
Shutterstock.com
After reading this article, you should be able to:
- Understand the importance of accurate and comprehensive patient notes;
- Learn the most important components of well-structured patient notes;
- Develop effective documentation skills to ensure clarity and consistency in patient notes.
Introduction
Patient notes are an integral part of clinical practice and a vital communication tool among healthcare professionals. As the role of the pharmacist evolves, with increasing involvement in prescribing and patient care, the ability to write clear, concise and accurate patient notes is of utmost importance.
Pharmacists need to be well versed in writing patient notes to ensure continuity of care by documenting medical history, medications, allergies and clinical findings. These notes facilitate personalised care and serve as a future reference for the wider multidisciplinary team (MDT). They also aid in medication management, allowing pharmacists and other clinicians to track dosages, adverse effects, changes, and adherence. Patient notes enable positive collaboration with healthcare teams, ensuring all professionals are informed about the patient’s condition, treatment plan and concerns. Additionally, accurate and comprehensive notes fulfil legal and regulatory requirements, maintaining confidentiality and adhering to standards, while providing a record for audits and disputes. This article aims to provide practical insights on writing effective patient notes, including what to include, what to avoid and the clinical impact of good documentation.
According to the General Medical Council’s guidelines on good medical practice, it is imperative to maintain clear, accurate, and legible records[1]. Clinical records serve several purposes:
- To record a concise account of the consultation, document actions, steps taken and outcomes;
- To inform fellow colleagues who may encounter the patient in the future, thereby enabling continuity of care;
- To offer valuable evidence if quality of care is ever called into question.
All records that contain personal information about patients, colleagues or others must be stored securely and in line with data protection law requirements[2,3].
What are patient notes?
Patient notes are written accounts that capture essential details of patient encounters. They are also known as medical records or clinical documentation. These records serve as a comprehensive reference for healthcare providers, documenting patient history, assessments, treatments and follow-up plans. They also serve as a legal and ethical record of patient encounters and are essential for continuity of care, communication, research and quality improvement initiatives[2,4].
With increased access to patient records in both the primary and secondary care sector, pharmacists can contribute to effective care coordination and enable seamless transitions between healthcare providers. Patient notes can take various forms, including handwritten notes, electronic medical records, or a combination of both. Regardless of the format, the principles of good documentation remain the same.
The clinical impact of patient notes
Between April 2021 and March 2022, the National Patient Safety Agency received more than 102,059 reports concerning documentation failures in Great Britain[5].
Well-written patient notes have significant clinical implications, impacting patient care in the following ways:
Continuity of care
Comprehensive and accurate patient notes ensure smooth transitions between healthcare providers, allowing for a consistent understanding of the patient’s medical history, ongoing treatments and future management plans. This promotes seamless care coordination and reduces the risk of errors or duplicated efforts.
Example: Decision-making around medicines optimisation can be improved if pharmacists can see the original rationale for prescribing.
Communication and collaboration
Patient notes facilitate effective communication among healthcare professionals, enabling seamless interdisciplinary collaboration and ensuring optimal patient outcomes. Accessible and comprehensive patient notes ensure all team members are aware of the patient’s condition, treatment plan and any changes made to the medication regimen. This enhances interdisciplinary communication, reduces the risk of miscommunication and improves overall patient outcomes. This collaborative approach also promotes coordinated and comprehensive care for the patient, leading to better outcomes and improved patient safety.
Example: Records can support communication with the pharmacist, clarifying any medicine-related questions or sharing updates on the patient’s condition.
Legal and ethical considerations
Legally and ethically sound patient notes provide a crucial documentation trail, aiding in legal disputes, research, audits and quality improvement initiatives. In legal disputes, patient notes serve as evidence of the care provided and the decision-making process. Additionally, patient notes contribute to research, audits and quality improvement initiatives, allowing for data analysis and identifying areas for improvement in patient care.
Example: If a patient files a complaint against a pharmacist alleging a medication error, the pharmacist’s detailed patient records play a crucial role. These records serve as valuable evidence during the investigation, allowing the pharmacist to provide a clear account of events, actions taken and information provided to the patient. The thorough documentation establishes the pharmacist’s adherence to professional standards and supports their defence.
Patient safety and quality of care
Clear and concise patient notes contribute to patient safety by minimising errors, improving medication management, and enhancing the overall quality of care delivered. Accurate documentation of medication-related information helps prevent medication errors and adverse events.
