
Dr P. Marazzi / Science Photo Library
Tetanus is caused by a neurotoxin produced by the bacterium Clostridium tetani. The disease is characterised by muscle contractions of the jaw and neck, including generalised muscle spasms. Although it is now rare in the developed world, tetanus can be fatal without appropriate and timely access to medical care[1]
.
Estimates from the Global Burden of Disease Study, published in 2015, suggest that more than 56,000 deaths worldwide were tetanus-related in 2015, of which 79% occurred in sub-Saharan Africa and south Asia[2]
. In the UK, since the introduction of the national tetanus immunisation programme in 1961, the number of cases has significantly reduced[3]
. Between 2001 and 2018, 118 cases and 13 deaths were reported in England and Wales[3]
.
Tetanus can affect people of all ages; however, the highest incidence in the UK is in adults aged over 64 years because they are more likely to be inadequately vaccinated[3]
. Newborn babies and mothers who have not been vaccinated, as well as people who inject drugs, are also at a higher risk of tetanus[3]
.
This article discusses the transmission and diagnosis of tetanus, as well as the main management options. It also covers the prevention of the disease through vaccination.
Causes and transmission
C. tetani is a Gram-positive, spore-forming bacillus commonly found in soil and the faeces of animals, such as horses and cows[1]
. Human infection occurs through direct contamination of a wound with these spores; tetanus is not spread from person to person[1],[3],[4]
. Common ways in which tetanus is acquired include:
- Burns with systemic sepsis;
- Certain animal bites and scratches (if the animal lives in an agricultural setting);
- Compound fractures;
- Contaminated surgery (use of non-sterile instruments/material);
- Cuts with/without foreign objects;
- Eye injuries;
- Gunshot wounds;
- Injecting contaminated drugs;
- Piercings;
- Puncture wounds acquired in a contaminated environment (e.g. gardening injuries);
- Splinters and other puncture wounds[1],[3],[5]
,[6]
.
The average incubation period of the disease is between 3 and 21 days[3]
. Under favourable anaerobic conditions, the spores germinate into toxin-producing tetanus bacilli. The potent neurotoxin is transported via the blood and the lymphatic system to the spinal cord and brainstem, where it enters inhibitory interneurons within the host. It then binds to membrane proteins within the neurons and disrupts the release of inhibitory neurotransmitters in the central nervous system that normally modulate anterior horn cells and muscle contraction. This results in increased muscle tone, contractions, painful spasms and autonomic instability[1],[4]
.
The tetanus toxin also affects the neural control of adrenal-released catecholamine, causing an increase in the activity of the sympathetic pathway, which manifests as tachycardia, sweating and hypertension[4]
. The effects on the anterior horns cells, the brainstem and autonomic neurons are long lasting; recovery requires the growth of new axonal nerve terminals. Therefore, tetanus usually lasts four to six weeks[5]
.
Symptoms
There are three main clinical presentations of tetanus[1],[4]
:
Generalised tetanus
This is the most common and severe clinical form of tetanus and is characterised by trismus (lockjaw), muscle rigidity and painful muscle spasms. During generalised tetanic spasms, patients characteristically clench their fists, arch their back, and flex and abduct their arms while extending their legs. Continual spasms and rigidity can lead to breathing difficulties[4],[7]
.
Other severe symptoms include autonomic instability (i.e. when the autonomic nervous system does not function correctly), resulting in tachycardia, hypertension and sweating (sometimes rapidly alternating with bradycardia and hypotension)[7]
.
Local tetanus
Presents with tonic and spastic muscle contractions in one extremity or body region, usually in the same area as the injury site. Local tetanus often, but not invariably, progresses to generalised tetanus[4],[7]
.
Cephalic tetanus
This is a rarer form of the disease. Patients with injuries to the head or neck may present with cephalic tetanus, which initially involves only cranial nerves. The facial nerve is most commonly affected, but involvement of other cranial nerves may also occur[5]
. Patients may manifest confusing clinical findings including dysphagia, trismus and focal cranial neuropathies that can lead to a misdiagnosis of stroke. Like other forms of local tetanus, patients with cephalic tetanus can progress to generalised tetanus[5]
.
Diagnosis
The diagnosis of tetanus includes the presence of clinical symptoms, a history of recent events (e.g. recent cut or wound that may have introduced tetanus spores) and differential diagnosis
[1]
,[3]
. Tetanus is more likely if there is dirt or something inside the wound and if the patient has not been fully vaccinated.
