
Shutterstock.com
After reading this article, you should be able to:
- Explain what objective structured clinical examinations are;
- Feel confident that you know how to prepare for them.
The objective structured clinical examination (OSCE) has been a feature of medical school programmes since the 1970s. OSCEs were introduced to assess professional performance in practice within a safe environment, where neither the student or patient is at risk of harm. In an OSCE, clinical scenarios are simulated and the student responds as though they are a qualified healthcare professional.
Some students find OSCEs to be a stressful form of assessment. The student is exposed to the direct scrutiny of members of staff and simulated patients or healthcare professionals, and must find solutions to problems within a tight timeframe. However, students who are well prepared for OSCEs tend to be calmer and perform better.
The aim of this article is to explain what OSCEs involve and how to prepare for them. This article has been adapted from Pharmacy OSCEs, published by Pharmaceutical Press.
Pharmacy OSCEs is the only pharmacy-specific OSCE revision guide that covers the key competencies that will be tested. Written in a concise and accessible way, all types of situations are covered from responding to a specific symptom to solving calculations. Over 70 scenarios read like tasks at an OSCE station and are accompanied by:
- Learning objectives;
- Questions and answers;
- Feedback and revision points;
- Key references and further reading.
What topics are OSCEs likely to cover?
The topics likely to be assessed by OSCE are the ones that are challenging to test in other types of assessment. For example:
- Responding to symptoms;
- History taking;
- Skills and knowledge needed for prescribing;
- Counselling patients about prescription medicines;
- Communicating information relating to medicines to healthcare professionals, patients or carers;
- Record keeping;
- Problem solving (e.g. identifying drug interactions or interpreting laboratory data and recommending appropriate management);
- Dosage calculations;
- Advising on drug administration.
To prepare, spend time revising these areas:
- Patient assessment;
- Interpreting laboratory biochemical data;
- Monitoring requirements and understanding of results, such as the international normalised ratio;
- Simple dosage calculations, such as doses for children expressed as mg/kg or mg/m2;
- Basic pharmacokinetics — more complex formulae will be supplied during the exam, but clearance or volume of distribution might be considered common knowledge.
Familiarise yourself with the reference sources
Many reference sources will be available online or through your university. At a minimum, take some time to explore the following resources prior to the OSCE:
- Martindale: The Complete Drug Reference[1];
- Stockley’s Drug Interactions[2];
- British National Formulary (BNF)[3];
- BNF for Children[4];
- National Institute for Health and Care Excellence clinical knowledge summaries[5];
- Summaries of product characteristics (SmPCs).
Bookmark where particular information is located, so that you can look it up quickly if needed. Similarly, have a look through patient information leaflets and SmPCs (available on the Electronic Medicines Compendium). These materials follow a specific format and you will save time in the exam if you know exactly where to look.
If you are able to bring a copy of the BNF into the exam with you, spend time becoming familiar with the edition that you intend to take. Considerations include:
- Do you understand all the symbols? Remind yourself by looking through the abbreviations pages prior to the OSCEs;
- When looking at an individual citation for a drug, additional information may be included in the class citation;
- Familiarise yourself with the location of the ‘equivalent dosages’, as it is not always obvious. For example, equivalent dosages of morphine and diamorphine are not found at the beginning of ‘Opioid analgesics’, but within ‘Prescribing in palliative care’;
- The appendices in the BNF are an accessible source of information. Older editions have separate appendices for hepatic failure, renal failure, pregnancy and breastfeeding. Newer copies have this information within the main body of the book;
- The BNF highlights important information, such as warnings, by using a coloured box or different font. This is intended to draw the reader’s eye;
- Many drugs are used for multiple clinical indications and the treatment schedule may vary considerably — for example, look at the doses of cyproterone used to treat acne, male hypersexuality and malignant disease.
- Be careful to choose the most appropriate indication when using the index.