Example: Documenting critical information, such as allergies, adverse drug reactions and drug interactions, allows healthcare professionals to identify potential risks and take appropriate actions to prevent adverse events.
What to include in patient notes
Patient notes should be made promptly. Each entry must include the precise date, time and your identity. When you are likely to be involved in prescribing for the patient, the notes should also cover the following five points.
1. Presenting complaint and history
Begin by documenting the patient’s presenting complaint and relevant medical history. This should encompass both normal and abnormal observations. Details such as allergies, current medications, past medical conditions and surgical history should be included. This information provides important context for the patient’s current condition and helps guide subsequent assessment and treatment. Include all pertinent medical history and examination findings.
Example: ‘Patient presents with a complaint of persistent cough and reports a history of asthma and current use of salbutamol inhaler.’
2. Objective findings
Record objective observations, which can include basic observations (i.e. respiratory rate, temperature, heart rate, blood pressure), recent pathology results, physical examination findings and any other relevant clinical data. This information provides an objective basis for the assessment and helps monitor the patient’s progress over time.
Example: ‘Blood pressure: 120/80mmHg, heart rate: 80bpm, and oxygen saturation: 98% on room air.’
3. Assessment and diagnosis
Write a concise assessment based on the information gathered, including a working diagnosis or differential diagnosis to rule out potential conditions. This section reflects the pharmacist’s professional judgment and clinical reasoning.
Example: ‘Based on the patient’s symptoms and history, the preliminary assessment suggests exacerbation of asthma.’
4. Medication management
Note all information provided to the patient during the consent process, such as discussions of various treatment options and the accompanying risks.
Document the recommended or prescribed medicines, including dosage, frequency, route of administration and any advice given to the patient. Clearly indicate any changes made to the patient’s medication regimen, including new prescriptions, adjustments or discontinuations.
Example: ‘The patient’s current use of medication was not suitably optimised to justify up-titration of the treatment regimen. In line with the patients’ presenting complaint, current medication use and SIGN/BTS guidelines the patient was therefore, advised to use salbutamol inhaler (two puffs every four to six hours, as needed) and to continue current maintenance inhaler (fluticasone 100mcg, twice daily). The patient was counselled on the appropriate use of inhalers and adherence to the regimen to accurately measure the outcomes.’
5. Follow-up plan and monitoring
Clearly outline the next steps or follow-up plan, including any referrals, diagnostic tests and patient education. Provide a timeline for follow-up appointments and specify the goals or expected outcomes of the treatment plan.
The notes should clearly state the decisions reached and mutually agreed-upon actions. Include the patient’s concerns, preferences, and expressed wishes — this can be particularly valuable if their capacity becomes compromised at a later stage.
Example: ‘Advise the patient to schedule a follow-up appointment in one week to reassess symptoms and evaluate treatment efficacy. The patient expressed concern with continued use of a steroid base treatment and the potential long-term effects. The side effects, evidence base for recommendation with the patient. The patient was reassured with further information on long term outcome and benefit of appropriate treatment.’
Similarly, where you are involved in a structured medication review you would also take a methodical and systematic approach and document recommendations and interventions. This will include a record of the pharmacist’s recommendations and interventions made during the review. This may include adjusting dosages, suggesting alternative medications, or providing counselling on medication adherence, potential side effects or drug interactions. The notes should also have a clear plan for any follow-up or monitoring, including any recommended laboratory tests, appointments or interventions discussed and agreed with the patient. The notes should clearly specify the timeframe for the follow-up and who will be responsible for ensuring it is carried out.
Different settings
Although the principles of what to document in patient notes are universal, there are some additional points to consider when looking at specific settings.
In a hospital ward, patient notes must contain specific information, including the patient’s precise location (ward number), their unique hospital identifier, and the details of the attending clinician (including their role and registration information). Currently, most UK trusts are working towards having electronic patient records. These bring all patients’ details together in one place, which allows quick access for clinicians, improves efficiency and reduces the chance of errors. This also ensures any changes are easily tracked and streamlines how records are made and stored. However, handwritten notes are still commonly used in this setting. Should any mistakes occur in these records, make clear corrections, counter-sign them and provide the date for the new entry.
In general practice, notes are typically recorded electronically using software such as EMIS (Egton Medical Information Systems) or SystemOne. If errors are made in these entries, it is essential to create new entries that explicitly reference and address the amendments made. These electronic records maintain a transparent audit trail, enabling the tracking of any modifications.
