The human body contains around 2g of zinc. Approximately 95 per cent of this zinc is found within cells. About 57 percent of the body pool is stored in skeletal muscle, 29 per cent in bone and 6 per cent in skin, but zinc is found in all body tissues and fluids.
Functions of zinc
Zinc is critical for the function of about 60 enzymes in humans. It is a co-factor in a
range of biochemical processes, including the synthesis of deoxyribonucleic acid, ribonucleic acid and proteins. Zinc is required for the hepatic synthesis of retinol binding protein, the protein involved in transporting vitamin A. Without adequate zinc, symptoms of vitamin A deficiency can appear even if vitamin A supplements are taken.
Zinc also acts as an antioxidant, restricting endogenous free radical production and acting as a structural component of the extracellular antioxidant enzyme, superoxide dismutase. It also helps to protect against depletion of vitamin E and maintains tissue concentrations of metallothionein, a possible scavenger of free radicals.
Other biochemical processes that require zinc include carbohydrate metabolism, protein digestion, blood clotting and bone metabolism.
Structural and regulatory role
Zinc plays a role in the structure of biomembranes. A reduction in the concentration of zinc in these membranes results in increased susceptibility to oxidative damage and alteration in specific transport systems and receptor sites and these may underlie some of the disorders associated with zinc deficiency.
Zinc is also important for the structure of some proteins, known as “zinc finger proteins”. Polypeptides that are too small to fold by themselves can do so when stabilised by bound zinc. Zinc finger proteins regulate gene expression by acting as transcription factors (binding to DNA and influencing the transcription of specific genes). Prostaglandins and nuclear receptors for steroids are also zinc finger proteins.
Zinc has regulatory roles in cell signalling and influences nerve impulse transmission. It also plays a role in apoptosis, a critical cellular regulatory process with implications for growth and development, as well as a number of chronic diseases.
Panel 1 describes current issues involving zinc.
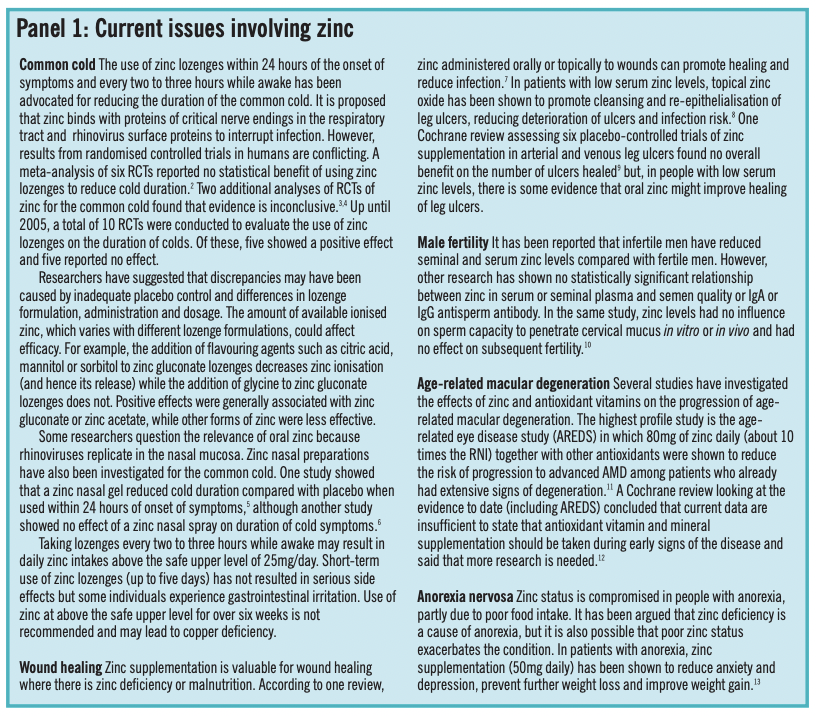
Immune function
Zinc is involved in the function of cells contributing to non-specific immunity, such as neutrophils and natural killer cells. Zinc also plays a role in T-lymphocyte function and in the development of acquired immunity.1
Reproduction
Zinc is essential for the metabolism of reproductive hormones (eg, androgens, oestrogens and progesterone), ovulation, testicular function, the formation and maturation of sperm, fertilisation and the health of the fetus and mother during pregnancy. Deficiency of zinc during early development can be teratogenic.