Table 1 shows how the severity of symptoms of generalised tetanus can be graded.
| Grading of severity | Signs and symptoms |
|---|---|
| Grade 1 (mild) |
|
| Grade 2 (moderate) |
|
| Grade 3a (severe) |
|
| Grade 3b (very severe) |
|
| Reproduced with permission from Public Health England [3] | |
Laboratory investigations, such as polymerase chain reaction and culture of C. tetani or a bioassay of the toxin, are available to support diagnosis. However, toxigenic C. tetani can be cultured from wounds in patients without tetanus, therefore, these investigations should only be used to support diagnosis[1]
.
Tetanus (local and generalised) is a notifiable disease, so the local health protection team must be notified of any suspected cases[3]
.
Treatment
Suspected tetanus with no symptoms
Patients presenting with a tetanus-prone wound (e.g. puncture-type injuries acquired in a contaminated environment) but no symptoms need to be individually evaluated to determine the best course of action. Their vaccination and medical history should be obtained, and the wound should be assessed (see Figure 1)[5]
.
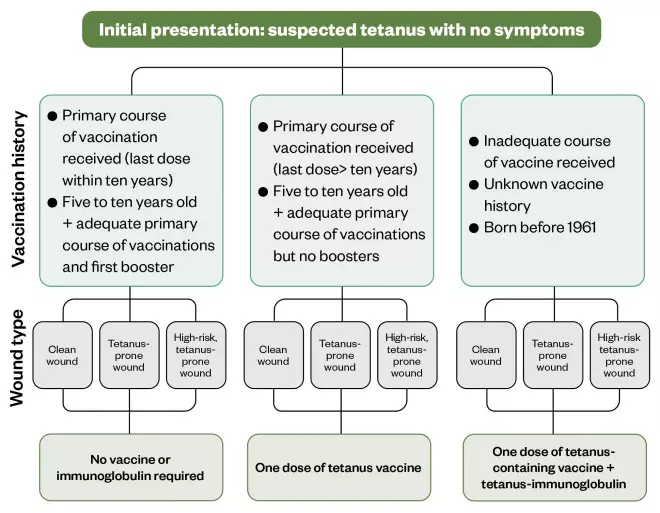
Figure 1: Management of suspected tetanus with no symptoms
To prevent the development of tetanus, all contaminated wounds should be thoroughly cleaned and, if required, surgical debridement of dead, damaged or infected tissue should be arranged[5]
.
Following this, a tetanus-containing vaccine and/or immunoglobulin should be administered if necessary (see Table 2). If intra-muscular tetanus immunoglobulin (IM-TIG) cannot be sourced, Public Health England (PHE) recommends Subgam 16% (human normal immunoglobulin; Bio Products; see Table 3)[3]
.
| Vaccination history | Type of wound | |||
|---|---|---|---|---|
| Clean wounda | Tetanus-prone wound | High risk tetanus-prone wound | Future treatment | |
| No vaccine or tetanus immunoglobulin (TIG) required | No vaccine or TIG required | No vaccine or TIG required | Provide further doses to complete the recommended schedule (i.e. further boosters if necessary) |
| No vaccine or TIG required | Administer re-enforcing dose of vaccine | Administer re-enforcing dose of vaccine And Immediate dose of TIG or Subgam 16% at a different site | |
| Administer re-enforcing dose of vaccine | Administer re-enforcing dose of vaccine And Immediate dose of TIG or Subgam 16% at a different site. | Administer re-enforcing dose of vaccine And Immediate dose of TIG or Subgam 16% at a different site | |
| a Clean wound is defined as less than six hours old, non-penetrating with negligible tissue damage b Adequate course is defined as receiving at least three doses of vaccinations at appropriate time intervals Reproduced with permission from Public Health England [3] , [6] | ||||
| Indication | First line: IM-TIG | Second line: Subgam 16% (1000mg) |
|---|---|---|
| Most uses | 250 units | 1 vial (6.4mL) |
More than 24 hours since the wound occurred Heavy contamination of wound Burns | 500 units | 2 vials (12.8mL) |
| IM-TIG: intra-muscular tetanus immunoglobulin Reproduced with permission from Public Health England [3] | ||
Tetanus with symptoms
Management of clinical tetanus with symptoms involves neutralisation of the toxin, wound debridement, antimicrobial therapy and supportive care for severe symptoms.
