MattLphotography / Alamy Stock Photo
Open access article
Hospital pharmacy teams could be involved in the aseptic preparation of neutralising monoclonal antibodies (nMABs), which would be given to patients in their homes as part of new NHS treatment services for COVID-19.
The monoclonal antibody treatment could be available to patients at high risk of severe disease and mortality — including ‘clinically extremely vulnerable’ individuals, care home residents and people aged 70 years and over — and those with impaired immune function.
The suggestion follows comments made by Simon Stevens, chief executive of the NHS, on 15 June 2021, that NHS services should “gear up” for the provision of nMABs so that the treatment can “immediately begin to be deployed” when it becomes available.
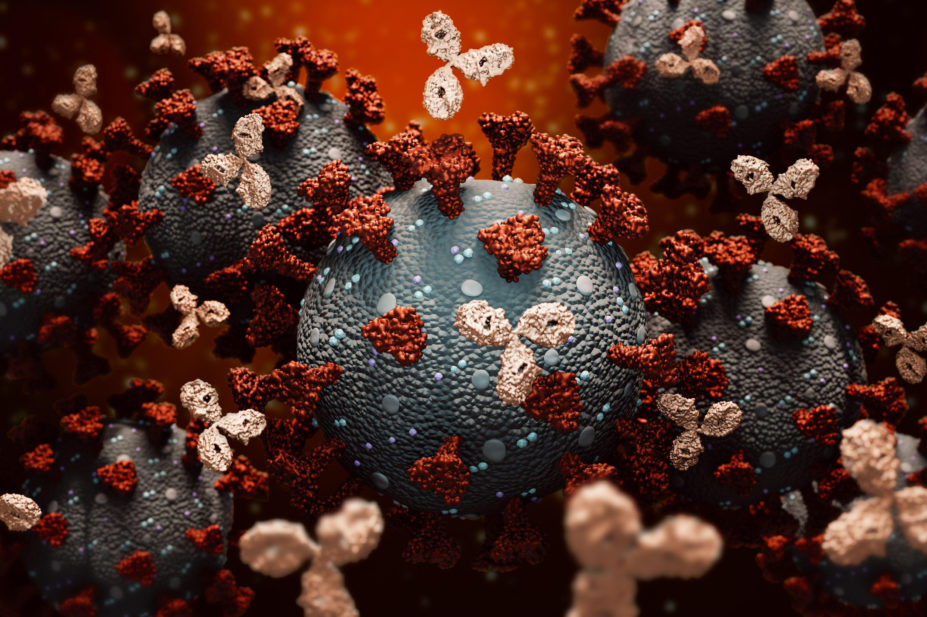
The antibodies bind to SARS-CoV-2 spike proteins, blocking the virus from entering host cells and preventing its replication.
Several such treatments are currently under development, including REGEN-COV, which was recently found to have reduced the risk of death and the length of hospital stay for seronegative patients hospitalised with severe COVID-19.
In a draft document, labelled as ‘confidential’ and seen by The Pharmaceutical Journal, NHS England sets out possible patient pathways for the administration of the treatment, as well as workforce requirements.
The document highlights that it is “not a policy” but is “designed to support the implementation of new interventions”.
As part of the implementation process, the document says hospital chief pharmacists would be involved in developing the standard operating procedure “for ordering, preparation and administration of the treatment”.
Chief pharmacists would also oversee treatment supply, cold chain storage and stock management for reporting “into the national reporting system”.
It adds that “sterile infusions should be prepared in line with local protocols by appropriately trained pharmacy or nursing staff using aseptic technique and good clinical practice”.
Raliat Onatade, group chief pharmacist at Barts Health NHS Trust, said she was “in the very early stages of thinking about this”.
“Pharmacy will need to lead on the aseptic preparation, as this is our role. We will need to collaborate at system-level,” she said.
According to the document, “the NHS is working with the [Department of Health and Social Care] to identify specific cohorts that are likely to be suitable for treatment with nMABs.”
The “likely candidates” proposed include clinically extremely vulnerable individuals, care home residents, individuals aged over 70 years, patients with nosocomial infections and “wider vulnerable groups”, such as those being considered for nMAB treatment by the European Medicines Agency and the United States Food and Drug Administration.
Under the NHS service, eligible patients will receive the treatment within three days of a positive COVID-19 polymerase chain reaction test, either “in dedicated treatment centres” or through a “hospital at home-type service that administers treatment at the patient’s base”.
The latter model would be “suitable for the most vulnerable patients who are unlikely to be able to present to outpatient treatment facilities”, the document says.
It adds that the “current preferred option” for patients to access the treatment service would involve high-risk patients being “proactively identified and notified of their eligibility to receive treatment with nMABs should they become infected”.
“Patients in this cohort will be advised to contact their GP or attend a local treatment centre in the event of a positive test for further assessment (subject to discussion) and referral for treatment as appropriate,” the document says.
Stevens told attendees at the NHS Confederation conference that nMABs “are potentially going to become available to us within the next several months”.
“But in order to be able to administer them, we’re going to need community services that are able to deliver, through regional networks, this type of infusion in patients before they are hospitalised, typically within a three-day window from the date of infection.
“So, the logistics and the organisation, and applying the full excellence the networked NHS services locally through integrated care systems — we’re going to need to harness all of that to be able to benefit from these new monoclonal antibodies,” he said.
READ MORE: Everything you need to know about the COVID-19 therapy trials