What not to include in patient notes
While it is important to be thorough, pharmacists must take care to maintain professionalism, accuracy and clarity.
1. Unnecessary personal opinions
Avoid including personal opinions, subjective biases, or irrelevant information that may cloud the accuracy and objectivity of the patient record. The account should remain factual and focus on evidence-based information. Do not include personal impressions that may be misconstrued in any way. Remember, these notes are to be used by other clinicians and could be presented as a legal document in court[6].
2. Incomplete or vague descriptions
Ensure that your notes provide comprehensive and detailed information, and avoid ambiguous language or incomplete descriptions that can be misinterpreted. Use clear and concise language to convey your observations and assessments. This ensures that anyone who reads your account can treat the patient without any doubt of what has happened before.
3. Inappropriate language or abbreviations
Use clear and concise language. Avoid jargon and acronyms that may not be universally understood. If using abbreviations, ensure they are well-known and clearly defined. Avoid using slang or informal language that may compromise the professionalism of the notes.
4. Unprofessional language or tone
Maintain a professional tone throughout the patient note, demonstrating respect, empathy and cultural sensitivity. Avoid derogatory or judgmental language that may negatively affect patient care and rapport.
Conclusion
Writing effective patient notes is a critical skill for pharmacists. It enhances patient care, communication and safety. By following the principles outlined in this guide, pharmacists can create comprehensive, accurate and concise patient notes that contribute to patient-centred care and improved healthcare outcomes[7].
Example 1: Poor patient notes
This example illustrates poor record-keeping practices. The presenting complaint is suspected to be a urinary tract infection (UTI), but the history provided is vague. The prescription of medication and mention of further investigation and a fit note are noted. However, there are several crucial details missing.
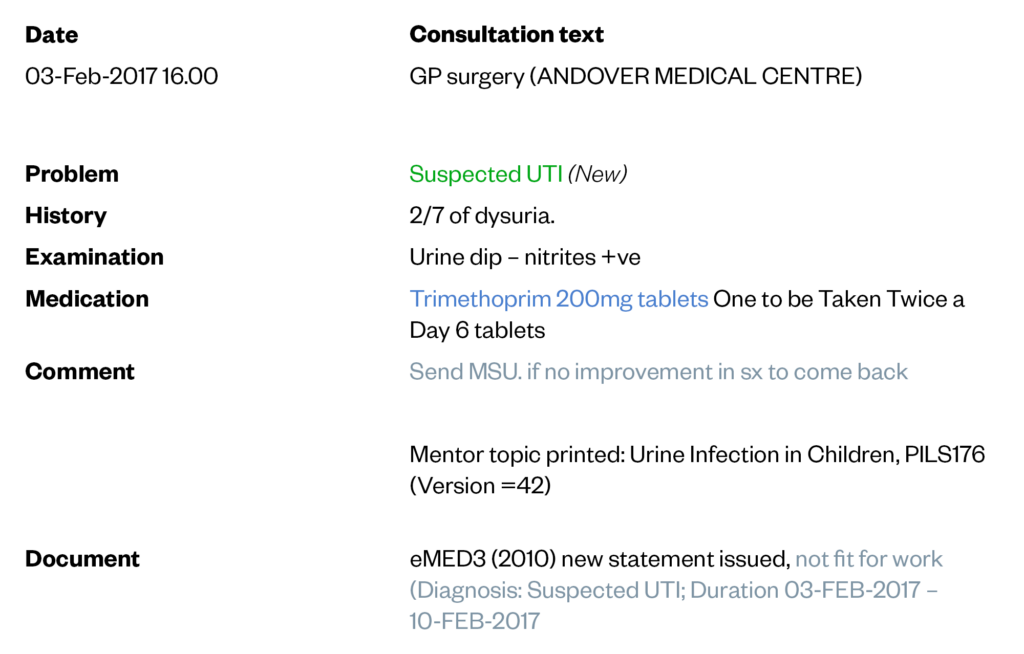
The Pharmaceutical Journal
For instance, is the patient aware of what steps to take if their symptoms worsen? The record simply advises the patient to return if there is no improvement. It is important to clarify the specific signs of non-improvement and establish when and whom they should contact. In terms of the examination, while a urine dip test was performed, there is no documentation regarding the GP checking the patient’s temperature or pulse rate. Consequently, we can assume that these were not conducted.