Treatment with intravenous immunoglobulin
Intravenous tetanus immunoglobulin (IV-TIG) is recommended for the treatment of clinical tetanus, however, owing to shortages within the UK, PHE also recommends the use of human intravenous immunoglobulin (IVIG), which contains adequate levels of tetanus antibody.
The required dose of anti-tetanus antibodies is based upon weight. For patients weighing less than 50kg, 5,000 IU (international units) immediately is recommended, whereas 10,000 IU is recommended for individuals weighing more than 50kg[3]
. Owing to varying concentrations of anti-tetanus antibodies in each product, the recommended volume of IVIG varies between brands. For information on dosing of IVIG, please refer to the PHE guidance
[3]
.
Adverse reactions (e.g. headache, flushing and nausea) may be related to the rate at which the volume is infused, therefore, administration of IVIG should always begin at the recommended rate stated in the summary of product characteristics of each brand, and increased accordingly[8]
. Patients should be monitored closely during administration, and those who experience a hypersensitivity reaction can be prescribed antihistamines if necessary.
Antimicrobial therapy
Alongside wound cleaning and debridement, treatment with antimicrobials should be considered[3],[4],[5]
. Traditionally, benzylpenicillin was used (0.6–1.2g four times daily), however, owing to concerns around penicillin being a competitive inhibitor of the GABA(A) receptor, and potentially increasing muscle rigidity, its use has now decreased. Therefore, metronidazole 500mg intravenous (IV) three times daily is now the antimicrobial of choice – it has a better safety profile and has shown a reduction in mortality when compared with benzylpenicillin[9]
. Suggested treatment durations range from 7–14 days[5],[10]
. It is always important to confirm patients’ allergy status before prescribing antimicrobials.
Supportive care
Patients experiencing severe tetanus symptoms will require supportive care and possible admission to intensive care.
Muscle spasms
Control of rigidity and spasms is achieved by sedation using benzodiazepines. Diazepam can be administered by various routes (i.e. IV, rectal, oral); the licensed IV dose is 0.1–0.3mg/kg repeated every 1–4 hours or a continuous infusion of 3–10mg/kg every 24 hours. However, owing to the long-acting metabolites, long-term use may result in accumulation. Therefore, midazolam, which has a shorter half-life and is available as an IV preparation, may be preferred[11]
. Doses of midazolam are variable; therefore, specialist advice should always be consulted. Side effects for benzodiazepines can include respiratory depression and lactic acidosis[11]
.
Non-depolarising neuro-muscular blocking agents (e.g. pancuronium) have been used when sedation alone is inadequate in controlling spasms, however pancuronium has been linked to tachycardia and hypertension. Newer agents, such as rocuronium (300–600 microgram/kg/hour, adjusted according to response), are associated with less autonomic disturbance, but are generally more expensive[11],[12]
.
Antispasmodics (e.g. baclofen) have also been used to improve muscle spasms. As oral treatment has a poor blood–brain barrier penetration, it is not considered to be beneficial, therefore, intrathecal boluses or infusions are used[4]
. However, this treatment option is costly and should only be considered under specialist clinical advice owing to the narrow therapeutic range and risk of adverse effects (e.g. respiratory depression and coma)[13]
.
As muscle spasms can compromise airways, it is important to ensure patients are adequately ventilated to avoid respiratory failure and aspiration. In severe cases of tetanus, mechanical ventilation or tracheostomy placement is required, especially in patients receiving high doses of sedatives to control muscle spasms[4],[5],[12]
.
Magnesium sulphate reduces the release of catecholamine from nerves and reduces receptor sensitivity to it. Studies have shown it has been effective in helping to control autonomic disturbance in patients with severe tetanus who are heavily sedated, while also helping to relieve spasms in ventilated patients[14]
. A loading dose of 5g over 20 minutes followed by an ongoing infusion titrated to the control of symptoms have been supported. Doses as high as 4–5g/hour may be required[11]
.
Autonomic dysfunction
Control of the autonomic dysfunction is complex and may require a combination of drugs, depending on the clinical situation. The use of beta-blockers (e.g. propranolol and labetolol) have been used to control hypertension and tachycardia, however, the use of propranolol has been linked to sudden cardiac death and should be prescribed with caution[15]
.
Owing to a reduced ability to swallow, an increase in metabolic rate and, consequently, a prolonged hospital stay, it is important to provide nutritional support to patients with tetanus. Nutrition can be achieved via enteral feeding or total parenteral nutrition until the patient has fully recovered[11],[12]
.
