Wes Mountain/The Pharmaceutical Journal
By the end of this article, you will be able to:
- Describe the prevalence and types of prescribing errors that commonly occur;
- Understand the relationship between human factors and patient safety;
- Apply knowledge of human factors in a clinical or professional setting;
- Recognise unsafe prescribing practices and develop potential strategies to reduce the risk of prescribing errors.

RPS Competency Framework for All Prescribers
This article is aimed to support the development of knowledge and skills related to the following competencies:
Domain 7: Prescribe safely (7.2, 7.4, 7.5)
- Knows about common types and causes of medication and prescribing errors, and knows how to minimise their risk;
- Recognises when safe prescribing processes are not in place and acts to minimise risks;
- Keeps up to date with emerging safety concerns related to prescribing.
Introduction
The principle of ‘patient safety’ is preventing avoidable patient harm in healthcare1. It has been suggested that 1 in 30 patients are affected by preventable medication-related harm, with the highest prevalence (around 50%) occurring during prescribing2. If you consider this statistic in the context of an average prescriber, a pharmacist who prescribes for ten patients a day could potentially cause a medication-related harm every six days.
As more pharmacists take on prescribing roles, it is essential that they understand patient safety to ensure the safe and effective use of medicines; however, ‘to err is human’, and patient safety efforts should not blame healthcare professionals for mistakes, but instead support their work in often flawed systems, attempting to make those as safe as possible3. To tackle patient safety from a prescribing perspective, it is necessary to recognise the fallibility of human nature and debunk the myth that you will not make errors if you try hard enough.
This article will discuss the common factors contributing to prescribing errors, the challenges pharmacist prescribers face, and how understanding ‘human factors’ can help in developing safe prescribing practices and reduce error risk.
The changing role of pharmacists driven by prescribing
As pharmacist prescribing continues to grow, it is essential that the responsibilities for, and complexities of, patient safety are understood4,5. It is likely that increased clinical responsibilities may accelerate the delegation of process and technical aspects of medicines supply to others. As pharmacists look to enhance their prescribing skills and expand their prescribing scope of practice, it is necessary to proactively engage with systems and working practices that prevent errors and promote a safety-first approach to patient care.
While some pharmacists have long benefited from advanced practice roles, (with an associated increase in professional satisfaction and perceived improvement in patient safety and outcomes), there are also factors which can limit pharmacist development in these roles6. In 2020, Rosenthal et al. noted that ‘pharmacist culture’ can be a barrier to pharmacists advancing their clinical practice as independent prescribers7. They highlighted the tendency of pharmacists to be risk-averse, which can make clinical decision making more difficult when working in the ‘grey’ areas of patient care, where outcomes of intervention are less defined and more probabilistic in nature7. This is particularly relevant as prescribing becomes more complex, caused in part by polypharmacy in an ageing population with an increasing burden of long-term conditions and amplified by new pharmacotherapies8. To work safely as a prescriber, it is important to develop a deepened understanding of errors, risk and how systems and culture can influence the way individuals approach their work with patients.
The prevalence of prescribing errors
The Chartered Institute of Ergonomics and Human Factors Pharmaceutical Human Factors Special Interest Group defines safety as “the level of system performance required to keep the incidence of harm (and risk) as low as reasonably practicable”9. It’s important to recognise that the level of acceptable risk will vary depending on the specific situation. For example, acceptable risk in a life-threatening situation will be different to acceptable risk in a self-limiting condition; therefore, pharmacist prescribers require a change in mindset in order to be accountable for prescribing decisions, taking a more flexible approach to assessing risk when making an intervention10. However, it is also necessary to distinguish between unavoidable and avoidable risk and recognise the importance of preventing patient harm from avoidable medication errors.
Medication errors are a significant concern in healthcare systems worldwide. In England alone, it is estimated that over 200 million medication errors occur annually11. Medication errors can have far-reaching consequences for patient wellbeing, health systems and practitioners. Most result in no or low-to-moderate harm; however, some result in severe harm or death12–14. From a purely financial perspective, the annual cost of avoidable medication errors for the NHS is around £100m11.
Errors can occur in all stages of the medication process, including prescribing, dispensing, administration and monitoring. A study of acute hospital trusts in north-west England identified around 9 errors per 100 medication orders, with prescribing errors made by all grades of doctors, including consultants; the highest risk was at admission to hospital12.
