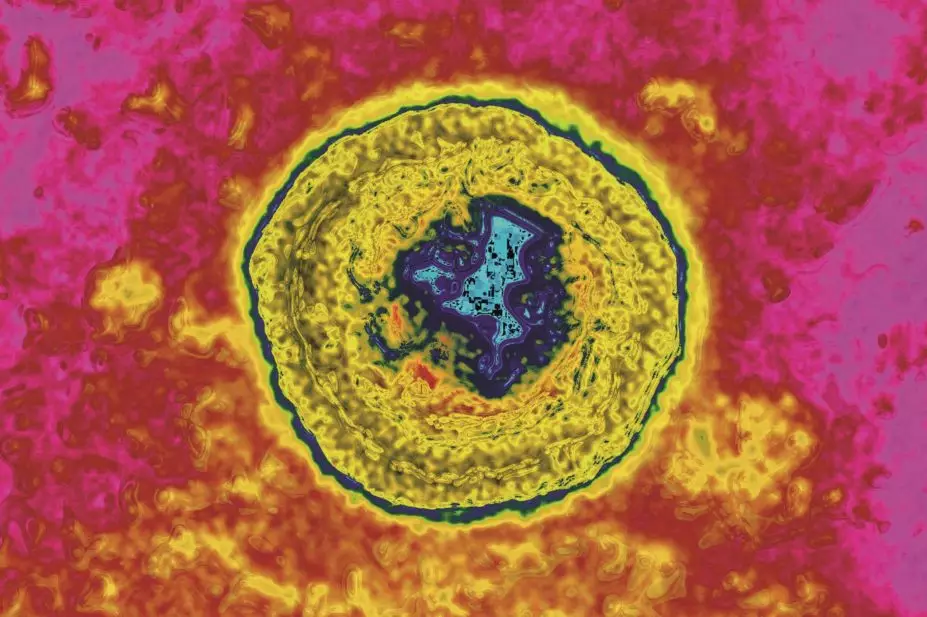
Cavallini James / BSIP / Science Photo Library
Patients with metastatic melanoma in the United States and Europe are set to have a new treatment option after a therapy derived from the herpes simplex virus was approved by the US Food and Drug Administration (FDA) and recommended for approval by the European Medicines Agency (EMA).
Both regulators have recommended talimogene laherparepvec (Amgen’s Imlygic) for the treatment of adults with melanoma that cannot be removed by surgery and has spread, without affecting the bones, brain, lung or other internal organs.
“This approval provides patients and healthcare providers with a novel treatment for melanoma,” says Karen Midthun, director of the FDA’s Center for Biologics Evaluation and Research.
Talimogene is classified by the EMA as an advanced therapy medicinal product (ATMP), which is a therapy for human use based on genes or cells.
The first-in-class medicine is derived from a genetically engineered virus — the herpex simplex virus-1 — that has been designed to infect and kill cancer cells. It is thought to do this in two ways: it enters the tumour cell and uses the cell’s energy stores to replicate, eventually overwhelming the cell and causing it to die; and by producing granulocyte-macrophage colony-stimulating factor (GM-CSF) — a protein produced by macrophages — thereby stimulating the patient’s immune system to recognise and destroy tumour cells. Once an infected tumour cell dies, copies of the virus are released into the patient’s bloodstream to infect more tumour cells. While talimogene can enter healthy cells, it is not able to replicate in these cells so does not kill them.
Paul Workman, chief executive of The Institute of Cancer Research, London, says that viral immunotherapy represents a completely new way of treating cancer, and described the EMA’s recommendation as “extremely exciting”.
“It is not only effective for patients with advanced melanoma, but also promises to have lower rates of side effects than traditional treatments or some other immunotherapies,” he says.
Talimogene will be available as a solution for injection and is injected directly into melanoma lesions. Its efficacy was assessed in a randomised controlled trial, in which 295 patients were treated with talimogene and 141 patients were treated with GM-CSF injected under the skin. Analysis of a subset of patients (249 patients whose disease had not spread to the lung or other internal organs) showed that 25% of patients treated with talimogene had at least a 50% reduction in their tumour lasting at least six months compared with 1% of those treated with GM-CSF.
Overall survival was a secondary endpoint in the trial, and subgroup analyses showed that the effect of talimogene on overall survival was largest in patients where the unresectable melanoma had not spread beyond the skin or lymph nodes.
The EMA’s Committee for Medicinal Products for Human Use (CHMP) issued the recommendation for Imlygic to be granted a marketing authorisation in Europe at its October 2015 meeting, following an assessment by the agency’s Committee for Advanced Therapies (CAT). The CHMP and CAT considered that talimogene is relatively well tolerated in patients with cancer and concluded that the medicine’s benefits outweigh its risks. A follow-up plan to monitor the therapy’s efficacy and safety was agreed by the CHMP and the CAT.
The most common side effects of talimogene are fatigue, chills, fever, nausea, influenza-like illness and injection site pain. The medicine should therefore not be given to individuals with suppressed immune systems.
Over the past three years, several types of targeted treatments, including immunotherapies, BRAF V600 inhibitors and MEK inhibitors, have been shown to improve survival in melanoma and revolutionised its treatment. Talimogene has not yet been compared with these drugs in terms of impact on overall survival.