Eye of Science / Science Photo Library
Scarlet fever is an infectious disease caused by toxin-producing strains of the bacteria Streptococcus pyogenes, also known as group A streptococcus (GAS). GAS can colonise the throat or the skin. Scarlet fever occurs most commonly in association with pharyngitis, but may also result from infection at other sites, including wound infection and puerperal sepsis[1]
.
In scarlet fever, the release of erythrogenic exotoxins results in the characteristic fever and rash. The management of scarlet fever, including treatment and potential complications, are the same as those for streptococcal pharyngitis.
Scarlet fever is highly contagious and, if not treated with antimicrobials, can be infectious for two to three weeks after the onset of symptoms (with antimicrobials it remains infectious for 24 hours after starting treatment). Transmission occurs by direct person-to-person contact via saliva or nasal secretions or, rarely, by indirect contact through objects or hands. The incubation period is two to five days.
The disease is most common in children aged between two and eight years. There is seasonal variation and in the northern hemisphere most cases occur between December and April, with peak incidence in March[2]
. There are sometimes outbreaks in schools or other institutions.
In England, scarlet fever is a notifiable disease and typically around 3,000–4,000 cases are diagnosed each year. Recently, however, there has been a substantial increase in cases, with more than 14,000 cases notified in 2013–2014[3]
. Public Health England data for 2014–2015 indicates ongoing increased levels for the second consecutive year. As of 13 March 2015, there were 5,746 cases of scarlet fever reported in England since 8 September 2014, compared with 2,833 cases during the same period in 2013–2014 (see ‘Scarlet fever activity in England’)[4]
. Around 89% of cases have been reported in children under ten years of age (median four years).
Scarlet fever activity in England
High numbers of notifications of the bacterial infection have occurred in England for the past two years; currently the highest incidence of cases in the 2014-2015 outbreak has been reported in the East Midlands, with 15.9 notifications per 100,000 people.
Weekly scarlet fever notifications from 2008–2015
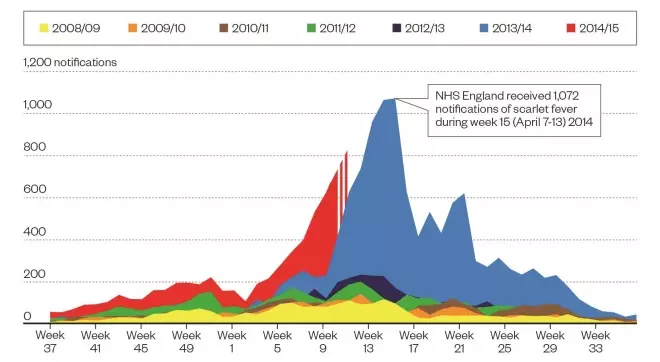
Source: © Crown copyright. Reproduced with permission of Public Health England. Data correct as of 10 March 2015
Reported scarlet fever infections in England 2014–2015
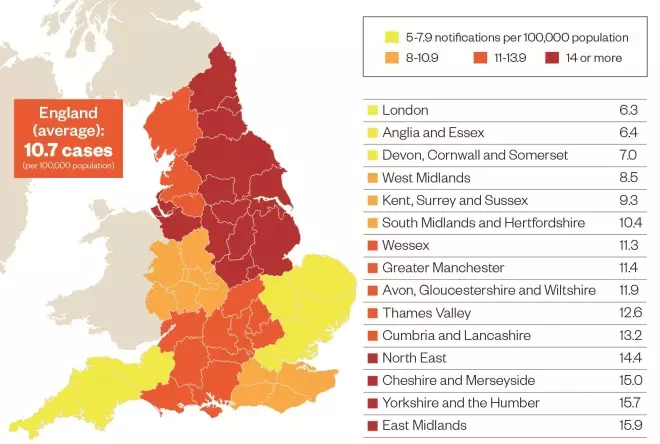
Source: Public Health England. Data correct as of 13 March 2015
Presentation
The initial clinical features of scarlet fever are non-specific and include sore throat, fever, headache, malaise, nausea and vomiting.
A characteristic diffuse, red, blanching rash usually develops by day two (see photo guide). It often starts on the upper trunk, before spreading to the rest of the trunk, the neck and limbs; the palms and soles are not affected. The redness is particularly marked in the skin folds of the neck, axillae, groin, elbow and knees; these red areas are called Pastia’s lines. The rash has a ‘sandpaper’ feel, which may help detection in patients with darkly-pigmented skin.
