Shutterstock.com
National action should be taken to make naloxone kits more widely available to people who use illegal drugs, a coroner has said in a ‘Prevention of future deaths’ (PFD) report.
Ian Potter, assistant coroner for Inner North London, made his recommendation in a PFD issued to the Department of Health and Social Care, published on 2 January 2025, following an investigation into the death of Joseph Benjamin Forbes Black, who died in August 2023 of acute polydrug toxicity.
The PFD said that Forbes Black “died as a result of acute polydrug toxicity, which included the taking of heroin that had been adulterated with protonitazene and metonitazene”.
“The presence of ‘nitazenes’ more than minimally contributed to his death,” it added.
Naloxone, an injectable opioid antidote that can reverse the effects of an opioid overdose, was not given in this case “because the circumstances in which he was found did not indicate that the administration of naloxone would be of any use in this instance”.
However, the coroner concluded that deaths could be prevented if naloxone kits were more readily available to drug users.
“The evidence revealed that neither the supported accommodation provider nor the mental health NHS trust that was treating Mr Forbes Black were permitted to give naloxone kits to their residents/patients who were known drug users,” Potter’s report said.
“In my experience, from this inquest and others, a significant proportion of illicit drug users are not engaged with or decline to engage with substance misuse services for a number of possible reasons. The evidence in the inquest was that if a drug user wanted to have naloxone in their possession as a safety-net measure, they would need to obtain this from a local substance misuse service.
“I am concerned that this set of circumstances raises the risk of future deaths occurring because the provision of naloxone kits could be made more widely available to those most likely to need them. The present situation appears to be that naloxone is most easily accessed through the very service(s) that many drug users are not engaged with. My concern, based on the evidence heard at this inquest and others that I am aware of, is that this is not a localised matter and is more likely a nationwide issue, and that action should be taken more widely.”
Potter added that the need for action was “heightened” because of the presence of nitazenes in street heroin.
On 2 December 2024, legislation came into force allowing pharmacists and pharmacy technicians — as well as others including prison staff, registered midwives and registered nurses — to supply take-home supplies of naloxone without a prescription, as part of drug treatment services.
Speaking in her capacity as chair of the Royal Pharmaceutical Society’s science and research committee, Amira Guirguis told The Pharmaceutical Journal: “[Nitazenes are] often detected as adulterants in heroin and other illicit drugs … [and] present a severe overdose risk due to their extreme potency, amplifying the urgency for wider naloxone availability.
“A positive step forward is the December 2024 amendment to the Human Medicines Regulations 2012, which will extend naloxone supply rights to the armed forces, police, prisons, probation officers, midwives, nurses, pharmacy professionals and paramedics,” she added.
“However, these changes are enabling rather than mandatory, leaving implementation to local discretion and funding priorities. This inconsistency risks delaying life-saving access where it is most needed.
“A coordinated national strategy is essential to ensure equitable naloxone access across all regions. This should include mandatory naloxone training for all professionals included in the expanded legislation, the provision of take-home naloxone kits in supported accommodation and community settings where overdose risks are highest and the introduction of anonymous mail-order services, similar to Scotland’s successful ‘click and deliver’ scheme.
“Additionally, pharmacies and community services should play a central role in proactive naloxone distribution to maximise accessibility.”
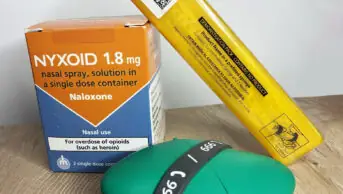
Graham Parsons, director of pharmacy at Waythrough, a charity supporting people with mental health, drugs, alcohol, housing and related areas, said: “Access to naloxone as a nasal spray or injection remains an important element of effective treatment provision to support the reduction in drug-related deaths, especially with the emergence of nitazenes in the UK. This includes through community pharmacies like the scheme Waythrough coordinates in Sheffield through our Likewise Sheffield service.
“We hope changes to the Human Medicines Regulations in December 2024 will support wider provision with appropriate commissioning arrangements in place. But in the meantime, we would encourage anybody who may witness or be at risk of an opioid overdose to obtain a naloxone kit from their local substance use provider.”
- This article was amended on 16 January 2025 to clarify the capacity through which Amira Guirguis was commenting