In 2009, a systematic review found a high rate of avoidable prescribing errors to be an international problem, with an overall median error rate of 7% (interquartile range 2–14%) of medication orders15. A study involving 15 general practices in England found that around 1 in 20 prescribed items had either a prescribing or monitoring error, with 1 in 550 prescribed items associated with a ‘severe error’13,14. The most common errors were incorrect dose or strength, incorrect timing of dose and incomplete information (e.g. co-amoxiclav prescribed for sinusitis with no dose or frequency specified on the prescription)14.
Most published research about prescribing errors focuses on prescribing by doctors, with relatively little known about the prevalence of prescribing errors made by other healthcare professionals. In 2015, the prevalence of prescribing errors by pharmacists was evaluated, with only 4 errors (0.3%) reported out of 1,415 prescribed medications over a 10-day period16. More recently, a 2021 investigation at an acute NHS trust compared errors by pharmacist prescribers with those by doctors. The error rate for pharmacist prescribers was numerically lower (0.7%), compared with the rate for doctors (9.8%)17. Although it is tempting to conclude that prescribing pharmacists are ‘safer’, it should be remembered that both studies were small, conducted in single-hospital trusts and probably did not compare like-with-like prescribing activities. Further, robust research is required in this area before definitive safety statements can be made.
Despite not yet being able to determine the exact prevalence of prescribing errors, absolute and comparative rates between types of prescribers remains a pressing issue, particularly for the commissioning of safer clinical services. The potential range of causes of prescribing errors requires a multifaceted approach to risk minimisation, including consideration of both systems design and human factors.
Case in practice: critically analysing risk of errors
When considering ways to minimise risk of error, it is important to look critically at existing processes and identify points where errors could potentially occur.
Consider the following case study:
A 77-year-old female presents with a history of episodes of breathlessness and palpitations. On examination, she is found to have atrial fibrillation (AF), and you consider prescribing an anticoagulant.
Consider this scenario:
- List all the stages of prescribing;
- Think of at least one error that could occur at each stage.
Possible answers
The prescribing process is complex and has several stages, with the potential for errors to occur at one or more stages of the process. It is not possible to consider every possible error but here are some suggestions for each stage:
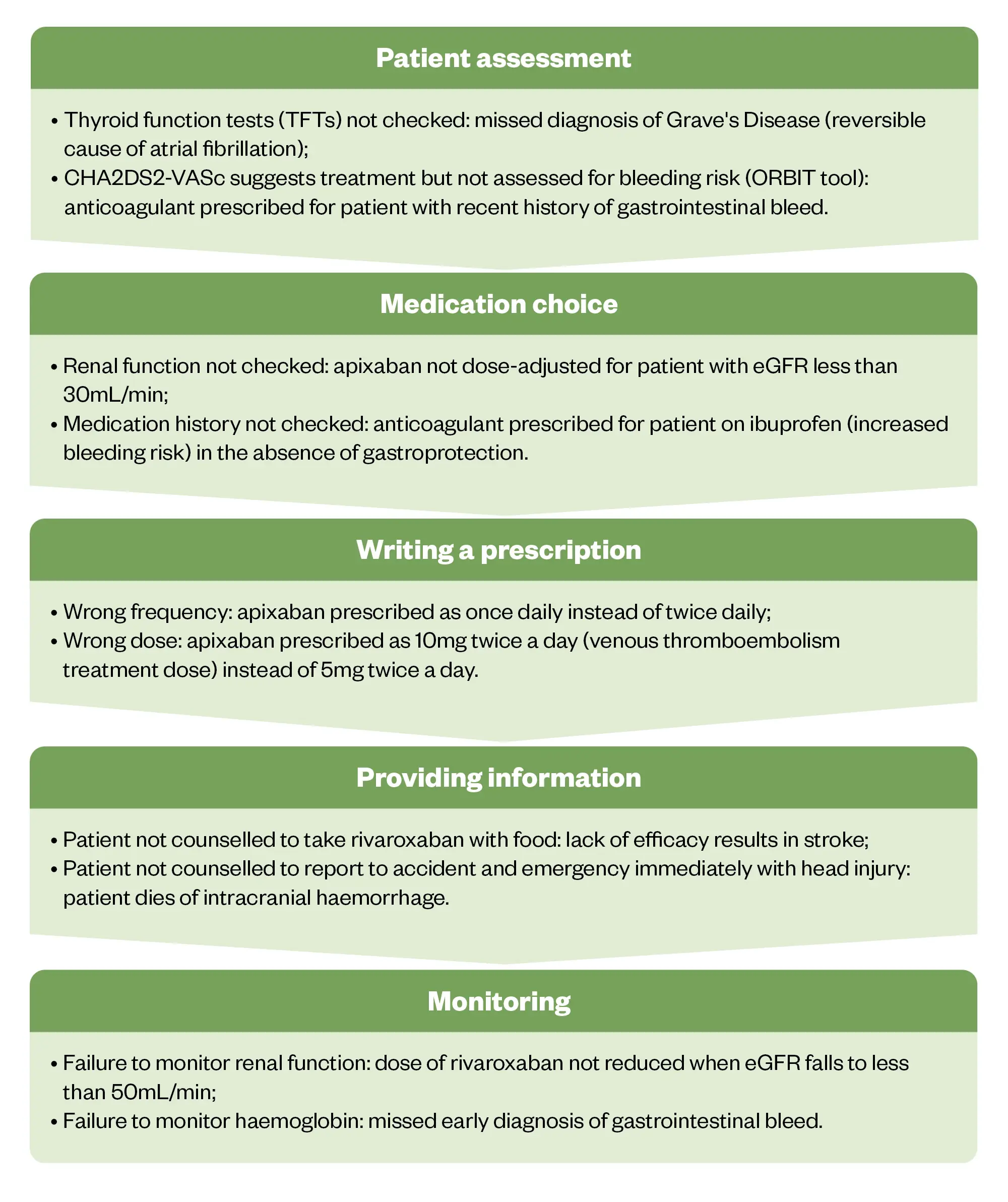
The Pharmaceutical Journal
What are human factors?
