Shutterstock.com
An experimental drug has been shown to reduce cognitive decline in patients with Alzheimer’s disease (AD) in what has been described as an ‘historic moment’ in dementia research.
According to data from its manufacturer Eisai, a phase III trial of lecanemab successfully slowed cognitive decline in participants as early as six months after they began taking the drug.
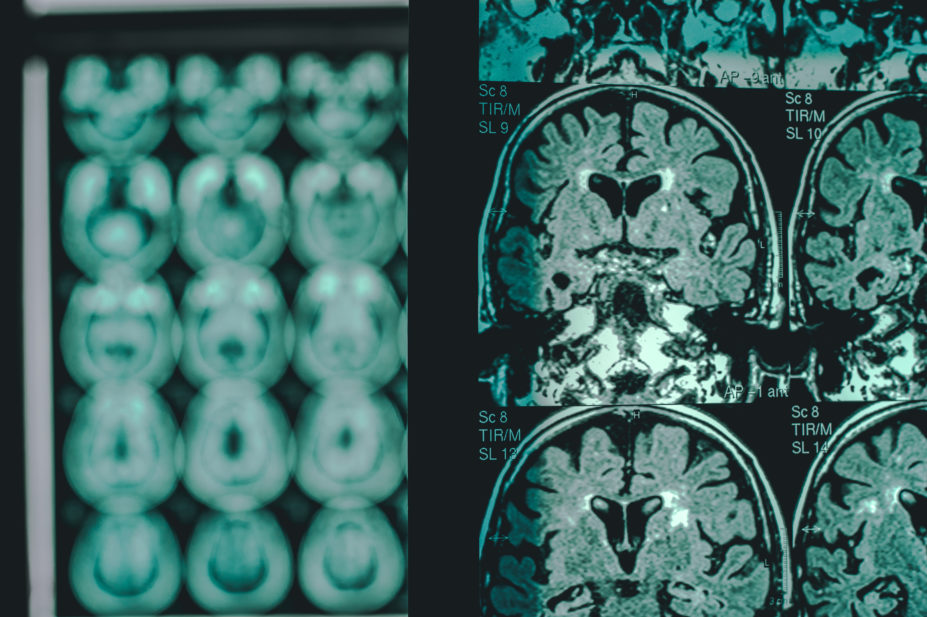
Previously known as BAN2410, lecanemab is designed to target and clear the build-up of the amyloid protein within the brain, which often indicates the early stage of AD.
The phase III trial involved 1,795 people with early-stage AD and mild cognitive impairment resulting from AD. Participants received either a bi-weekly infusion of lecanemab or a placebo over 18 months.
The results, which have not yet been fully published, show that patients taking lecanemab deteriorated 27% more slowly than those who took placebo, resulting in reduced memory decline and better cognitive function over the 18-month period, helping people manage day-to-day activity better.
Susan Kohlhaas, director of research at Alzheimer’s Research UK, said the trial was the first phase III trial of a AD drug that had slowed cognitive decline “in a generation”.
“This is a historic moment for dementia research,” she said.
“These results show that lecanemab slows the progression of memory and thinking problems in people with early AD, demonstrating a major breakthrough in dementia research.”
Commenting on the trial results, Rob Howard, professor of old age psychiatry at University College London, said: “It’s really fantastic news. For the first time, someone has actually shown convincingly, that they can change the course of AD.”
The researchers found that lecanemab made a small but statistically significant impact on cognitive decline in people with early-stage disease.
Howard added: “What’s happened up until now is there’s been lots of what looked like promising steps, but every time we’ve put our foot on them, they’ve crumbled. This is the first actual step we’ve taken up that cliff that’s secure, and that’s going to help us scale the rest of it, but we’re not at the top.”
The drug has not been approved in the UK and was shown to cause substantial side effects in the trial, the most common of which were headaches and swelling in the brain, known as amyloid-related imaging abnormalities. The headaches were experienced by 17% of those who received lecanemab.
As a result, Howard said the benefit-risk equation for lecanemab will be complicated.
“The kind of sting in the tail is that the magnitude of the treatment effect is really small. There are going to be some very difficult conversations with regulators and also with the people who fund services. It’s quite expensive, difficult to give and it has a not insignificant series of side effects.
[The National Institute for Health and Care Excellence has] got a really difficult job to do because [it has] to balance, effectiveness, cost-effectiveness and the effects that funding this would have on services and the rest of the NHS.”
However, he added: “I’ve been in this field for 30 years, waiting for something like this. And despite my rationalism about the difficulties, yesterday was a very exciting day for me.”


