
Sheila Terry/ Science Photo Library
This content was published in 2010. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
Hypertension is a major but modifiable contributory factor in cardiovascular diseases such as stroke and coronary heart disease. The main driver for the close monitoring and management of hypertension is the reduction in cardiovascular morbidity and mortality.
What are the important numbers?
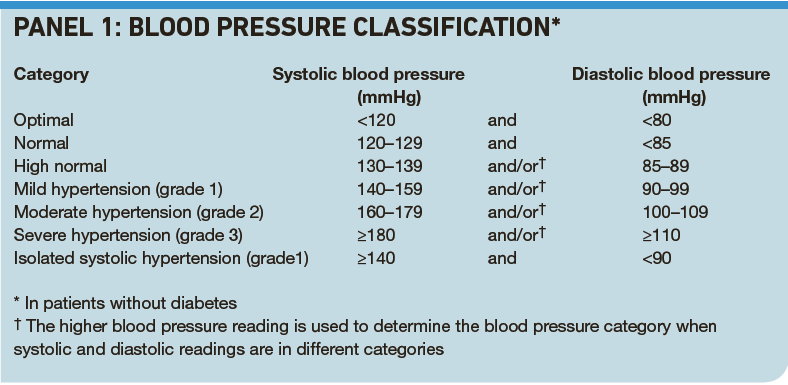
Hypertension is defined as persistent raised blood pressure above 140/90mmHg. Panel 1 shows the classification of blood pressure in terms of numbers, as accepted by the British Hypertension Society, the European Society of Hypertension and the European Society of Cardiology. This does not take into account the rise in blood pressure seen with increasing age, but current treatment targets are not generally based on the age of the patient.
Hypertension should be confirmed by asking the patient to return for at least two subsequent measurements under quiet and calm conditions. The period over which this is confirmed will depend on the initial blood pressure readings and, in most cases, whether the patient has cardiovascular complications. For example, an initial reading of 180–219mmHg systolic or 110–119mmHg diastolic should be confirmed within two weeks. In comparison, an initial reading of 140–159mmHg systolic or 90–99mmHg diastolic in a patient with diabetes requires confirmation within 12 weeks.1
In the diagnosis of hypertension it is also necessary to exclude “white coat” hypertension —where blood pressure readings are artificially raised in the clinic. In addition, patients sometimes claim to have lower readings (using a home blood pressure monitor) and this can complicate matters.
Reflect
- What are the advantages and disadvantages of monitoring blood pressure at home?
- What extent of blood pressure lowering can be expected through lifestyle modifications?
- What are the thresholds for initiating antihypertensive treatment?
Before reading on, think about how this article may help you to do your job better.
Thresholds and targets
Suggested thresholds and targets for treatment are outlined in the British National Formulary. They are based on blood pressure readings in a clinical setting rather than readings taken at home.
The decision to initiate drug treatment will also be influenced by factors such as comorbidities (eg, cardiovascular complications and diabetes) and 10-year cardiovascular risk. Unless blood pressure is over 179mmHg systolic or 109mmHg diastolic, patients with no complications may first be advised to make lifestyle changes and be reassessed before drug treatment is considered. Those with complications tend to be given drug treatment earlier.
The aim of treatment is to get blood pressure down to below140/90mmHg.1 (For patients with diabetes or atherosclerotic cardiovascular disease the targets are lower and the aim is to maintain systolic pressure below 130 mmHg and diastolic pressure below 80mmHg.1)
The Panel also highlights the need to look out for isolated systolic or diastolic hypertension. For example, grade 2 isolated systolic hypertension, defined as a systolic pressure greater than 160mmHg and a diastolic pressure of less than 90mmHg, is associated with an increased cardiovascular risk, particularly in those aged over 60 years. If grade 2 isolated systolic hypertension persists over three to six months after attempting appropriate lifestyle interventions, it should be treated in those aged over 60 years. ISH is not as common in patients under the age of 60 years but if a patient is at increased risk of cardiovascular disease and has persistent raised systolic pressure, treatment should be considered.
Some patients may have only a raised diastolic pressure. A patient with a diastolic pressure of over 85mmHg would be regarded as being in the normal to high category and would invite closer monitoring.
Measuring blood pressure
The accurate measurement of blood pressure is important for effective diagnosis and treatment. The traditional method of measuring blood pressure is the auscultatory (listening) method. This involves the use of a stethoscope and sphygmomanometer by a trained healthcare professional. An inflatable cuff is placed around the upper arm at approximately the same height as the heart and attached to a mercury or aneroid (clock face) manometer. The mercury manometer is considered to be more accurate because it is based on a height of a column of mercury. An aneroid device, although more portable, is highly sensitive to mechanical strain and is more easily damaged by impact, so accuracy can decrease. It is also subject to calibration drift errors.