As the previous activity has shown, there are countless ways that medical errors could potentially occur. It is vital that the underlying causes of and opportunities for prescribing errors are well understood and that steps are taken to mitigate against them. The application of human factors can greatly aid and improve this process9.
Human factors refers to environmental, organisational and task factors, as well as individual physical and mental characteristics, that can impact on safety18. It has been suggested that all healthcare professionals develop human factors competencies to help them perform effectively and safely within complex healthcare systems9. This is particularly pertinent for pharmacist prescribers, as the majority of medication errors are attributed to prescribing2.
The focus of human factors in healthcare is on understanding human behaviour and human limitations19. This enables the design of technologies, environments and processes to optimise performance through system-wide improvements, improving patient safety and the wellbeing of patients and clinicians18,20.
Aviation is often cited as an industry that has successfully applied human-factor interventions, such as checklists and sterile cockpits, to reduce risk and improve safety. The term ‘sterile cockpit’ originates from aviation regulations and refers to critical phases of flight when flight crews must refrain from non-essential activities or conversations to prevent distractions21. Its success is frequently cited in support of widespread adoption of human factors in healthcare, with attempts made to apply and adapt learnings22.
For example, application of the sterile-cockpit theory to medication rounds is aimed to remove distractions during medicine administration, theoretically allowing greater focus on process and reducing error23. Those involved in aviation safety consistently advocate for the application of human factors; tellingly, the pilot of the Hudson River aircraft incident, Chesley Sullenberger, commented that the aviation industry would “close down” if the same number of fatalities happened in aviation as occur from prescribing errors24.
However, it is also recognised that healthcare has features that require the transfer of learning from aviation to be nuanced23. One factor is the variability and complexity of patients, compared with aircraft22. Another is that the scale of the intervention differs drastically — a single safety intervention in aviation would affect all the passengers on an aircraft simultaneously, whereas a safety intervention in healthcare would need to be repeated on hundreds of individual patients to have the same impact.
Understanding the relationship between human factors and patient safety
The Swiss cheese model, proposed by psychologist James Reason, illustrates that harm often results from a series of small mistakes that align in complex systems, rather than being a result of a single, catastrophic error. Even the most robust systems will have weaknesses, which are the ‘holes’ in the Swiss cheese analogy; given a certain set of circumstances, those weaknesses will align, allowing an error to occur25 (see Figure 226).