‘Bell ringers’
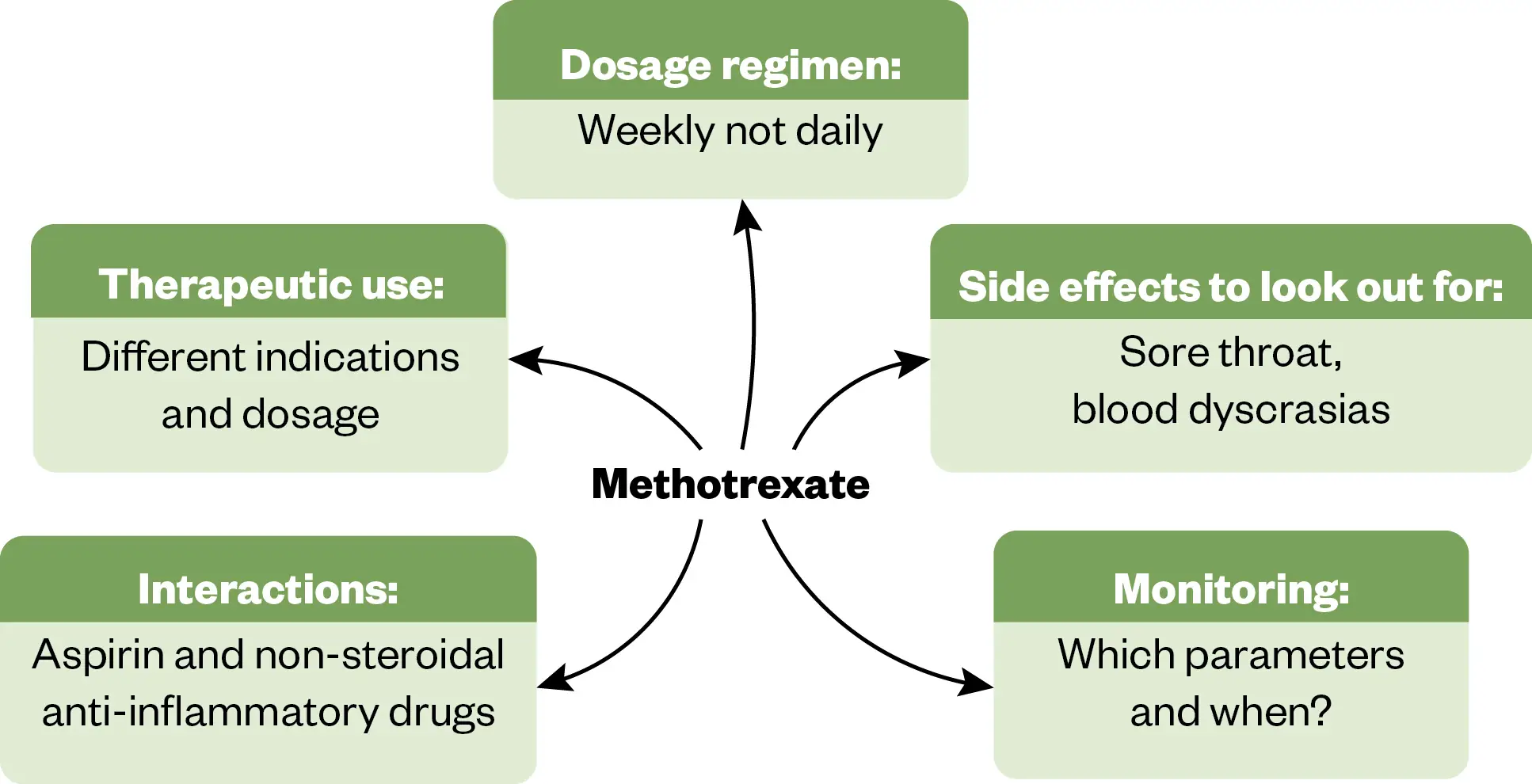
As you develop your clinical skills, you will identify some drugs that are difficult to use; for example, they may have narrow therapeutic indices, be enzyme inhibitors or inducers, need therapeutic drug monitoring or have serious adverse effects. These are the medicines most likely to appear in OSCEs because they are also most likely to cause problems in practice. These drugs could be called ‘bell ringers’, which is to say that when you encounter them, bells should start ringing in your head. You can probably think of a few immediately — digoxin, warfarin, methotrexate, carbamazepine and erythromycin.
