Wes Mountain/The Pharmaceutical Journal
By the end of this article, you should be able to:
- Understand the role of formulae, equations, conversion charts and algorithms when calculating required dosage;
- Apply the use of formulae to clinical practice;
- Follow provided instructions and account for patient-specific factors when using provided formulae.
Introduction
Healthcare professionals — particularly pharmacists — frequently rely on a variety of equations, conversion charts, algorithms and formulae to determine correct drug dosages, concentrations and infusion rates. These evidence-based tools help tailor treatments to individual patient requirements by considering factors such as weight, age, renal function and disease state.
Some of these approaches, such as the Cockcroft-Gault equation for estimating renal function, may be integrated into electronic systems to partially automate the process and reduce the risk of errors. However, pharmacists are still expected to understand the physiological basis to these formulae. Exam questions involving formulas require you to demonstrate that you understand how to apply them in routine patient care. You should also familiarise yourself with the common pharmaceutical formulae used in clinical pharmacy practice. For some examples of common formulas, see Box. However, please note that this is not an exhaustive list.
Box: Selection of common formulas seen in pharmacy practice
Creatinine clearance (Cockcroft-Gault equation): The formula used for estimating renal function for drugs that are renally excreted.
Further information is available from the British National Formulary (BNF)1.
Pharmacokinetic formulas: A list of some useful pharmacokinetic equations2. Note that the formulas with logarithmic or exponential functions should be ignored as scientific calculators are not allowed in the General Pharmaceutical Council assessment. You could, however, be asked to calculate a missing parameter using a formula.
Opiate conversion tables: A list of common opiate conversions from the BNF3. Questions could be centred around dosage calculations for patients being converted from one or several opiates to another.
Benzodiazepine conversion tables: A list of common benzodiazepine doses converted to diazepam4. Questions could be centred around dosage calculations for patients being converted from one or several benzodiazepines to another.
Steroid conversion tables: A list of common corticosteroid conversions5. Questions could be centred around dosage calculations for patients being converted from one or several steroids to another.
Ganzoni formula: Determines the exact amount of iron to be given to patients parenterally6.
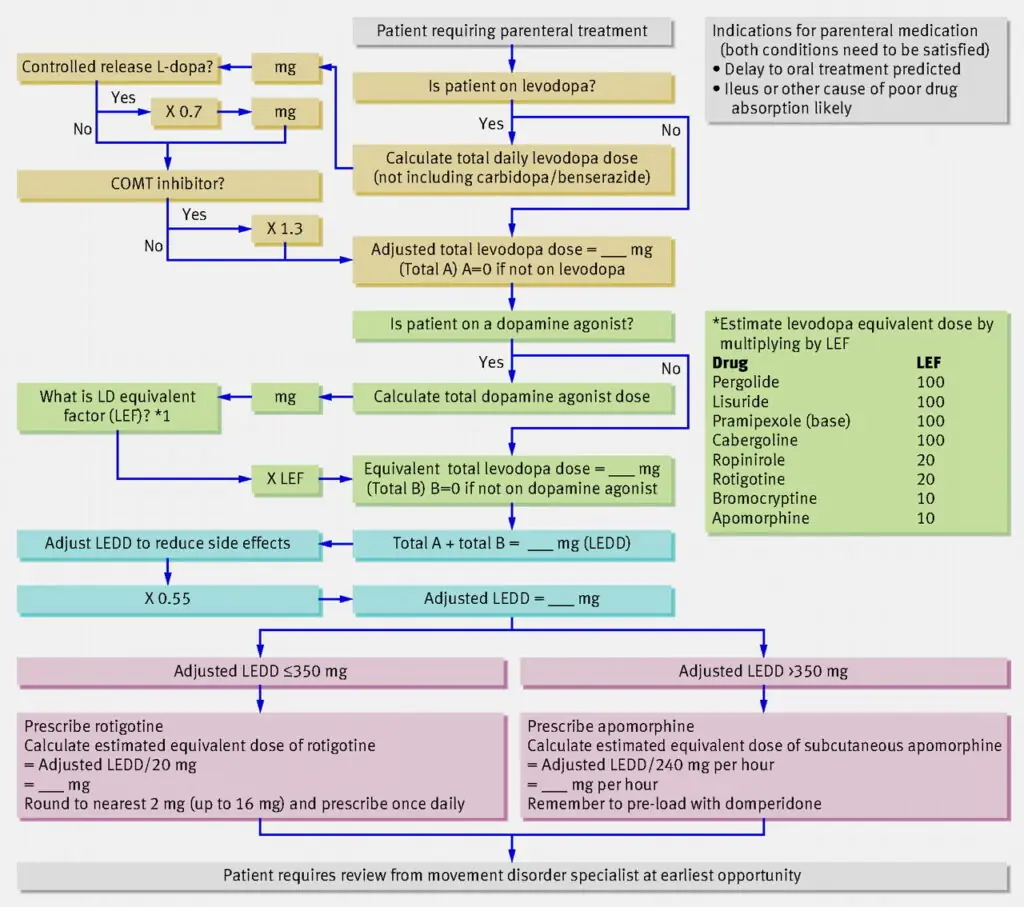
Parkinson’s disease medicines conversion chart: A step-by-step guide for converting Parkinson’s disease oral medications to a Rotigotine (Neupro; UCB) patch7.
