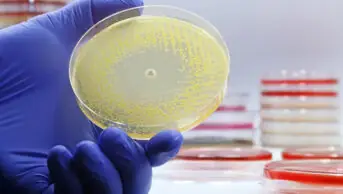
Julian Claxton / Alamy Stock Photo
The rate of Escherichia coli antibiotic resistance has continued to increase despite reductions in unnecessary antibiotic prescribing in general practice in England, a review has found.
The review, published in The Lancet Infectious Diseases on 4 August 2021, looked at the effectiveness of a ‘Quality premium’, introduced by NHS England in 2015/2016, which incentivised clinical commissioning groups with payments of up to £5 per patient to cut back on antibiotic prescribing.
To gain the full payment, primary care clinicians must reduce the number of antibiotic prescriptions by 1% over 12 months and make a 10% reduction in prescriptions of broad-spectrum antibiotics, such as cephalosporins, quinolones and co-amoxiclav.
The reviewers looked at monthly prescribing data from 6,882 GP practices in England between 1 January 2013 and 31 December 2018. This time period was chosen because it included a 27-month pre-implementation period and a 45-month post-implementation period for the ‘Quality premium’ intervention.
At the time the ‘Quality premium’ was introduced, the review says the rate of antibiotic prescribing for all five broad-spectrum antibiotics was increasing at a rate of 0.2% per month. It adds that the rate of resistance to at least one broad spectrum antibiotic was increasing at a rate of 0.1% per month before the ‘Quality premium’ was implemented.
By the end of 2018, the data showed that antibiotic prescribing had reduced by 57% and there was a 12% reduction in the resistance rate across England. However, the authors said that there has remained “a sustained increase in the number of E. coli isolates [that are] resistant to at least one of the broad-spectrum antibiotics”.
They added that the overall trend “was one of attenuation rather than a reversal of previously rising rates of antibiotic-resistant E. coli isolates”.
Study author Shirin Aliabadi, a pharmacist working at the Global Digital Health Unit at Imperial College London, said: “Naturally, the nation’s efforts and resources have shifted to responding to the ongoing COVID-19 crisis but our findings suggest that we must nevertheless consider the growing threat of antimicrobial resistance, which can be a viewed as a silent pandemic.”
The Royal Pharmaceutical Society’s (RPS’s) campaign on antimicrobial stewardship aims to support pharmacists to lead in the appropriate use of antimicrobials.
Jacqueline Sneddon, chair of the Royal Pharmaceutical Society (RPS) Antimicrobial Expert Advisory Group, said: “Pharmacists dispensing or prescribing antibiotics should ensure prescriptions comply with local guidelines.
“Community pharmacists have a key role in providing advice on self-care and symptom relief to patients with common self-limiting infections, which is a big factor in reducing unnecessary use of antibiotics,” she said.
Sneddon added that the RPS website hosts antimicrobial resistance resources for pharmacists, and the Society also runs an education programme “open to pharmacists from all sectors, and a series of webinars focused on infection and antimicrobial use”.
E. coli is the most common drug resistant infection in the UK, with more than half of drug-resistant bacterial blood stream infections in the UK caused by the bacterium.
The UK government has set targets to reduce antimicrobial use in humans by 15% by 2024, and to reduce the number of specific drug-resistant infections in people by 10% by 2025.
READ MORE: Pharmacy’s role in antimicrobial resistance and stewardship