An appropriately-sized cuff is fitted around the upper arm and inflated manually with a rubber bulb until the artery is completely occluded. The stethoscope is then used to listen to the brachial artery at the elbow while, at the same time, slowly releasing the pressure in the cuff. As the pressure drops to a level that is equivalent to the patient’s systolic blood pressure the first Korotkoff sound — named after the Russian physician — is heard. This sound can be described as a “whooshing” or “snapping” and is heard when the pressure in the cuff reaches the pressure produced in the artery during systole. The characteristic sound is caused as the blood flows in spurts as the pressure in the cuff drops below the pressure in the artery, resulting in turbulence.
Korotkoff described five types of sound as the pressure is slowly released from the cuff. The fourth, which is at pressures within 10mmHg above the diastolic pressure, is described as “thumping” or “muting”. The fifth “sound” is silence as the cuff pressure drops below the diastolic arterial pressure. The diastolic pressure reading is taken at this point.
Not all GPs and nurses use mercury manometers and, according to a member of the British Hypertension Society blood pressure device monitoring group, the number of readings that GPs and nurses have to do make it impractical not to use an automated device.2 (Automated devices detect oscillation in the arterial wall as blood flows through at different pressures.3) However, a recent US study found that automated BP monitors give readings an average of 2mmHg lower than mercury manometers, putting some patients at risk. The disparity in readings was found to be greatest in patients over 65 years of age.2
Healthcare professionals trained to measure blood pressure should have their performance reviewed periodically.
Systolic versus diastolic
Current guidelines and clinical practice are based on the measurement and treatment of both systolic and diastolic blood pressure.
However, due to the increasing evidence of the importance of systolic hypertension in terms of risk, it has been suggested that diastolic blood pressure need not be measured.4 There appears to be some debate about the risks associated with increased diastolic hypertension whereas the Multiple Risk Intervention Trial found that for any level of diastolic blood pressure, the systolic blood pressure was the major determinant for cardiovascular risk.5
One reason diastolic pressure is not ignored is that pulse pressure, which is defined as the difference between systolic and diastolic blood pressure, has been highlighted as an independent predictor of cardiovascular risk.6 The use of pulse pressure as an indicator of cardiovascular risk is a possible way forward in the complex debate on the relative importance of systolic over diastolic pressure. In the meantime, however, national guidelines and treatment targets are based on both readings.
Issues with monitoring at home
The most recent National Institute for health and Clinical Excellence guidelines state that the routine use of home monitoring devices or automated ambulatory monitoring devices is not recommended.7 This is because the value of such equipment in primary care has not been established and NICE has recommended that this is an area of focus for further research.
In practice, however, healthcare professionals may encourage the use of a home blood pressure monitor so that patients can monitor their blood pressure between clinic appointments. The potential advantages of home blood pressure monitoring include:
- A more general overview of a patient’s blood pressure everyday life
- An indication of whether the blood pressure is higher or lower than in the clinic
- A means of observing if medication and lifestyle interventions are having an impact on blood pressure readings
On the negative side, the use of a home blood pressure monitor can cause anxiety in some patients, which can lead to the obsessive taking of frequent readings. It is important to establish with individual patients whether monitoring at home either reassures or is a form of additional stress.
In general, it is not necessary to take home readings more than once a week. Patients with an irregular heart rate may not be able to achieve an accurate reading with an electronic device. Patients with problems bending or moving their arms may also have problems using the cuff and home monitoring may be unsuitable.
Home blood pressure monitors are usually supplied with a standard cuff and if the person’s upper arm circumference is outside the standard range, he or she will need to buy a larger or smaller cuff because cuffs that are too large or small give inaccurate readings. The bladder of the cuff should cover at least 80 per cent of the circumference of the arm but no more than 100 per cent. The cuff should be tight but not too tight. (Two fingers should be inserted between the skin and the cuff to check for tightness before a measurement.)
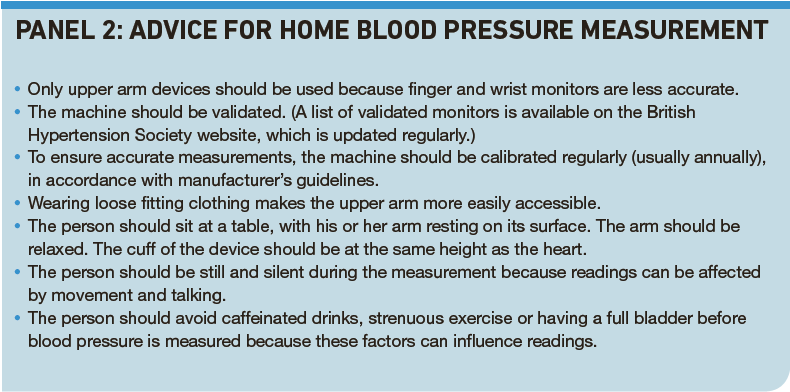
Further advice associated with home blood pressure measurement can be found in Panel 2.