In men, the prostate gland has the highest concentration of zinc of any organ in the body.
Vision
Present in high concentrations in the eye, particularly in the retina and choroid, zinc plays a role in the maintenance of vision.
Sources of zinc
Foods vary widely in their zinc content. Concentrations can range from 0.02mg/100g for egg white to 1mg/100g for chicken and 75mg/100g oysters. Shellfish and red meats are good sources of zinc. The bioavailability of zinc is high in these foods because of the relative absence of compounds that inhibit zinc absorption (eg, phytic acid) and the presence of amino acids, such as cysteine and methionine, that enhance absorption.
Wholegrain cereals are relatively rich in zinc but nearly 80 per cent of it can be lost in the wheat milling process. Nuts and legumes are also good sources of zinc. The zinc concentration in plant sources might be enhanced if plants are grown in zinc-rich soil. However, zinc in plants is less bioavailable than that in animal sources because of the high content of phytic acid. Fermentation of wholemeal bread reduces the phytic acid content and significantly improves zinc absorption. Leavened breads, therefore, have more bioavailable zinc than unleavened breads. Techniques used for cooking breakfast cereals seem to inhibit degradation of phytic acid in the gut and results in less efficient absorption of zinc.
Supplements
Many over-the-counter multivitamin and mineral supplements contain zinc. Those sold in pharmacies commonly contain a daily dose of 5–15mg of elemental zinc. Elemental zinc is also available as single supplements in the form of zinc acetate (30 percent), zinc amino acid chelate (10 percent), zinc gluconate (14 percent), zinc orotate (17 percent), zinc picolinate (35 percent) and zinc sulphate (23 percent).
Human requirements
Zinc requirements are based on a number of different indicators because a sensitive indicator of zinc status is not available. In the UK, these indicators include measurement of zinc losses in faeces, urine, skin, hair and menstrual blood or semen during metabolic studies of zinc deprivation. Turnover time of radiolabelled endogenous zinc pools and deduction from metabolic studies of patients receiving total parenteral nutrition (TPN) are also used.
Minimal zinc losses have been estimated to be 2.2mg/day in men and 1.6mg/day in women. Based on 30 percent absorptive efficiency, these figures correspond to estimated average requirements (EARs) of 7.3mg/day in men and 5.5mg/day in women. The reference nutrient intakes (RNIs) are 9.5mg/day for men and 7.0mg/day for women while lower reference nutrient intakes (LRNIs) are 5.5mg/day for men and 4.0mg/day for women.
Mean intake of zinc in the UK is 10.2mg/day in men and 7.4mg/day in women. Overall intakes are, therefore, higher than the RNI. However, 43 per cent of men and 45 per cent of women fail to achieve the RNI. In addition, 4 per cent of both men and women fail to achieve the LRNI, a level that fulfils the requirements of relatively few people and below which deficiency is likely to occur.14
The EU recommended daily amount (RDA) for zinc is 15mg.This is judged to be sufficient for most people. However, this is an approximate figure, based on the requirements of adult men, and does not take into account the needs of other population groups.
Zinc deficiency
Serious zinc deficiency is rare in the UK, but inadequate intake and marginal deficiency are not uncommon. Clinical manifestations of severe zinc deficiency include growth retardation, delayed sexual maturation, hypogonadism, diarrhoea, alopecia, skin lesions and nail dystrophy. Immune system deficiencies and susceptibility to infection, behavioural disturbances, impaired taste, delayed wound healing, impaired appetite and food intake may also indicate zinc deficiency.Eye lesions, photophobia and lack of adaptation to the dark can occur.