It may be helpful to create revision aids for these drugs. An example is provided in Figure 1.
Practise your communication, consultation and counselling skills
If you do not have experience speaking to patients and healthcare professionals about medication-related issues, it is possible to practise these skills at home. Try explaining pharmacy scenarios to friends or family.
The Pharmaceutical Journal
This exercise is particularly useful for helping to understand the type of language to use with patients. Print out a patient information leaflet and try to explain how to use a device (such as an inhaler) to someone who has never used one, using a household prop. Your friends and family will certainly tell you if they do not understand. This method also works for complex dosage schemes, such as decreasing doses of steroid. Remember that, in the OSCE, the ‘patient’ may be a tutor, an actor or a member of the public from a voluntary organisation.
On the day of the OSCE
- Arrive in plenty of time. In many centres, OSCEs run as an automated circuit and latecomers will not be admitted;
- Remember to bring all necessary items. Your centre will tell you what you may bring, which may include a calculator and a copy of the BNF;
- Dress appropriately. There may be a dress code. Many students feel more confident when dressed as a professional would dress.
Approaching a new scenario
At each OSCE station, read the instructions carefully and try to avoid jumping to conclusions. This is particularly important with the ‘bell ringers’. It is easy, especially if you are nervous, not to consider all the possible options. Once you have a plan, decide if you need to look up any information. Students sometimes waste valuable time looking up information that they actually know. Once you have decided what you need to look up, decide which of the available reference sources is the most appropriate.
Remember that each scenario is a new start. Many students will dwell on previous scenarios that they found difficult to the detriment of their performance at further stations.
OSCEs differ from other types of assessment in that they test a student’s ability to communicate verbally. This means that there will be marks assigned to verbal communication. If appropriate, introduce yourself to the patient or healthcare professional. Finish each station by asking if they understand or if they have further questions. If you are given a patient’s name, use it. Try to maintain eye contact with the patient or examiner. There may be marks assigned for non-verbal communication.
Remember your mnemonics and apply them in their entirety. This is particularly important if you are nervous — it will stop you missing out vital questions.
If the scenario begins with the patient or healthcare professional speaking, listen carefully to what they have to say. Try not to start looking through your resources before they have finished speaking. If you are distracted, you may miss vital information, and it is also poor non-verbal communication.
Conclusion
OSCEs can seem intimidating and stressful, particularly as they are so different from other types of pharmacy assessments. It is vital is to practise and prepare beforehand; students who are well prepared for OSCEs usually feel calmer and perform better. Revise the material and areas most likely to come up in an OSCE and familiarise yourself with the reference sources you are going to use. Practice your consultation and communication skills, ideally with friends or family who are not as familiar with medicines and devices, so they can give you valuable feedback. On the day, plan to be early and remember to bring everything you’ll need. Stay calm, read the instructions, and listen to the patient and examiner. Good luck!
- 1Brayfield A, Cadart C. Martindale: The Complete Drug Reference. Pharmaceutical Press. 2024. https://www.pharmaceuticalpress.com/products/martindale-the-complete-drug-reference/ (accessed July 2024)
- 2Preston C. Stockley’s Drug Interactions. Pharmaceutical Press. 2019. https://www.pharmaceuticalpress.com/products/stockleys-drug-interactions/ (accessed July 2024)
- 3British National Formulary. National Institute for Health and Care Excellence. 2024. https://bnf.nice.org.uk/ (accessed July 2024)
- 4British National Formulary for Children. National Institute for Health and Care Excellence. 2024. https://bnfc.nice.org.uk/ (accessed July 2024)
- 5Clinical Knowledge Summaries. National Institute for Health and Care Excellence. 2024. https://cks.nice.org.uk/ (accessed July 2024)