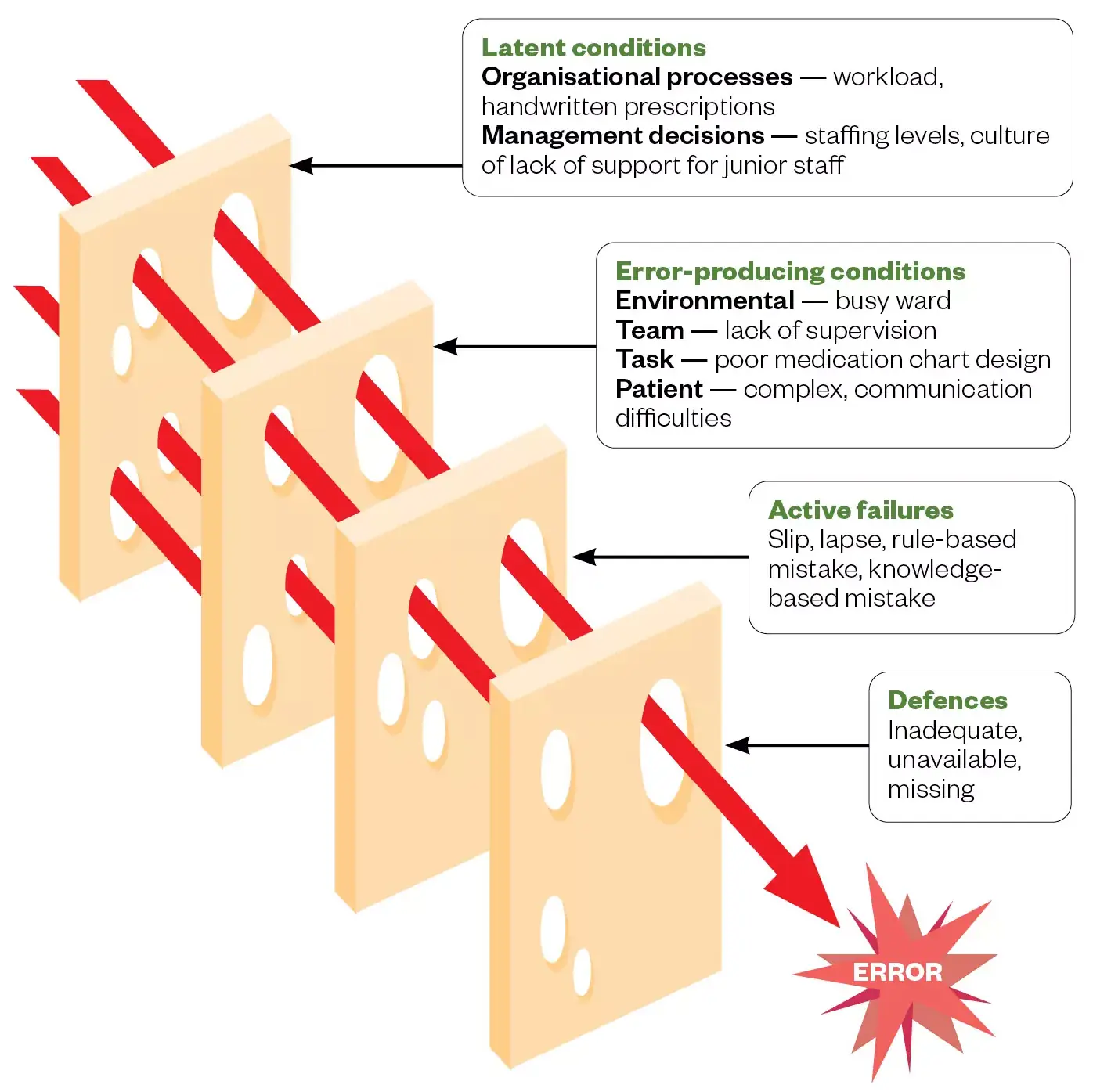
From Dornan et al, adapted from Coombes et al, used with permission
For example, when a patient is prescribed a medication, there will be several layers of defence to prevent an error occurring: electronic prescribing systems, electronic dispensing systems and accuracy checking before, during, and after dispensing among others. However, most pharmacists, during their careers, will experience examples of failures in all these defensive layers.
Reason’s model described two main ways in which humans contribute to errors: active failures and latent failures. Active failures are unsafe acts or omissions by the person whose actions have a measurable, unintended, consequence; for example, a prescriber who makes a calculation error resulting in the overdose of a patient and subsequent toxicity27.
Some other examples of active failures include:
- Mistakes (where the treatment plan itself is inadequate): these are rule or knowledge-based mistakes; for example, writing a prescription for 300mg, not knowing that the correct dose is 100mg;
- Slips/lapses (where the action does not go to plan): these are omissions, memory or attentional failures; for example, intending to write a prescription for 100mg but writing 300mg instead owing to lapse in concentration or forgetting to prescribe a drug after being interrupted;
- Violations (where a deliberate action is taken that proves to be harmful): these involve deviating from a protocol or standard operating procedure; for example, prescribing lithium without checking that appropriate monitoring has been carried out owing to lack of time.
Latent failures are the underlying factors that affect the conditions in which errors occur. They may be caused by decisions made by a person outside of the workplace; for example, senior managers, commissioners or policy makers. These decisions might result in conditions — such as a stressful working environment, inadequate systems or poor maintenance of equipment — all of which can contribute to errors28.