Patients with scarlet fever have a flushed face, except for the area around the mouth; this is called circumoral pallor and is characteristic of scarlet fever. This may be accompanied by exudative tonsillopharyngitis, enlarged cervical lymph nodes, small red spots on the palate (petechiae) and a ‘strawberry tongue’. Patients initially have a ‘white strawberry tongue’, which has a white coating with red papillae visible beneath; when this coating is lost, the tongue appears beefy and red (‘red strawberry tongue’).

Photo guide: clinical features of scarlet fever
Source: BSIP SA / Alamy and Dr P Marazzi / Science Photo Library
1) Strawberry tongue initially appears white, but when the coating is lost appears beefy and red; the patient also has circumoral pallor around the mouth.
2) A red, blanching rash usually develops by day two. It often starts on the upper trunk before spreading to the neck and limbs.
Scarlet fever is usually a mild, self-limiting disease that lasts around one week. After the rash is resolved, skin peeling (desquamation) of the tips of the digits and, to a lesser extent, the limbs and trunk occurs.
Complications may occur, although these are rare with appropriate antibiotic treatment.
Possible suppurative complications include:
- Peritonsillar/retropharyngeal abscess
- Cervical lymphadenitis
- Mastoiditis
- Acute sinusitis
- Otitis media
- Pneumonia
- Septic arthritis
- Central nervous system infection (meningitis, brain abscess).
In addition, complications can occur after the infection has resolved, including acute post-streptococcal glomerulonephritis and acute rheumatic fever. These non-suppurative, immune-mediated complications are only occasionally seen in developed countries, but remain a common cause of cardiac and renal disease in developing countries.
Diagnosis
Scarlet fever is usually diagnosed based on clinical presentation. Differential diagnoses of the scarlatiniform skin rash include staphylococcal toxic shock syndrome, viral rash, drug-associated rash and Kawasaki disease[1]
.
Clinical algorithms are available to assist with the diagnosis of acute streptococcal pharyngitis. The Scottish Intercollegiate Guidelines Network (SIGN) recommends the Centor scoring system, which uses the following clinical criteria:
- Tonsillar exudate
- Tender anterior cervical nodes
- Lack of a cough
- History of fever.
Patients with four of these signs have a 25–86% chance of GAS infection; conversely, patients with one of these signs have a 2–23% chance of GAS infection (depending on age, local prevalence and seasonal variation) and other diagnoses should be considered[5]
. The score is not validated for use in children under three years of age.
Laboratory tests can be used to differentiate between bacterial and viral pharyngitis, and a throat swab culture is recommended for the diagnosis of GAS pharyngitis. However, interpretation is made difficult by the fact that GAS are often present in the throat of young children without causing illness. Rapid streptococcal antigen tests are also available. These allow quick and easy access to results, but are less sensitive than culture.
Measurement of anti-streptococcal antibody titres is not useful in the diagnosis of acute infections, but may have a role in diagnosis of post-infection complications such as acute rheumatic fever and acute glomerulonephritis[6]
.
Management
The goal of antibiotic therapy is to reduce duration of symptoms and prevent complications.
Although GAS infections such as scarlet fever are generally susceptible to many antibiotics, penicillins remain the treatment of choice on account of their proven efficacy and safety (see ‘Treatment options for scarlet fever’). Worldwide, no penicillin-resistant clinical isolates of GAS have been identified to date.
| Treatment options for scarlet fever | |||
|---|---|---|---|
Drug and route | Patient age | Recommended dose | Duration |
Phenoxymethylpenicillin (pencillin V), oral | 1–6 years | 125mg every six hours | 10 days |
6–12 years | 250mg every six hours | ||
12–18 years | 250–500mg every six hours | ||
Adults | 500mg every six hours | ||
Cefalexin, oral | 1–5 years | 125mg two times a day | 10 days |
5–12 years | 250mg two times a day | ||
12 years and over | 500mg two times a day | ||
Clarithromycin, oral | 1–12 years | 7.5mg/kg/dose twice daily (max 250mg) | 10 days |
12 years and over | 250mg two times a day | ||
Azithromycin, oral | 6 months–12 years | 12mg/kg (max 500mg) once a day | 5 days |
12 years and over | 500mg once a day | ||
There is now convincing evidence that cephalosporins are more effective than penicillins in treatment of streptococcal pharyngitis. This may be because penicillins are hydrolysed by beta-lactamases produced by organisms that naturally reside in the oropharynx, while cephalosporins are not. However, penicillins are still preferred as a first-line treatment because of their narrow spectrum and low cost[7]
.
