheories6.html#headingtaglink_1 (accessed February 2020)
[28] Donovan GR & Paudyal V. England’s Healthy Living Pharmacy (HLP) initiative: facilitating the engagement of pharmacy support staff in public health. Res Soc Adm Pharm 2016;12(2):281–292. doi: 10.1016/j.sapharm.2015.05.010