Vincent et al. applied Reason’s Swiss cheese model to patient safety in healthcare, introducing a framework of seven factors that influence clinical practice (see Box)28. The framework has been used to investigate errors in healthcare20, promote the examination of influences at each stage of clinical practice, and to make interventions that improve patient safety28.
Box: Factors that influence patient safety in clinical practice28,29
- Institutional context (e.g. national policies; regulatory standards)
- Organisational and management factors (e.g. safety culture; financial resources; organisational structure; staff training and education)
- Work environment (e.g. workload; staffing levels and skills mix; availability of drugs, equipment and supplies)
- Team factors (e.g. verbal and written communication; team structure; team goals)
- Individual (staff) factors (e.g. knowledge and skills; physical and mental health; motivation)
- Task factors (e.g. familiarity or difficulty of task; availability and use of protocols)
- Patient characteristics (e.g. complex medical history; language barrier; social factors)
The ‘Systems Engineering Initiative for Patient Safety’ (SEIPS) model further adapts this framework and considers how interactions between different work–system factors produce different outcomes (as opposed to simple cause-and-effect relationships)30 (see Figure 231). The framework can be considered a more holistic view and identifies six broad elements within work systems: the internal and external environment, organisation, person, tasks, and tools and technologies. Modulated differences in interactions between each component results in different outcomes, both for patients and employees30. Crucially, the framework recognises that people are central to the work system, and that systems should be designed to support people at the centre of the system32.
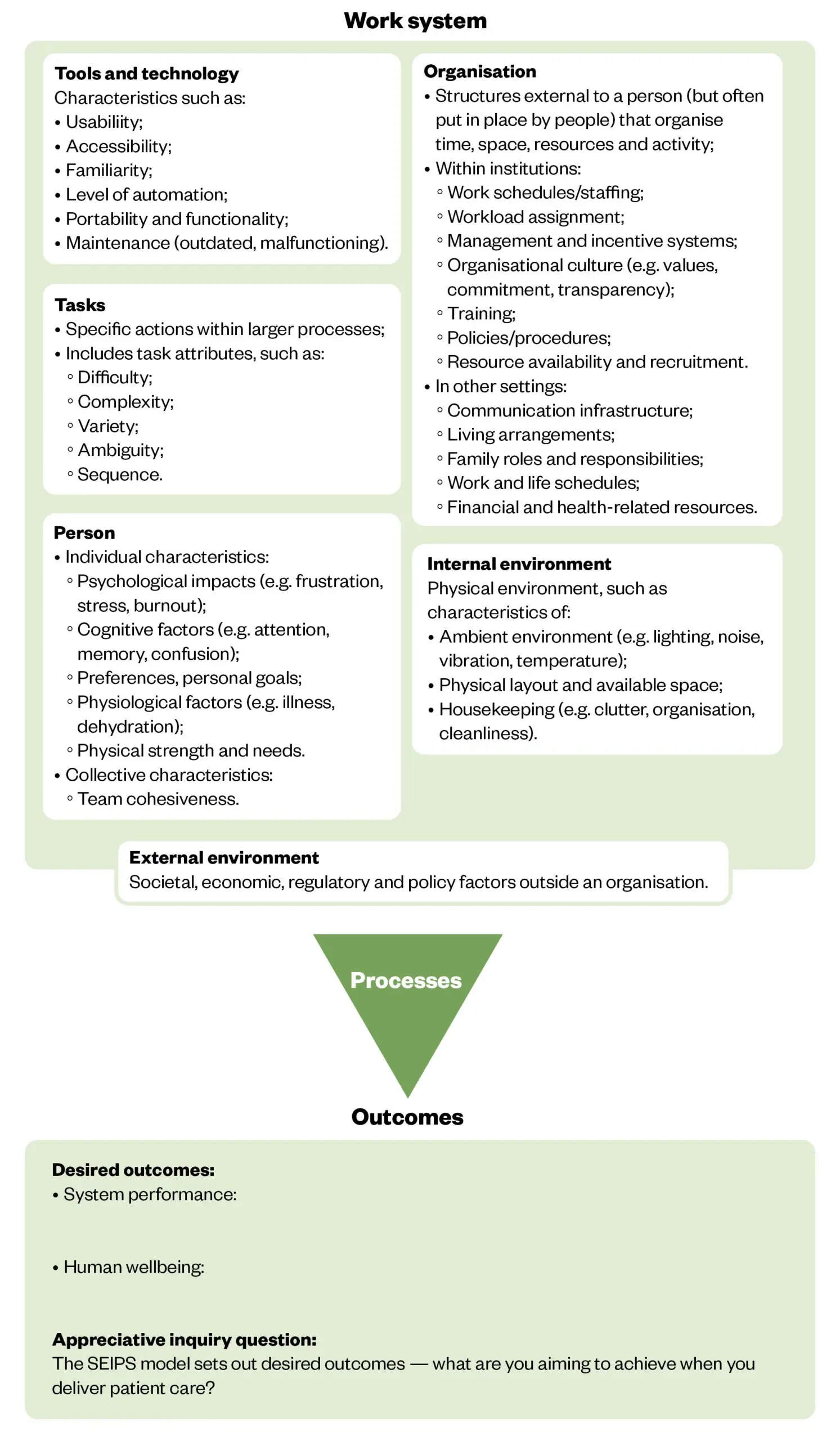
The Pharmaceutical Journal, adapted from NHS England
The SEIPS model can be used proactively to help design systems or reactively to help investigate incidents30. In a paper published in 2018, a large, acute NHS hospital used the SEIPS model to identify several systems issues that were leading to prescribing errors on admission33. The investigation involved considering the people, tasks, tools and technologies, physical environment and organisational conditions involved during the medicines-reconciliation process carried out by junior doctors. This human-factors-led system analysis resulted in a variety of interventions, including a relatively simple intervention of improving junior doctor access to GP records by issuing more individual NHS smartcards33. Although simple, this intervention may not have been identified and implemented if each prescribing error was considered to be solely the fault of the prescribing doctor and dealt with on an individual basis. By considering how the design of work systems influenced processes and affected outcomes, the intervention improved the medicines reconciliation process for all prescribers.
How human factors can improve patient safety
Although it is difficult for most individuals to address wider organisational factors, pharmacist prescribers can be effective vectors for change through proactive feedback to managers via both formal and informal mechanisms. In addition, by recognising some of the human factors that affect themselves and their teams, prescribers can apply the principles already outlined to improve patient safety, personal performance, and wellbeing32.