Example question
A 60-year-old man with advanced Parkinson’s disease is unable to take his oral medications by mouth. You have been tasked to convert all his usual Parkinson’s disease medications to an equivalent Rotigotine (Neupro; UCB) patch. He is currently taking:
- Madopar (50mg Levodopa + 12.5mg Benserazide) capsules 1QDS;
- Entacapone 90mg tab 1OD;
- Ropinirole 1mg tab 1TDS.
Calculate the daily dose in mg for Rotigotine for this patient. Give your answer to the nearest 2mg, and use the resource provided.
(Note: Rotigotine patch is available as Neupro 1mg, 2mg, 3mg, 4mg, 6mg and 8mg. The patient can use more than one patch if necessary).
Figure: Algorithm for estimating parenteral doses of drugs for Parkinson’s disease
Comments and explanations
The above question looks complicated at first glance; however, it is not if you take a few moments to study it carefully. This question requires you to correctly follow the instructions on the algorithm and follow it through based on the information available to you. At the end, you are required to round your answer to the nearest 2mg, and you have been informed that multiple patches can be used to provide the required dose. We have broken the task down into the following steps.
Step one
Calculate the daily levodopa dose.
Daily levodopa dose = 50mg x 4 = 200mg per day.
You can disregard the patient’s prescription for carbidopa or benserazide and just focus on the levodopa dose. Carbidopa and benserazide are included in the formulation to enhance the effectiveness of levodopa by inhibiting decarboxylase inhibitors and do not contribute directly to replenishing dopamine in the brain.
Step two
Make adjustments based on whether levodopa is controlled release (CR).
Check if levodopa is CR or not. If it is CR, you would be required to multiply the daily levodopa dose x 0.7.
In this case, it is an immediate release preparation, so no adjustment is necessary, and you can move to the next line of the algorithm.
Step three
Make further adjustments based on whether the patient is taking a COMT inhibitor or not.
In this case, prior knowledge of drug classes is helpful. You need to know examples of COMT inhibitors, such as entacapone and tolcapone.
Entacapone is a COMT inhibitor, so multiply the levodopa daily dose by 1.3, as depicted in the algorithm.
200mg x 1.3 = 260mg
This figure becomes the adjusted levodopa dose (A) in the algorithm.
Step four
Make further adjustments based on whether the patient is taking a dopamine agonist.
You are required to know examples of dopamine agonists (e.g. pramipexole, ropinirole, bromocriptine, cabergoline or pergolide). In the question scenario, the patient is taking the dopamine agonist ropinirole.
According to the algorithm, you next need to calculate the daily dose of ropinirole and use the levodopa equivalent dose conversion factor (LEF) tables to convert it to the levodopa equivalent dose.
For ropinirole, the prescription information provided by the scenario is 1mg TDS, which means 1mg given three times per day or a daily dose of 3mg.
The LEF for ropinirole provided in the table is 20, so the levodopa equivalent daily dose (LEDD) (B) = 20 x 3mg = 60mg.
Step five
Calculate the total LEDD.
This is simply the LEDD of levodopa + the LEDD of ropinirole
= (A) + (B) = 260mg + 60mg
= 320mg
Step six
Make any necessary calculations adjustments to reduce side effects.
According to the algorithm, you are required to multiply the final dose by 0.55.
LEDD = [(A) + (B)] x 0.55]
= 320 x 0.55
= 176mg
Step seven
Calculate the strength of the Rotigotine patch needed, depending on whether LEDD is ≤ to 350mg or >350mg.
From step six, we know that LEDD is less than 350mg, so the required Rotigotine patch strength is 176mg/20 = 8.8mg.
Finally, this needs to be rounded to the nearest 2mg giving a final answer of 8mg.
Conclusion
From the example question above, it is important to be familiar with the various conversion charts and formulae used in calculating doses. You need to practice with these resources so that there are no surprises in the General Pharmaceutical Council exam. Finally, carefully scrutinise the information given in the resource so that you are selecting the relevant information.
Disclaimer and acknowledgements
The views in this article are those of the authors and do not represent the views of any organisations they are associated with. The questions and explanations presented here are for educational purposes only and do not replace your training, knowledge and application of professional judgement as a pharmacist or trainee pharmacist. The example questions used in this article and the answers provided are for educational purposes and should not be translated to represent what would happen in real practice.
All practice questions were reproduced with kind permission provided by Focus Pre-Reg Revision.
- 1.Prescribing in renal impairment. The National Institute for Health and Care Excellence. https://bnf.nice.org.uk/medicines-guidance/prescribing-in-renal-impairment/
- 2.Useful pharmacokinetic equations. University of Florida College of Pharmacy . https://pharmacy.ufl.edu/files/2013/01/5127-28-equations.pdf
- 3.Prescribing in palliative care. The National Institute for Health and Care Excellence. https://bnf.nice.org.uk/medicines-guidance/prescribing-in-palliative-care/
- 4.Hypnotics and anxiolytics. The National Institute for Health and Care Excellence . https://bnf.nice.org.uk/treatment-summaries/hypnotics-and-anxiolytics/
- 5.Glucocorticoid therapy. The National Institute for Health and Care Excellence . https://bnf.nice.org.uk/treatment-summaries/glucocorticoid-therapy/
- 6.Monofer 100mg/ml solution for injection/infusion. EMC. April 29, 2025. https://www.medicines.org.uk/emc/product/5676/smpc
- 7.Brennan K, Genever R. Managing Parkinson’s disease during surgery. BMJ. 2010;341(nov01 2):c5718-c5718. doi:10.1136/bmj.c5718