Non-pharmacological management
This includes regular chest physiotherapy and suction of excessive secretions to help prevent respiratory complications[12]
. Patients should also avoid any loud noises or bright lights, as these can be sensory triggers for muscle spasms[6]
.
Complications
As a result of repeated muscle spasms, fractures and tendon rupture can occur in patients with severe tetanus, as well as rhabdomyolysis (the rapid breakdown of damaged skeletal muscle). Muscle rigidity and spasms can make swallowing and coughing more difficult, which may result in the inhalation of secretions or contents of the stomach. This can lead to a lower respiratory tract infection (also known as aspiration pneumonia)[11],[12]
.
Generally, severe cases of tetanus require admission to critical care for long periods of time (up three to five weeks). As a result, these patients are at a higher risk of developing nosocomial infections, ventilator-associated pneumonia and gastrointestinal haemorrhage[4],[11],[12]
. The lack of immobility over several weeks also increases their risk of developing a thrombosis, meaning patients must also receive appropriate thromboprophylaxis[11],[12]
.
Vaccination
Tetanus can be prevented through active immunisation with tetanus vaccine[3]
. In the UK, PHE recommends a total of five doses of the vaccine (which is only available in the UK as a combined product)[3],[6]
. It is important to note that people who recover from tetanus do not have natural immunity and can be infected again, therefore, they must also be immunised.
It is recommended that children receive the vaccine at two, three and four months of age (see Table 4). This primary course is followed by two booster doses at 3 years 4 months old and 14 years old. For adults, the primary course consists of three doses, each one month apart, with the first booster administered five years after the primary course and the second booster administered ten years after the first booster. If the primary course is interrupted, it is recommended to continue with the remaining doses, ensuring there is one month between each dose[3],[6]
.
Although extremely rare, anaphylaxis can occur as a side effect of the vaccination. Localised redness and swelling occur in more than one in ten patients, with symptoms eventually resolving[16]
.
| Immunisation | Children aged under 10 years | Adult and children aged over 10 years |
|---|---|---|
| Primary immunisation course | Three doses of vaccine (usually as DTaP/IPV/Hib/HepB) at two, three and four months of age. | Three doses of vaccine (as Td/IPV)** one month apart. |
| First booster | One dose of vaccine (as DTaP/IPV*) at age four to seven years. | One dose of vaccine (usually as Td/IPV)** for those who have completed primary immunisation and last dose was five or more years ago. |
| Second booster | One dose of Td/IPV**, ten years after first booster | |
| *Combined diphtheria/tetanus/pertussis/polio (DTaP/IPV) **Combined tetanus/low dose diphtheria/inactivated polio vaccine (Td/IPV) Reproduced with permission from: Public Health England [3] | ||
Box: Best practice
Pharmacy professionals should be able to apply the following best practice principles in relation to vaccination and the management of tetanus-prone wounds as outlined below.
Provide vaccination advice
- Tetanus is found throughout the world, therefore, ensure individuals are fully vaccinated before travelling abroad, especially to areas with limited medical facilities and where access to post-exposure treatment may be difficult
- These individuals should receive a single dose of combined tetanus/low dose diphtheria/inactivated polio vaccine (Td/IPV) prior to travel, every ten years[6]
; - Community pharmacies that offer travel vaccination services can administer the vaccination. Individuals who are unsure of their immunisation status or have an incomplete immunisation status should be treated as unimmunised, as per PHE guidance[17]
; - Pharmacies that do not offer this service can refer individuals to their GP/vaccination clinic and signpost them to useful websites (see Useful resources).
- These individuals should receive a single dose of combined tetanus/low dose diphtheria/inactivated polio vaccine (Td/IPV) prior to travel, every ten years[6]
Provide wound management advice
- Patients presenting with a wound should receive basic advice, including cleaning the wound by rinsing it under running water, applying pressure and raising the injury, if possible, to reduce the bleeding. If the bleeding does not stop, or if there is a foreign object in the cut or the wound looks infected, advise the patient to seek further medical attention at their local hospital emergency department or minor injuries unit[18]
; - Obtain the patient’s tetanus immunisation status and medical history to help identify their risk of developing tetanus. If the patient is unsure of their immunisation status, advise them to seek further medical attention as they may require tetanus immunoglobulin/human normal immunoglobulin and/or vaccination. When obtaining a history, it is important to clarify from the patient what was administered in the past – it is not uncommon for patients to confuse the immunoglobulin for the vaccine. This affects the length of protection as the tetanus immunoglobulin only lasts a few weeks, whereas the routine booster vaccine can last up to ten years[6]
; - If a patient is experiencing muscle spasms or stiffness following a recent trauma, call 999.