For instance, it is well known that sleep deprivation and tiredness can significantly impair important neurocognitive functions — such as attention, decision making and working memory — increasing the risk of errors34. However, this knowledge is not extrapolated to healthcare environments, where complex decisions are often being made by fatigued members of the team.
Other factors that can affect personal performance include hydration, nutrition and stress. ‘HALT’ — Hungry, Anxiety/anger, Late/lonely, Tired — is a useful mnemonic for considering these personal factors; stopping for a moment to improve your personal performance could have a positive impact on patient safety and team working32. The ‘I’M SAFE’ — Illness, Medication, Stress, Alcohol/drugs, Fatigue, Eating and elimination — checklist is another example of a simple self-assessment tool that can be used to assess your current ability to perform safely35.
Effective communication is also a behavioural factor commonly linked with medication errors. One suggestion is to imitate the aviation industry, in which all essential communication is verbal and staff are trained to be unambiguous and to read back safety-critical information36.
Loss of situational awareness can happen when all of the information is available, but not acted on appropriately, possibly owing to distraction or intense concentration on a specific task (tunnel vision)37. This can be prevented in a team that is actively supporting its members and in which team members feel empowered to voice their concerns32.
Strategies for pharmacist prescribers to improve patient safety
Pharmacist prescribers can apply the principles of human factors to enhance patient safety by focusing on optimising the interaction between people, systems and environments.
Activity: minimising risk of error in a prescribing task
- Identify a prescribing task you would potentially undertake in your own working environment;
- Using the SEIPS model above, list the work-system factors that could affect your ability to carry out that task safely and effectively;
- For each work-system factor listed, think of one strategy that you could implement to reduce the risk of making an error.
Answer guidance: You could consider some of the following proposed strategies, based on the factors described in the SEIPS model30,38–41:
Although it is unlikely that you will be able to implement all the strategies listed above, any that you can implement may help reduce the risk of making an error.

Knowledge check
‘Joint royal college safer use of medicines webinar series’
Want to learn more about human factors and how you can help build robust systems and processes to minimise risk to patients and improve quality of care?
This joint webinar series, hosted by the Royal Pharmaceutical Society, will use real-life examples to help you relate human factors to your day-to-day practice, understand when interventions should be implemented, and be equipped with practical tools and solutions you can use in your practice to improve medication and patient safety.
For more information, and to register, click here.

Expanding your scope of practice
The following resources expand on the information contained in this article.