There are important questions that need to be addressed when following up or reviewing this patient if they return in a few days. Without a comprehensive record, it is difficult to determine how the patient was examined and what information they were provided. We cannot assume that the patient will remember the details shared by the GP.
Example 2: Good patient notes
By comparison, another clinician has significantly improved the documentation by providing more detailed information.
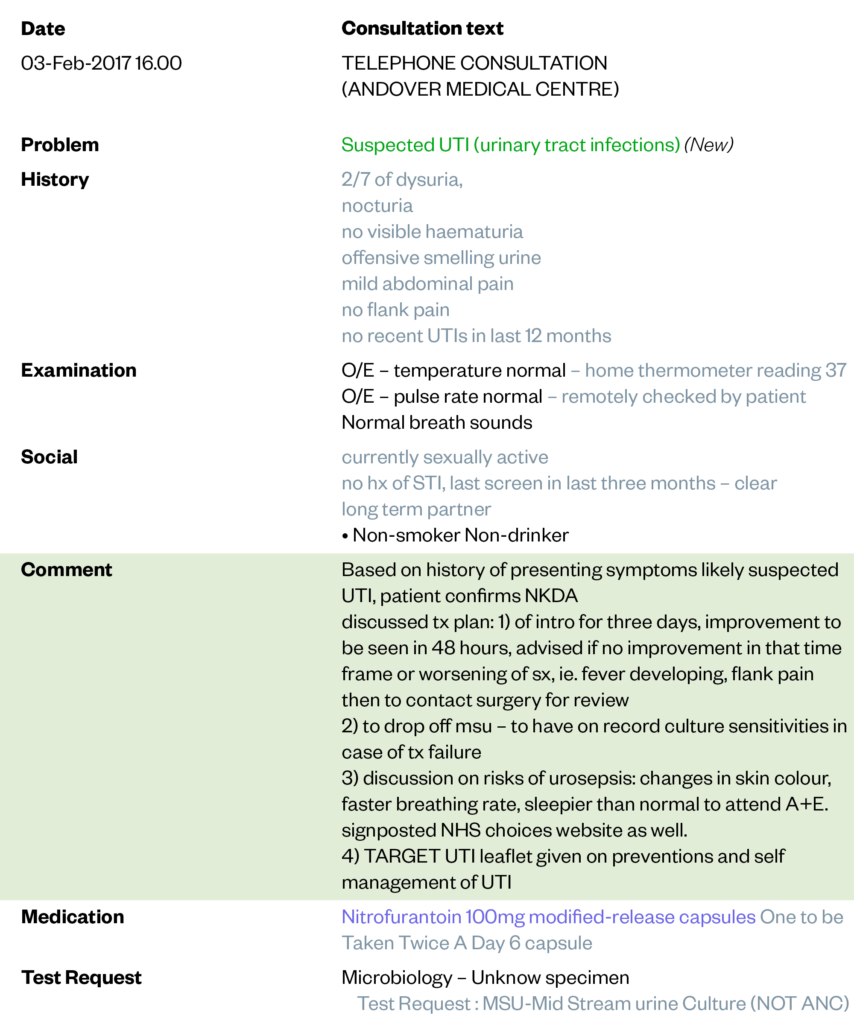
The Pharmaceutical Journal
First, it is clearly stated that the consultation took place over the telephone. The presenting complaint, suspected to be a UTI, is now described in greater depth. Additionally, there is additional information about the history of the presenting complaint, and the type of examination that was conducted remotely. The clinician explicitly notes that the patient performed the examination themselves. The patient’s social history is also included, as it is relevant to the case.
Moving on to the discussion between the patient and the clinician, a clear plan has been established. The clinician addresses the length of treatment, when improvement can be expected, and specific symptoms to watch out for in the event that treatment fails. Furthermore, guidance is provided on which healthcare setting the patient should seek depending on their symptoms, whether it be a return visit to the surgery for a review with a clinician or attending the emergency department.
Recognising the importance of patient understanding and recall, the clinician has also provided the patient with additional information to refer to in case they forget what was discussed during the consultation.
The notes in Example 2 are significantly better than in Example 1. The clinician has effectively demonstrated the proper way to document consultation notes, ensuring that all relevant information is captured for future reference and continuity of care.
Box: Activity to complete
Please take a moment to review the patient record example provided, considering the issues we have discussed regarding record keeping.