Useful resources
Peer-reviewed article
This article has been peer reviewed by relevant subject experts prior to acceptance for publication. The reviewers declared no relevant affiliations or financial involvement with any organisation or entity with a financial interest in or in financial conflict with the subject matter or materials discussed in this article.
Financial and conflicts of interest disclosure
The authors have no relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in this manuscript. No writing assistance was used in the production of this manuscript.
References
[1] World Health Organization. Tetanus vaccines: WHO position paper – February 2017. 2017. Available at: https://apps.who.int/iris/bitstream/handle/10665/254582/WER9206.pdf;jsessionid=AC28007E22CAD3AF71B88120F2A9663C?sequence=1 (accessed April 2020)
[2] Kyu HH, Mumford JE, Stanaway JD et al. Mortality from tetanus between 1990 and 2015: findings from the global burden of disease study 2015. BMC Public Health 2017;17(1):179. doi: 10.1186/s12889-017-4111-4
[3] Public Health England. Tetanus. Guidance on the management of suspected tetanus cases and on the assessment and management of tetanus-prone wounds. 2019. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/820628/Tetanus_information_for_health_professionals_2019.pdf (accessed April 2020)
[4] Yen L & Thwaties C. Tetanus. Lancet 2019;393(10181):1657–1668. doi: 10.1016/S0140-6736(18)33131-3
[5] Sexton D. Tetanus. UpToDate. Waltham, MA: UpToDate Inc. 2019. Available at: https://www.uptodate.com/contents/tetanus (accessed April 2020)
[6] Public Health England. The Green Book. Chapter 30: Tetanus. 2020. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/859519/Greenbook_chapter_30_Tetanus_January_2020.pdf (accessed April 2020)
[7] Hassel B. Tetanus: pathophysiology, treatment, and the possibility of using botulinum toxin against tetanus-induced rigidity and spasms. Toxins (Basel) 2013;5(1):73–83. doi: 10.3390/toxins5010073
[8] Palabrica FRR, Kwong SL & Padua FR. Adverse events of intravenous immunoglobulin infusions: a ten-year retrospective study. Asia Pac Allergy 2013;3(4):249–256. doi: 10.5415/apallergy.2013.3.4.249
[9] Ahmadsyah I & Salim A. Treatment of tetanus: an open study to compare the efficacy of procaine penicillin and metronidazole. Br Med J (Clin Res Ed) 1985;291:648–650. doi: 10.1136/bmj.291.6496.648
[10] Hinfey PB. Tetanus. Emedicine Medscape. 2019. Available at: https://emedicine.medscape.com/article/229594-overview (accessed April 2020)
[11] Cottle L, Beeching NJ, Carrol ED & Parry CM. Tetanus. BMJ Best Practice. 2018. Available at: https://bestpractice.bmj.com/topics/en-gb/220 (accessed April 2020)
[12] Cook TM, Protheroe RT & Handel JM. Tetanus: a review of the literature. Br J Anaesth 2001;87(3):477–487. doi: 10.1093/bja/87.3.477
[13] eMC. Lioresal Intrathecal. 2020. Available at: https://www.medicines.org.uk/emc/medicine/1295/SPC/Lioresal+Intrathecal (accessed April 2020)
[14] Attygalle D & Rodrigo N. Magnesium sulphate for control of spasms in severe tetanus: can we avoid sedation and artificial ventilation? Anaesthesia 1997;52(10):956–962. doi: 10.1111/j.1365-2044.1997.206-az0340.x
[15] Buchanan N, Smit L, Cane RD et al. Sympathetic overactivity in tetanus: fatality associated with propranolol. Br Med J 1978;2:254–255. doi: 10.1136/bmj.2.6132.254-a
[16] eMC. REVAXIS suspension for injection in pre-filled syringe. 2017. Available at: https://www.medicines.org.uk/emc/product/5581/smpc (accessed April 2020)
[17] Public Health England. Vaccination of individuals with uncertain or incomplete immunisation status. 2019. Available at: https://www.gov.uk/government/publications/vaccination-of-individuals-with-uncertain-or-incomplete-immunisation-status (accessed April 2020)
[18] NHS. Tetanus. 2017. Available at: https://www.nhs.uk/conditions/tetanus (accessed April 2020)
You might also be interested in…

Everything you need to know about mpox

Norovirus and strategies for infection control