Orally administered amoxicillin, given as a single daily dose for ten days, is as effective as orally administered phenoxymethylpenicillin (penicillin V) or amoxicillin given multiple times per day for ten days. This approach may be suitable where compliance with multiple doses of penicillin is difficult to achieve. Patients deemed unlikely to complete a full ten-day course of oral therapy should be given a single intramuscular dose of benzathine benzylpenicillin[6]
.
For patients with a penicillin allergy, the treatment of choice is a first-generation cephalosporin (except for patients with a history of anaphylaxis to penicillins) or a macrolide, such as erythromycin, clarithromycin or azithromycin.
Erythromycin is associated with substantially higher rates of gastrointestinal adverse effects than are the other agents. Azithromycin has a longer half-life and sustained intracellular concentration compared with alternative treatments, and therefore a shorter course (five days) is effective against streptococcal pharyngitis.
Treatment should be given for the full recommended length even if there is a prompt response to therapy. Testing for microbiological clearance is not performed routinely as 7–37% of children will still remain positive for GAS on throat swab culture despite appropriate treatment. These children are most likely to be chronic carriers of GAS and further antibiotic therapy is generally not indicated[6]
.
Infection control
Children with scarlet fever should not return to school or childcare facilities until at least 24 hours after starting appropriate antimicrobial therapy. Close contact with other children during this period should be avoided. If the child is admitted to hospital, staff should follow local droplet transmission protocols until a minimum of 24 hours after starting appropriate antimicrobial therapy.
Household and family members of patients with GAS pharyngitis are at increased risk of invasive GAS infection. People in close contact with affected patients should be advised to be vigilant and seek medical help if they notice symptoms of GAS infection.
Routine testing of asymptomatic household contacts is not required because of the limited efficacy of antibiotic prophylaxis and potential risks associated with antibiotic use, including adverse effects and promotion of resistance[2],
[6]
. However, antibiotic prophylaxis can be considered in exceptional circumstances, such as in patients with severe immunosuppression. The recommended antibiotic prophylaxis regimen is the same as for treatment.
In the event of a possible outbreak of scarlet fever in a school or childcare facility, local public health experts should be informed[2]
and advice sought. Public health management includes ‘inform and advise’ for exposed individuals, exclusion of symptomatic individuals and consideration of use of chemoprophylaxis[2]
.
Elisabeth Holden is a specialty trainee in year 5 at the Department of Microbiology, Hirminder Ubhi is an antibiotic pharmacist and
Mitul Patel is a consultant microbiologist, all at Birmingham Children’s Hospital NHS Foundatio
n Trust.
References
[1] Mandell GL, Bennett JE & Dolin R. Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases, 7th Edition. Churchill Livingstone 2009.
[2] Public Health England. Interim guidelines for the public health management of scarlet fever outbreaks in schools, nurseries and other childcare settings. PHE public gateway number: 2014034. London: PHE 2014.
[3] Public Health England. Group A streptococcal infections: seasonal activity 2014/15. Health Protection Report 2014;8(44): Infection (News) Report. London: PHE 2015.
[4] Public Health England. Group A streptococcal infections: update on seasonal activity 2014/15. Health Protection Report 2015;9(5): Infection (News) Report. London: PHE 2015.
[5] Scottish Intercollegiate Guidelines Network. Management of sore throat and indications for tonsillectomy. A national clinical guideline. SIGN Guideline 117. Edinburgh: SIGN 2010.
[6] Shulman TS, Bisno AL & Clegg HW. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clinical Infectious Diseases 2012;15:55:e86–102.
[7] Casey JR & Pichichero ME. Meta-analysis of cephalosporin versus penicillin treatment of group A streptococcal tonsillopharyngitis in children. Pediatrics 2004;113:866–882.