As the clinician responsible for the follow-up, consider the following points:
- What additional information would you require in the record?
- If the patient returns a week later due to unsuccessful treatment, do you have sufficient information in the record to facilitate a thorough follow-up?
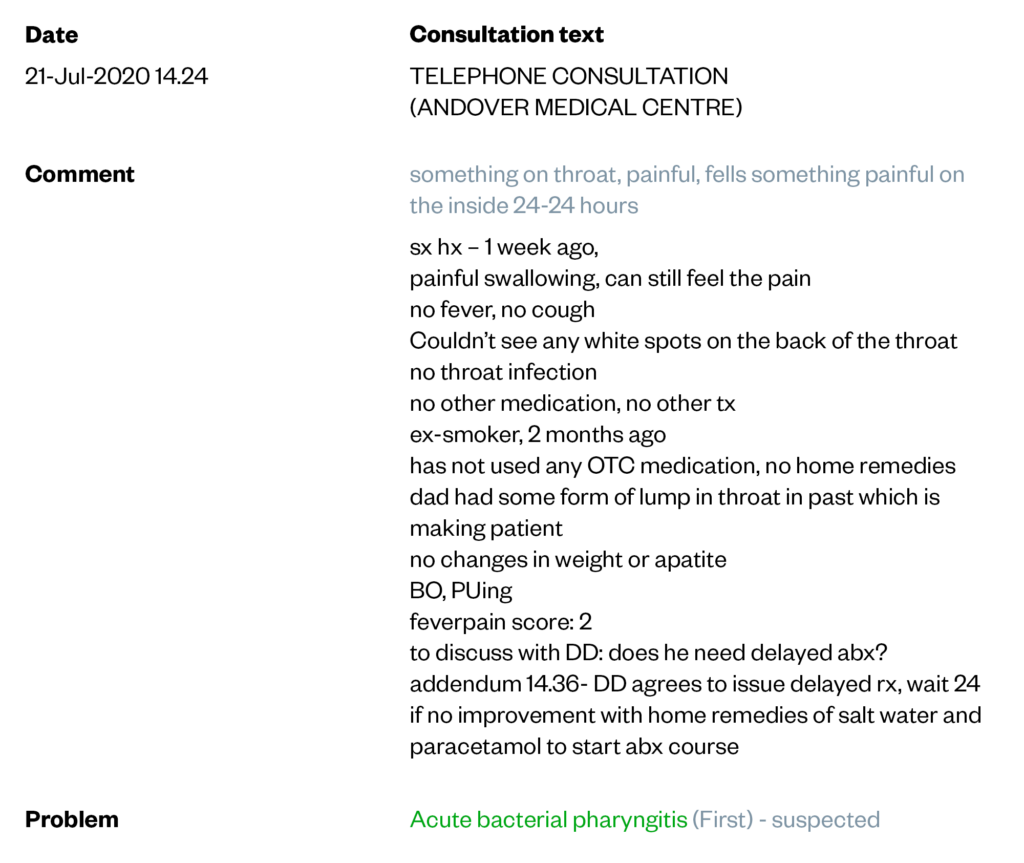
The Pharmaceutical Journal
- 1Keeping Records. General Medical Council. 2023.https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/protecting-children-and-young-people/keeping-records (accessed Jun 2023).
- 2Records Management Code of Practice. NHS England. 2023.https://transform.england.nhs.uk/information-governance/guidance/records-management-code/ (accessed Jun 2023).
- 3Generic medical record keeping standards. Royal College of Physicians. 2015.https://www.rcplondon.ac.uk/projects/outputs/generic-medical-record-keeping-standards (accessed Jun 2023).
- 4An Essential Guide to Medical Records. Medical Protection. 2017.https://www.medicalprotection.org/uk/articles/an-mps-essential-guide-to-medical-records (accessed Jun 2023).
- 5National Patient Safety Incident Reports up to June 2022. NHS England. 2022.https://www.england.nhs.uk/publication/national-patient-safety-incident-reports-up-to-june-2022/ (accessed Jun 2023).
- 6Chowdhury M, Peteru S, Askandaryan A, et al. Incomplete Medical Charts: Impacts And Possible Solutions. Eur. Psychiatr. 2022;65:S747–S747. doi:10.1192/j.eurpsy.2022.1930
- 7Data Protection Act 2018. . 2018.https://www.legislation.gov.uk/ukpga/2018/12/contents/enacted (accessed Jun 2023).