- World Health Organization (WHO): ‘Medication without harm: WHO global patient safety challenge‘;
- The Human Factor: learning from Gina’s story,
- Clinical Human Factors Group;
- NHS England e-learning for healthcare: Human factors/ergonomics (safety science) for patient safety: level 1;
- National Institute for Health and Care Excellence (NICE): ‘Medicines optimisation: the safe and effective use of medicines to enable the best possible outcomes‘.
- 1.Patient safety. World Health Organization. September 2023. Accessed September 2024. https://www.who.int/news-room/fact-sheets/detail/patient-safety
- 2.Hodkinson A, Tyler N, Ashcroft DM, et al. Preventable medication harm across health care settings: a systematic review and meta-analysis. BMC Med. 2020;18(1). doi:10.1186/s12916-020-01774-9
- 3.To Err Is Human. National Academies Press; 2000. doi:10.17226/9728
- 4.Pharmacist independent prescriber workforce has more than tripled since 2016. Pharmaceutical Journal. Published online 2021. doi:10.1211/pj.2021.1.98014
- 5.Adopting a quality improvement approach to patient safety incidents. Pharmaceutical Journal. Published online 2024. doi:10.1211/pj.2024.1.284831
- 6.The trials and triumphs of pharmacist independent prescribers. Pharmaceutical Journal. Published online 2018. doi:10.1211/pj.2018.20204489
- 7.Rosenthal M, Austin Z, Tsuyuki RT. Are Pharmacists the Ultimate Barrier to Pharmacy Practice Change? Can Pharm J. 2010;143(1):37-42. doi:10.3821/1913-701x-143.1.37
- 8.Improving prescribing practice to ensure patient safety. Pharmaceutical Journal. Published online 2016. doi:10.1211/pj.2016.20201734
- 9.Considering human factors and developing systems-thinking behaviours to ensure patient safety. Clinical Pharmacist. Published online 2018. doi:10.1211/cp.2018.20204352
- 10.Becoming a pharmacist independent prescriber: eight tips for success. Pharmaceutical Journal. Published online 2022. doi:10.1211/pj.2022.1.138994
- 11.Elliott RA, Camacho E, Jankovic D, Sculpher MJ, Faria R. Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Qual Saf. 2020;30(2):96-105. doi:10.1136/bmjqs-2019-010206
- 12.Dornan T, Ashcroft D, Heathfield H, et al. An in Depth Investigation into Causes of Prescribing Errors by Foundation Trainees in Relation to Their Medical Education. EQUIP Study. General Medical Council; 2009. Accessed September 2024. https://www.gmc-uk.org/-/media/documents/FINAL_Report_prevalence_and_causes_of_prescribing_errors.pdf_28935150.pdf
- 13.Investigating the prevalence and causes of prescribing errors in general practice. General Medical Council. May 2012. Accessed September 2024. https://www.gmc-uk.org/about/what-we-do-and-why/data-and-research/research-and-insight-archive/investigating-the-prevalence-and-causes-of-prescribing-errors-in-general-practice
- 14.Avery AJ, Ghaleb M, Barber N, et al. The prevalence and nature of prescribing and monitoring errors in English general practice: a retrospective case note review. Br J Gen Pract. 2013;63(613):e543-e553. doi:10.3399/bjgp13x670679
- 15.Lewis PJ, Dornan T, Taylor D, Tully MP, Wass V, Ashcroft DM. Prevalence, Incidence and Nature of Prescribing Errors in Hospital Inpatients. Drug Safety. 2009;32(5):379-389. doi:10.2165/00002018-200932050-00002
- 16.Baqir W, Crehan O, Murray R, Campbell D, Copeland R. Pharmacist prescribing within a UK NHS hospital trust: nature and extent of prescribing, and prevalence of errors. Eur J Hosp Pharm. 2014;22(2):79-82. doi:10.1136/ejhpharm-2014-000486
- 17.Turner E, Kennedy MC, Barrowcliffe A. An investigation into prescribing errors made by independent pharmacist prescribers and medical prescribers at a large acute NHS hospital trust: a cross-sectional study. Eur J Hosp Pharm. 2020;28(3):149-153. doi:10.1136/ejhpharm-2019-002074
- 18.What are clinical human factors? Clinical Human Factors Group (CHFG). Accessed September 2024. https://chfg.org/what-are-clinical-human-factors/
- 19.Human Factors in Healthcare: A Concordat from the National Quality Board. NHS England. Accessed September 2024. https://www.england.nhs.uk/wp-content/uploads/2013/11/nqb-hum-fact-concord.pdf
