GSK
The first preventive vaccine for malaria has been given the green light by European regulators to protect young children in areas where the disease is prevalent.
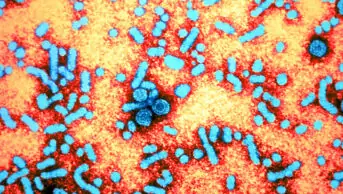
GlaxoSmithKline’s Mosquirix, a vaccine against Plasmodium falciparum and hepatitis B infection, received a positive scientific opinion for its use outside the EU from the European Medicines Agency’s Committee for Medicinal Products for Human Use (EMA’s CHMP) on 24 July 2015.
“The EMEA’s decision marks an extraordinary achievement and huge scientific milestone as we now have the world’s first malaria vaccine, and first vaccine against a human parasite,” says a spokesperson for charity Malaria No More. “Even a partially effective vaccine could prevent millions of malaria cases.”
Mosquirix was assessed under the EMA’s Article 58 regulatory process, which allows a product’s quality, safety and efficacy to be assessed even though it will not be marketed in the EU. The next step is to achieve a recommendation from the World Health Organization (WHO), which will base its decision on feasibility, affordability and cost-effectiveness, particularly in relation to other malaria control measures currently available.
“The Article 58 process for regulatory review is an important collaboration between the EMA and the WHO,” says a WHO spokesperson. “The WHO will provide recommendations on use by November 2015.”
The EMA announcement follows disappointing results from a phase III clinical trial of the vaccine in seven African countries (Burkina Faso, Gabon, Ghana, Kenya, Malawi, Mozambique and Tanzania) in a study published in The
Lancet
[1]
on 24 April 2015. The data showed the vaccine only led to modest protection; it protected 56% of children aged 5–17 months from a first or only attack of malaria, but only 31% of children aged 6–12 weeks, with a decline in efficacy after a year.
“This vaccine is not the game changer that children at risk of dying from malaria need,” says Martin De Smet, leader of Médecins Sans Frontières’ (MSF) malaria working group. “The efficacy of the vaccine is disappointing, especially as there is no significant protection against severe malaria in infants.”
The vaccine will have to be given outside of the routine immunisation schedules, and requires a booster, which will pose a compliance challenge. The vaccine also needs to be used with other measures, such as insecticide-treated bed nets, indoor spraying, testing and treatment, to help ensure prevention and treatment of malaria in people of all age groups.
“Nevertheless, the vaccine still reduces malaria episodes by about 30%,” says De Smet. “MSF and the global community are in desperate need of additional, affordable tools to prevent malaria, especially for areas with high year-round malaria transmission. We therefore cannot afford to not consider and make use of an additional tool, even if it’s highly imperfect.”