MATTLPHOTOGRAPHY / ALAMY STOCK PHOTO
Neutralising monoclonal antibodies (mAbs) will be offered to some non-hospitalised patients with COVID-19 from 16 December 2021, according to a rapid policy statement issued by the Medicines and Health products Regulatory Agency (MHRA).
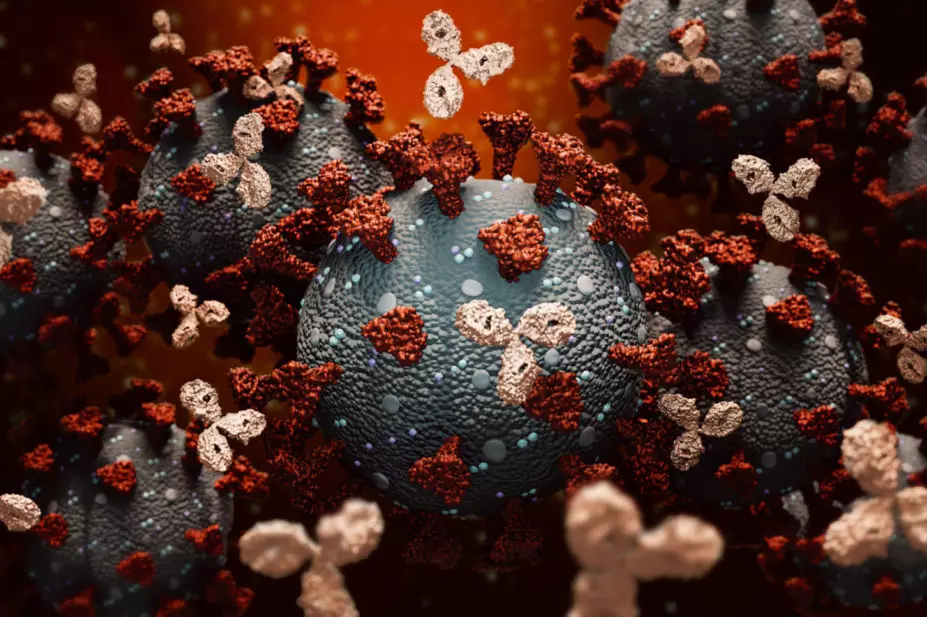
The treatment — which prevents SARS-CoV-2 virus particles entering cells, inhibiting the replication of the virus within the body — has been available to certain patients hospitalised with COVID-19 since September 2021.
Eligible patients in the community will be treated with Ronapreve (Regeneron/Roche), a combination of the mAbs casirivimab and imdevimab. Patients who are not considered suitable for mAb treatment, but who meet all the other conditions, will instead be offered the antiviral treatment molnupiravir.
In England, community mAb treatment will be delivered and managed by COVID-19 medicines delivery units (CMDUs). Every integrated care system in England has established at least one CMDU, with most of these based within hospitals. Local CMDUs will contact eligible patients who have had a positive PCR test to discuss their options and arrange treatment.
The treatment will not be prescribed by GPs or pharmacist independent prescribers in the community.
A spokesperson for the Welsh government told The Pharmaceutical Journal: “Health boards in Wales will be making the combination of casirivimab and imdevimab, and the antiviral molnupiravir, available from later [in December 2021].
“In most cases, eligible patients will be contacted by their health board within 48 hours of their PCR test showing they have COVID-19 to arrange treatment.”
The spokesperson added that health board pharmacists may be involved in undertaking clinical assessments, preparing Ronapreve for administration and supplying molnupiravir.
Patients in the UK will be eligible for community treatment with mAbs if they have had a positive PCR test within the past 72 hours; if they have developed symptoms of COVID-19 within the past week; and if they are part of a cohort considered to be at the highest risk from the virus. The latter includes patients with solid cancers; certain renal and liver diseases; certain immunodeficiencies; sickle cell disease and Down’s syndrome.
The MHRA’s statement also said: “mAbs and oral antivirals significantly improve clinical outcomes in unvaccinated non-hospitalised patients with COVID-19 who are at high risk of progression to severe disease and/or death.”
Raliat Onatade, group chief pharmacist and clinical director for medicines optimisation at Barts Health NHS Trust, said that hospital pharmacists were “integral” to CMDUs.
“Hospital pharmacists’ role is to ensure the correct and appropriate handling and supply of [neutralising mAbs (and oral antivirals) to patients who are referred to the CMDU. This includes storage, preparation, prescription, administration and delivery, according to the clinical commissioning policies and official guidance,” she said.
“We will be ensuring that all eligible patients are able to receive treatment.”
The Pharmaceutical Journal asked the Scottish government for its plans on widening access to mAbs.
Read more: Everything you need to know about the COVID-19 therapy trials