Ambulatory monitoring
Ambulatory blood pressure monitoring uses an automatic device to obtain readings over 24 hours while a patient is in his or her normal environment. It is sometimes used in patients who have borderline clinic readings or poorly controlled hypertension.8 Readings can be taken every 30 minutes and every hour during the night. It should be noted that the numbers from ambulatory readings are not equivalent to clinic readings in terms of thresholds and targets.
Frequency of monitoring
In practice, the frequency of blood pressure monitoring is usually every five years in healthy individuals.
One of the indicators in the Quality and Outcomes Framework for the general medical services contract is a record of the percentage of patients with hypertension in whom there is a record of their blood pressure in the previous nine months. There are no specific British Hypertension Society Guidelines on the frequency of follow up in patients with hypertension but there is an assumption that this will be approximately every six months and the audit standard is based on nine months. The frequency of follow up in patients on antihypertensive medicines will depend on factors such as the severity of the hypertension, the complexity of the treatment regimen, patient compliance and the need for non-pharmacological advice. If the patient has uncontrolled hypertension the frequency of monitoring is usually every four to eight weeks.
Lifestyle advice: is it worth it?
Pharmacological intervention is the main way to treat hypertension, which continues to be viewed as a condition that is under-treated. However, lifestyle modifications can also be useful. There are clear links between obesity and salt and alcohol intake in the development of hypertension.
An important question for the healthcare professional and the hypertensive patient is: how significant are lifestyle modifications in the reduction of blood pressure readings? This question also overlaps with the question surrounding overall cardiovascular risk. For example, there is no strong direct link between smoking and blood pressure but smoking cessation is the most important lifestyle modification for the reduction of overall cardiovascular risk.
The reductions, in terms of mmHg, resulting from lifestyle changes (summarised in Panel 3 using data from NICE guidelines) may appear modest. However, it should be appreciated that the overall picture is complex in terms of additive effects between different factors and variability between individuals. For example, about 25 per cent of patients receiving multiple lifestyle interventions were estimated to achieve a reduction in systolic blood pressure of 10mmHg systolic or more in the short term, up to a year.

Pharmacists should note, however, that NICE concluded that patient education about lifestyle on its own is unlikely to be effective. Any lifestyle advice needs to be supplemented with appropriate written or audiovisual materials.
Cardiovascular risk
When an increase in blood pressure persists and there is no previous history of cardiovascular disease the patient should be invited to discuss the need to assess their cardiovascular risk formally. Age is the main determinant of risk for cardiovascular disease —the condition mainly affects people older than 50 years.
Although it has been established that women have lower coronary heart disease rates than men, the disease is the leading cause of mortality in women as well as men in most industrialised countries. This suggests that interventions by healthcare professionals need to be targeted at both sexes.
The three modifiable risk factors that make a major contribution to CVD risk are smoking, raised blood pressure and raised cholesterol. These factors are present in 80 per cent of all cases of premature coronary heart disease. Initially, patients should be prioritised on the basis of an estimate of their CVD risk, based on information recorded in their medical record, before a full formal assessment is made.
Debate over tools
A cardiovascular risk assessment tool can be useful in terms of prognosis. Assessment tools provide an indication of percentage risk of cardiovascular disease over a 10-year period. This is usually undertaken by inputting information, such as age, sex, systolic blood pressure, total cholesterol, high density lipoprotein cholesterol, smoking status and other factors, into a computer programme.
Most risk assessment models are based on information derived from the Framingham Heart Study, which involved a cohort of over 5,000 men and women aged between 30 and 62 years of age from Framingham, Massachusetts. The subjects were followed from 1971 in order to assess the determinants of cardiovascular disease. Major criticisms of this model include poor validation in the UK and lack of application to ethnic minorities and younger populations.
The University of Nottingham developed the QRISK CVD risk assessment tool to address some of these issues and provide a more UK-centred tool. This is updated annually as the population characteristics change and comparison data improves. In Scotland, the ASSIGN tool was developed by Dundee University and took into account factors suited to Scotland, such as social deprivation. There is significant debate surrounding both the choice and the use of these tools. Until recently, the Framingham risk calculator was the model of choice. However, this year the NICE guidance executive agreed to withdraw the recommendation that the Framingham risk equation should be the tool of choice for the assessment of CVD risk.9 The updated NICE guidance states that other risk assessment tools can be used and it is up to the individual clinician.
Some would view the development of a specific UK-wide, standardised CVD risk tool as a positive move. An alternative view is that all risk equations are inaccurate to some degree and need constant refinement. The main issue is that they are applied consistently. The cardiovascular risk prediction charts at the back of the BNF are based on the Joint British Societies guidelines on prevention of cardiovascular disease in clinical practice.10 It should be noted that these differ from the estimation of cardiovascular risk in the latest NICE clinical guideline.
Do you need to revise your knowledge of hypertension treatment? A second CPD article, to be published online on 16 October, will summarise the current treatment recommendations. It will contain practice points, a suggested answer to the scenario in Panel 4 and references. Our “Check your learning” tool will be available once this second article is published.
CPD articles are commissioned by The Pharmaceutical Journal and are not peer reviewed.


