Shutterstock.com
More than 70% of people would be happy to consult with a pharmacist or nurse in their GP surgery, or with a community pharmacist, regarding a respiratory tract infection (RTI), according to survey results published in BJGP Open.
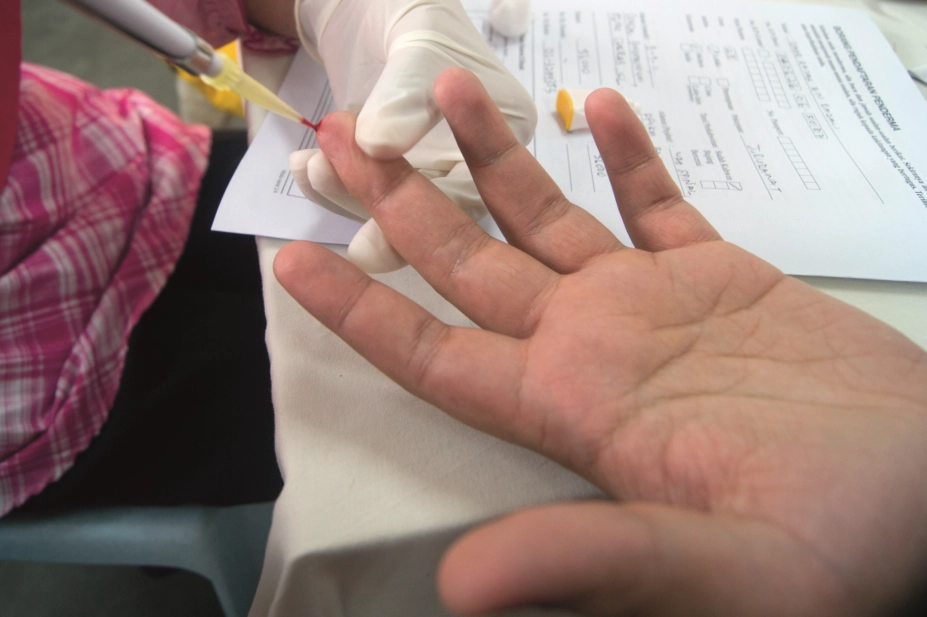
In addition, more than 90% of the almost 9,000 people surveyed would be happy to have a finger-prick blood test in primary care to help inform the need for antibiotics.
The aim of the study was to describe public perceptions regarding finger-prick testing, back-up antibiotic prescriptions (also known as delayed antibiotic prescriptions) and alternatives to traditional consultations for RTIs, with the purpose of directing further research and service design.
According to the researchers, RTIs are one of the most frequent reasons for consulting in primary care and contribute significantly to GP workload in the UK. In addition, UK national guidance recommends that GPs do not prescribe antibiotics for most RTIs, but prescribing continues to be “excessive”. Alternatives to face-to-face GP consultations, the researchers said, may help reduce the pressure on primary care services from RTIs, and use of antibiotics.
More than 8,750 people completed the questionnaire between 2016 and 2018 as part of HealthWise Wales, a national online cohort study in Wales. The questionnaire covered five domains: perceived consulting frequency, drivers of consulting, perceptions of serious illness, alternative sources of information and views about alternative approaches to consulting for RTIs.
Of the participants who completed the question about consulting for an RTI with a pharmacist or nurse in their usual GP surgery, 76.7% were in favour, and, of those who completed the question about consulting with a community pharmacist with training in assessing RTIs, 71.2% were in favour.
In addition, 92.8% were in favour of having a finger-prick blood test to help guide antibiotic treatment during a consultation; however, just 31.8% said they would be happy to have a back-up, or delayed, antibiotic prescription if their clinician thought they did not need immediate antibiotics.
Slightly more than 33% of respondents indicated that they would not feel comfortable in knowing when to take a back-up prescription.
The researchers said that their findings supported the view that several approaches to managing RTIs were likely to be acceptable to the public.
“Pharmacists, nurses and allied health professionals already play an important role in managing RTIs, and our findings suggest that many value these options,” they said.
They also said it was “encouraging” to see that more than 90% were happy to have a finger-prick blood test to guide antibiotic prescribing.
“POCT [point-of-care testing] can improve antibiotic prescribing for RTIs, including acute exacerbations of COPD,” they added.
A spokesperson for Community pharmacy Wales said: “It is always heartening to see the public showing an overwhelming trust in community pharmacists to deliver tests and undertake less traditional roles.”
“Whether or not this service is ever delivered in a community pharmacist setting is for the future, but certainly the move to community pharmacists delivering clinical services is part of an ongoing journey for the profession.”