Mild or marginal deficiency is more difficult to characterise. However, there is likely to be a graded response to progressive degrees of deficiency. Thus, while growth may cease in severe deficiency, growth may slow in mild deficiency. Maternal zinc deficiency before and during pregnancy is associated with intrauterine growth retardation, low birthweight, teratogenicity and increased risk of miscarriage and stillbirths. Zinc deficiency is also associated with increased morbidity, pre-eclampsia and toxaemia.
There is no reliable clinical test to determine zinc deficiency. Serum or plasma zinc on its own is neither sensitive nor specific.This is because zinc is primarily found intracellularly. The small proportion in the plasma is bound to plasma proteins. Plasma zinc is influenced by conditions unrelated to zinc status (eg, infection and inflammation) and does not fluctuate with modest changes in dietary zinc intake. Until better markers are developed, an estimate of zinc status can be made from a combination of dietary zinc intake and plasma zinc concentration. If usual intake is below the EAR and plasma zinc is low, poor zinc status can be considered possible.
Zinc deficiency can result from inadequate dietary intake, poor absorption or increased loss. Vegetarians are at risk because the high levels of phytic acid in plant foods reduce the absorption of zinc. Some patients receiving TPN have been reported to develop symptoms of zinc deficiency. Zinc deficiency can also develop as a result of diseases, such as sickle cell anaemia, Wilson’s disease (see Panel 2) and cirrhosis, or recurrent infections. It is also associated with anorexia nervosa and alcoholism.
Malabsorption syndromes such as coeliac disease or chronic diarrhoea and inflammatory bowel conditions, such as Crohn’s disease and ulcerative colitis, can lead to increased zinc losses and zinc deficiency in this way. Other conditions of increased zinc loss include severe burns, major surgery and HIV or AIDS.
Diabetes, particularly if poorly controlled, is associated with increased zinc loss in urine, reduced absorption and decreased total body zinc. However, the role of zinc and the influence of zinc deficiency in diabetes is currently unclear. It has been suggested that zinc deficiency may exacerbate destruction of islet cells in type 1 diabetes and adversely affect synthesis, storage and secretion of insulin — processes that require zinc. Zinc supplementation is sometimes used in diabetes to try to prevent deficiency, but it is not yet known whether this is of benefit in preventing or treating diabetes.
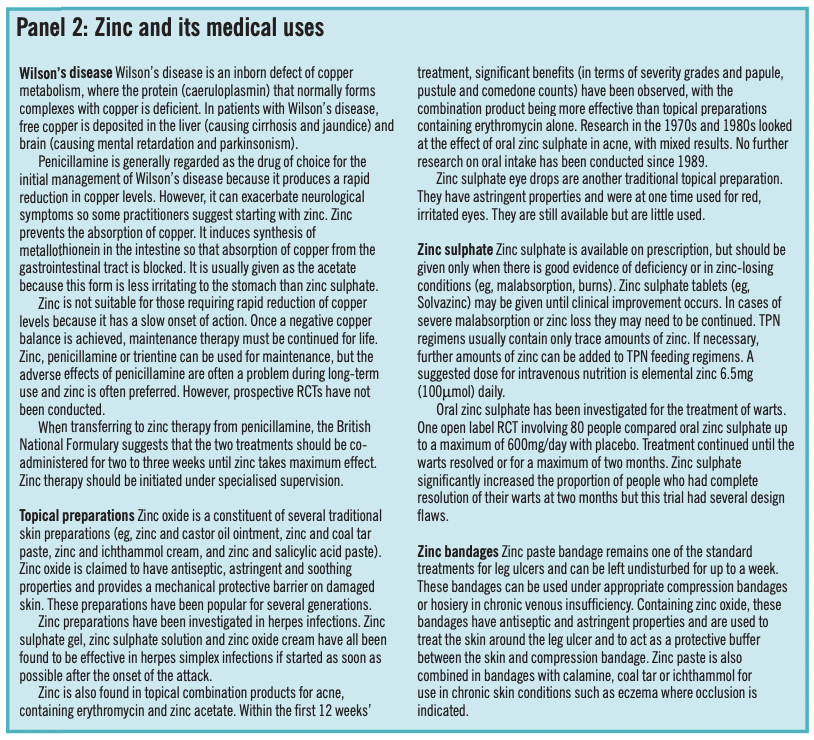
Interactions and toxicity
Zinc can interact with a number of other minerals, foods and medicines. High intakes of dietary calcium and calcium supplements have been shown to impair zinc absorption in some studies, but not others. Supplemental iron at prescription doses reduces zinc absorption. Long-term folate supplementation may also reduce zinc levels. Thiazides, loop diuretics and, possibly, angiotensin converting enzyme inhibitors increase urinary excretion of zinc and the possibility of zinc deficiency during long-term use of these drugs should be considered.
