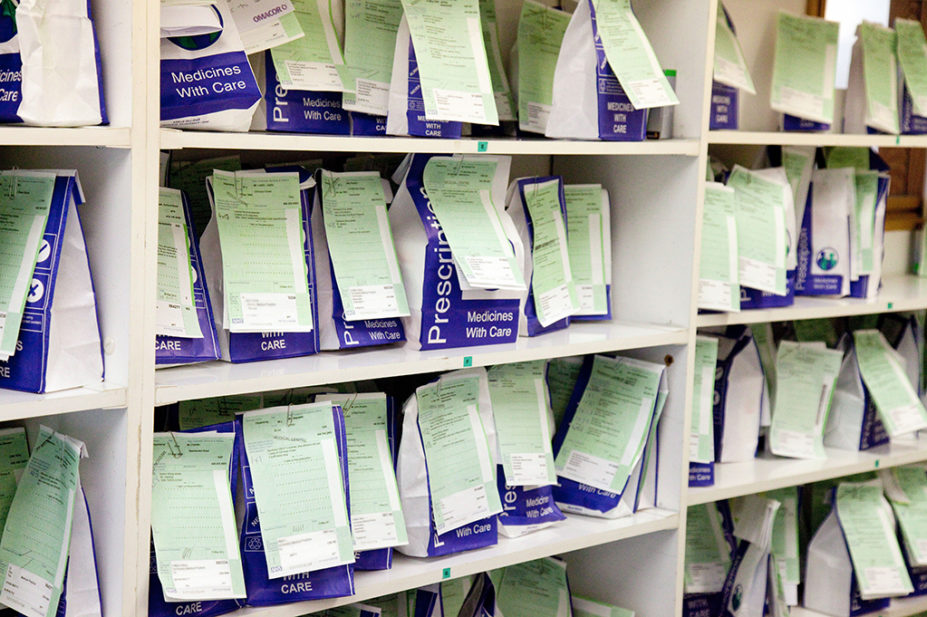
Kumar Sriskandan / Alamy Stock Photo
Pharmacies will provide a national contraception management service and the emergency care pharmacy referral scheme will be expanded, following agreement on the final two years of the current community pharmacy contract, but plans for an English version of a ‘Pharmacy First’ walk-in consultation service appear to have been shelved.
However, the delayed agreement for the remaining two years of the ‘Community Pharmacy Contractual Framework: 2019 to 2024‘, which was announced on 22 September 2022, will mean extra funding for the sector.
The agreement also says that transitional payments — which were introduced when the contract was first agreed in 2019 and are worth around £70m per year — will now be continued until the end of the contract, and a £100m excess margin write-off will mean an increase in Drug Tariff prices, meaning that pharmacies will get to keep £100m that they would otherwise have had to repay to government.
In October 2021, Sajid Javid, then health and social care secretary, said he had asked his department to look into setting up a national minor ailments scheme similar to Scotland’s ‘Pharmacy First’ service, through which 3.3 million consultations were carried out in its first two years.
Speaking at the local pharmaceutical committees conference on 22 September 2022, Janet Morrison, chief executive of the Pharmaceutical Services Negotiating Committee (PSNC), said: “All of the committee members at the PSNC feel hugely frustrated and angry about the refusal of government and the NHS to move away from the five-year ‘Community Pharmacy Contractual Framework’ but it’s also our belief that accepting this and bringing the deal to a close now is a better option than rejecting it. We could have made a stand now, but at the cost of that £100m.
“We are still pressing for a new ‘Pharmacy First’ service, not least because we know that will help the secretary of state and the prime minister to deliver on their aspirations to improve access to general practice and as a frontline to the NHS.”
On the same day, health secretary Thérèse Coffey gave details in a speech to MPs in the House of Commons of the government’s ‘Plan for Patients‘.
In a press release released alongside Coffey’s speech, the Department for Health and Social Care (DHSC) said: “Pharmacies will help ease pressures on GPs and free up time for appointments by managing and supplying more medicines such as contraception without a GP prescription, which could free up to 2 million general practice appointments a year, and taking referrals from emergency care for minor illnesses or symptoms, such as a cough, headache or sore throat.”
Pharmacies across seven primary care networks began a year-long oral contraceptive management pilot in September 2021, allowing people who were already using hormonal oral contraceptives to obtain a repeat supply from their community pharmacy.
From 11 January 2023, this will be expanded to all community pharmacies in England, enabling community pharmacists to provide ongoing management, via a patient group direction (PGD), of routine oral contraception that was initiated in general practice or a sexual health clinic. The fees for each consultation will be £18, plus a set-up fee of £900.
From 4 October 2023, subject to positive evaluation, community pharmacists will also be able to initiate oral contraception via a PGD, and provide ongoing clinical checks and annual reviews.
Also, from March 2023, the ‘Community Pharmacist Consultation Service‘ (CPCS) will expand to enable urgent and emergency care settings to refer patients to a community pharmacist for a consultation for minor illness or urgent medicine supply. The fee for this service will be the existing CPCS fee of £14.
In the new ‘Plan for Patients’, the DHSC also said: “We will look to go further on enabling pharmacists with more prescribing powers and making more simple diagnostic tests available in community pharmacy.” When asked what this meant by The Pharmaceutical Journal, the department could not provide any further details.
Commenting on the contract agreement and the health secretary’s announcement, Nick Kaye, vice chair of the National Pharmacy Association, said his organisation was “bitterly disappointed and concerned” that no extra funding for community pharmacy would be available.
“The life is being choked out of independent pharmacy businesses by the continuation of a fundamentally under-resourced contract in England,” he said.
“The £100m write-off on so-called ‘excess margin’ goes a small way to recognising the current dire financial circumstances, but a clawback of any amount under this kind of pressure would surely be totally unreasonable.”
Meanwhile, a spokesperson for the Company Chemists’ Association described the health secretary’s announcement as “a positive step forward”.
“However, we are concerned that the current financial pressures, and the chronic shortage of pharmacists available to work in community pharmacy, could limit the sector’s ability to fully support the secretary of state’s ambitions at this time,” they said.
Thorrun Govind, chair of the Royal Pharmaceutical Society’s English Pharmacy Board, commented: “To ensure patients get the most out of the NHS it’s important they receive care in the right place.
“A ‘Pharmacy First’ approach in England, where people can go directly to a community pharmacy to treat a minor health problem, would improve access by patients to the care they need and better manage demand right across primary care services.”