- 20.Carayon P, Xie A, Kianfar S. Human factors and ergonomics as a patient safety practice. BMJ Qual Saf. 2013;23(3):196-205. doi:10.1136/bmjqs-2013-001812
- 21.What are ‘Sterile Flight Deck Procedures’? EASA. 2018. Accessed September 2024. https://www.easa.europa.eu/en/faq/19134
- 22.Kapur N, Parand A, Soukup T, Reader T, Sevdalis N. Aviation and healthcare: a comparative review with implications for patient safety. JRSM Open. 2016;7(1):205427041561654. doi:10.1177/2054270415616548
- 23.Federwisch M, Ramos H, Adams SC. The Sterile Cockpit. AJN, American Journal of Nursing. 2014;114(2):47. doi:10.1097/01.naj.0000443777.80999.5c
- 24.Sullenberger C. Chesley B. “Sully” Sullenberger: Making safety a core business function. Healthc Financ Manage. 2013;67(10):50-54. https://www.ncbi.nlm.nih.gov/pubmed/24244993
- 25.Reason J. Human error: models and management. BMJ. 2000;320(7237):768-770. doi:10.1136/bmj.320.7237.768
- 26.Prescribing errors in children: why they happen and how to prevent them. Pharmaceutical Journal. Published online 2023. doi:10.1211/pj.2023.1.184013
- 27.Reason J. Human Error. Published online October 26, 1990. doi:10.1017/cbo9781139062367
- 28.Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ. 1998;316(7138):1154-1157. doi:10.1136/bmj.316.7138.1154
- 29.Yorkshire Contributory Factors Framework. Improvement Academy. 2022. Accessed September 2024. https://improvementacademy.org/resource/yorkshire-contributory-factors-framework/
- 30.Carayon P, Schoofs Hundt A, Karsh BT, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15(suppl 1):i50-i58. doi:10.1136/qshc.2005.015842
- 31.SEIPS quick reference guide and work system explorer. NHS England. August 2022. Accessed September 2024. https://www.england.nhs.uk/wp-content/uploads/2022/08/B1465-SEIPS-quick-reference-and-work-system-explorer-v1-FINAL-1.pdf
- 32.Brennan PA, Oeppen RS. The role of human factors in improving patient safety. Trends Urol & Men’s Health. 2022;13(3):30-33. doi:10.1002/tre.858
- 33.Carling J, Janes G, Murray D. Using human factors to enhance drug prescribing safety. Contemporary Ergonomics and Human Factors. Accessed September 2024. https://publications.ergonomics.org.uk/uploads/Using-human-factors-to-enhance-drug-prescribing-safety.pdf
- 34.Sugden C, Athanasiou T, Darzi A. What Are the Effects of Sleep Deprivation and Fatigue in Surgical Practice? Seminars in Thoracic and Cardiovascular Surgery. 2012;24(3):166-175. doi:10.1053/j.semtcvs.2012.06.005
- 35.Tool: I’M SAFE Checklist. Agency for Healthcare Research and Quality. June 2023. Accessed September 2024. https://www.ahrq.gov/teamstepps-program/curriculum/situation/tools/safe.html
- 36.Hardie JA, Oeppen RS, Shaw G, Holden C, Tayler N, Brennan PA. You Have Control: aviation communication application for safety-critical times in surgery. British Journal of Oral and Maxillofacial Surgery. 2020;58(9):1073-1077. doi:10.1016/j.bjoms.2020.08.104
- 37.Brennan PA, Holden C, Shaw G, Morris S, Oeppen RS. Leading article: What can we do to improve individual and team situational awareness to benefit patient safety? British Journal of Oral and Maxillofacial Surgery. 2020;58(4):404-408. doi:10.1016/j.bjoms.2020.01.030
- 38.In practice: Guidance for pharmacist prescribers . The General Pharmaceutical Council. January 2024. Accessed September 2024. https://assets.pharmacyregulation.org/files/2024-01/in-practice-guidance-for-pharmacist-prescribers-february-2020.pdf
- 39.Communication techniques for prescribing. Pharmaceutical Journal. Published online 2023. doi:10.1211/pj.2023.1.198986
- 40.ISMP Medication Safety Alert. ISMP. October 2023. Accessed September 2024. https://www.ismp.org/sites/default/files/newsletter-issues/20231005.pdf
- 41.Wake N. How to ensure that you report medication incidents effectively. The Pharmaceutical Journal . June 2013. Accessed September 2024. https://pharmaceutical-journal.com/article/ld/how-to-ensure-that-you-report-medication-incidents-effectively