High zinc intake (100–150mg/day) reduces copper absorption by competition. Zinc forms complexes with tetracyclines, quinolones and also non-steroidal anti-inflammatory drugs and doses should be separated by two hours. Acute zinc toxicity is rare, but typical signs include epigastric pain, diarrhoea, nausea, vomiting, bad taste and discomfort in the mouth and throat. Doses above 200mg/day are typically emetic and may be vomited before absorption can occur.The major consequence of chronic long-term ingestion of excessive zinc supplements (ie, 100–150mg zinc/day) is induction of a secondary copper deficiency with anaemia and neutropenia. Impaired immune function and an adverse effect on the ratio of low-density lipoprotein to high-density lipoprotein cholesterol can also occur.
The UK Food Standard Agency’s Expert Group on Vitamins and Minerals has set a safe upper level for zinc from supplements alone of 25mg daily.This level applies to long-term use of supplements in the normal healthy population. It does not apply to patients who receive zinc on prescription. Panel 2 discusses the medical uses of zinc.
References
- Shankar AH, Prasad AS. Zinc and immune function: the biological basis of altered resistance to infection. American Journal of Clinical Nutrition 1998;68:447S–63S.
- Jackson JL, Peterson C, Lesho E. A meta-analysis of zinc salts lozenges and the common cold. Archives of Internal Medicine 1997;157:2373–6.
- Jackson JL, Lesho E, Peterson C. Zinc and common cold: a meta-analysis revisited. Journal of Nutrition 2000;130:1512S–15S.
- Marshall I. Zinc and the common cold. Cochrane Database Systematic Review 2000;2:CD001364.
- Hirt M, Nobel S, Barron E. Zinc nasal gel for the treatment of common cold symptoms: a double-blind, placebo-controlled trial. Ear Nose and Throat Journal 2000;79:778–80.
- Turner RB. Ineffectiveness of intranasal zinc gluconate for prevention of experimental rhinovirus colds. Clinical Infectious Diseases 2001;33:1865–70.
- Landsdown AB. Zinc in the healing wound. Lancet 1996;346;706–7.
- Agren MS. Studies in zinc wound healing. Acta DermatoVenereologica 1990;154 (Suppl):1–36.
- Wilkinson EA, Hawke CI. Oral zinc for arterial and venous leg ulcers. Cochrane Database Syst Rev 2000;2:CD001273.
- Eggert-Kruse W, Zwick EM, Batschulat K, Rohr G, Armbruster FP, Petzoldt D, et al. Are zinc levels in seminal plasma associated with seminal leukocytes and other determinants of semen quality? Fertility and Sterility 2002;77:260–9.
- Age related eye disease study research group. A randomised, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta-carotene, and zinc for age-related macular degeneration and vision loss. Archives of Ophthalmology 2001;119:1417–36.
- Evans JR. Antioxidant vitamin and mineral supplements for age-related macular degeneration. Cochrane Database Systematic Review 2002;2:CD000254.
- Safai Kutti S. Oral zinc supplementation in anorexia nervosa. Acta Psychiatrica Scandinavica 1990;361(Suppl);253–60.
- Henderson L, Gregory J, Swan G. The National Diet and Nutrition Survey: adults aged 19 to 64 years. A survey carried out on behalf of the Food Standards Agency and the Department of Health by the Social Security Division of the Office for National Statistics and Medical research Council Human Nutrition Research, 2003. Available at: www.food.gov.uk (accessed 14 February 2006).


