Brigette Supernova / Alamy Stock Photo
Researchers are calling for a change to national guidance after a study has suggested that combination treatment could increase the chance of resolution after a missed miscarriage, reducing the need for surgery.
Misoprostol, a prostaglandin analogue, is commonly used for the medical management of miscarriage to induce myometrial contractions to aid the expulsion of pregnancy tissue. However, according to the researchers, in 15%–40% of cases, women require an additional dose of misoprostol and, in some cases, a surgical procedure is required to complete the miscarriage.
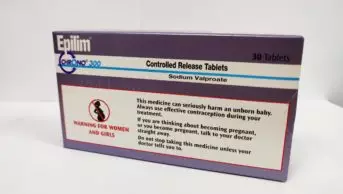
Mifepristone, a steroidal anti-progesterone, can be used to augment the effect of misoprostol by priming the myometrium before prostaglandin exposure, the researchers said. However, current National Institute for Health and Care Excellence (NICE) guidance recommends against its use in missed miscarriage, and instead advises to use a single dose of 800 micrograms of misoprostol alone.
The researchers, from the University of Birmingham, set out to investigate whether treatment with mifepristone in combination with misoprostol would result in a higher rate of completion of missed miscarriage compared with misoprostol alone.
A missed miscarriage is diagnosed when a non-viable pregnancy is identified on an ultrasound scan during the first 14 weeks. Often in missed miscarriages there are no noticeable symptoms because all pregnancy tissue is retained in the uterus.
The randomised controlled ‘MifeMiso’ trial, published in The Lancet , included 711 women across 28 UK hospitals who had a diagnosis of missed miscarriage in the first 14 weeks of pregnancy.
The women were randomly assigned to receive either a single dose of mifepristone (200mg), followed by a single dose of misoprostol (800 micrograms) two days later, or an oral placebo tablet followed by a single dose of misoprostol (800 micrograms) two days later.
The researchers found that, within seven days, the combination treatment group had a miscarriage resolution rate of 83%, compared with a resolution rate of 76% in the group who received misoprostol alone.
In addition, they recorded fewer incidences of surgical management to complete miscarriage in the combination group (17%), compared with the placebo group (25%).
There was no difference in the incidence of adverse events between the two groups.
“Given the extra strain on the NHS in the COVID-19 pandemic, our findings could have huge benefits if they’re translated into clinical practice,” said Justin Chu from Tommy’s National Centre for Miscarriage Research, who led the study at the University of Birmingham’s Clinical Trials Unit.
“We could achieve better outcomes for women and lower costs for care services. We hope the NICE guidance will be updated in light of this new evidence, so that everyone who needs it has access to the most effective treatment.”
Nuttan Tanna, consultant pharmacist for women’s health and older people at the North West London Hospitals NHS Trust, said that those in obstetrics had been “waiting with interest” for the results of the MifeMiso trial.
“This UK, multi-centre, carefully conducted RCT [randomised controlled trial] with over 700 patients adds to our knowledge and has reported findings that will be welcome — a higher significant resolution rate for women undergoing miscarriage without symptoms in the first 7 days; no difference in incidence of adverse events between the two study cohorts; [and] no deaths reported in either study group,” she said.
“It would be helpful for improved NHS patient care if the NICE guidelines were reviewed and updated,” she added. “This also ensures the NICE evidence base team independently review the MifeMiso results reported.”
However, Tanna said it was important to note that the combination of mifepristone and misoprostol would not be advised in women who have already started expelling pregnancy tissue.
“[In this case] there is no need for the pharmacological/biological pathway function being utilised when providing the mifepristone dose prior to the misoprostol — the main oxytocic ‘inducing contractions’ miscarriage medicine,” she explained.