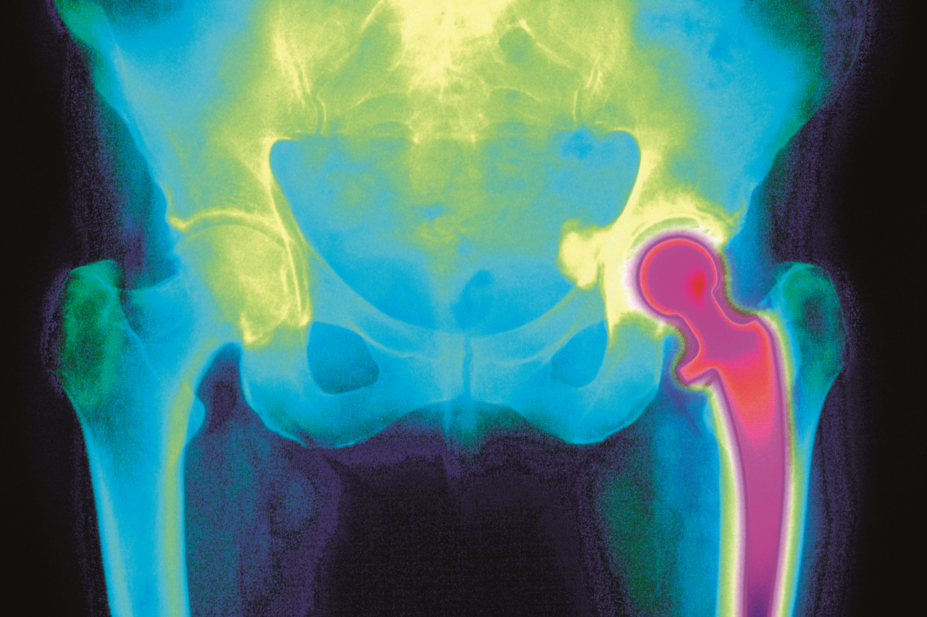
Mehau Kulyk / Science Photo Library
Multimodal pain management is commonplace after joint replacement surgery. However, there is limited evidence to inform the optimal number of analgesics to be used.
In Anesthesiology (online, 2 March 2018), researchers used database records from 2006–2016 on 512,393 people who underwent total hip arthroplasty and 1,028,069 who underwent total knee arthroplasty and grouped them according to whether they were given opioids only or opioids plus one, two or more than two additional modes of analgesia[1]
. Analgesic modes included opioids, peripheral nerve blocks, paracetamol, steroids, gabapentin/pregabalin, non-steroidal anti-inflammatory drugs, cyclooxygenase-2 inhibitors and ketamine.
Overall, 86% of patients received multimodal pain management. The researchers found a stepwise increase in beneficial effects as the number of analgesic modes increased. For example, hip arthroplasty patients who received more than two additional modes of analgesia had 19% fewer respiratory complications, 26% fewer gastrointestinal complications and a 19% decrease in opioid prescriptions compared with those receiving opioids only. Total knee arthroplasty analyses showed similar patterns.
The researchers said the results should encourage the use of multimodal perioperative analgesia for joint replacement surgery.
References
[1] Memtsoudis S, Poeran J, Zubizarreta N et al. Association of multimodal pain management strategies with perioperative outcomes and resource utilization. Anesthesiology 2018. doi: 10.1097/ALN.0000000000002132