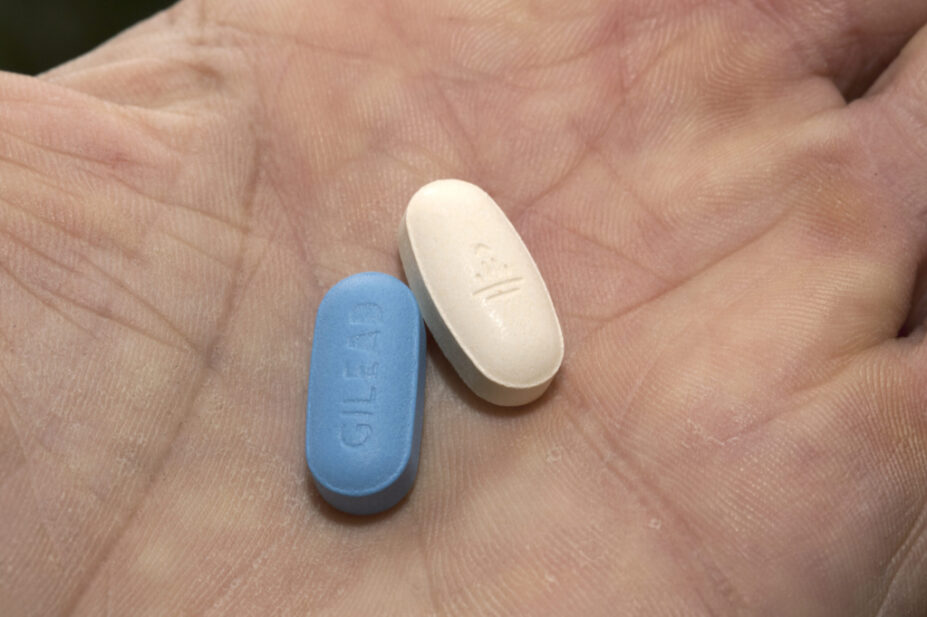
DR P. MARAZZI / SCIENCE PHOTO LIBRARY
Government advisers have recommended a series of national pilots for pre-exposure prophylaxis (PrEP) provision in settings outside specialist sexual health clinics, including pharmacies.
According to documents seen by The Pharmaceutical Journal, the ‘PrEP access and equity task and finish group’ — established by the Department of Health and Social Care (DHSC) in October 2022 to identify ways of improving access to PrEP as part of the the HIV action plan, which pledges to eliminate HIV transmission by 2030 — has made several recommendations to improve access to PrEP and reduce HIV transmission in England, which are currently being considered by government ministers.
Among these is a recommendation that “national health bodies, in partnership with local commissioners, should commission a series of pilots providing PrEP in a variety of settings outside specialist sexual health clinics, including online, pharmacies, GPs, a community setting, a contraceptive clinic and a non-specialist sexual health setting”.
The taskforce has also recommended that the pilots must be supported by funding for promotion and gathering learnings to expand PrEP provision nationally, and that co-production with populations who use or who could benefit from PrEP should be “prioritised”.
“The Department for Health and Social Care must commit to swiftly considering the findings of PrEP pilots and if successful, commission PrEP beyond sexual health services nationally,” the documents said.
In a parliamentary answer, published on 3 April 2023, health minister Lord Markham said the recommendations of the ‘PrEP access and equity task and finish group’ were being considered by the HIV Action Plan Implementation Steering Group and that the plan would be made available in 2023.
The Pharmaceutical Journal approached the DHSC but it said it would not comment on leaked information.
Commenting on the proposals, Jim McManus, president of the Association of Directors of Public Health, said that, since the HIV action plan, “there has been progress, but probably not as fast as people would like”.
McManus said directors of public health wanted PrEP access to be improved, but one of the challenges was “it takes money and the government hasn’t come up with money and the public health budget has been cut”.
He added that there was a need for a “vision” for how community pharmacy could best be used in public health.
An online pilot, run by a sexual health service provider, is currently in progress, but McManus said there was a need for pilots in other settings.
“There is a desire to do [a pilot] in prisons and in pharmacies as well,” he said.
“We would be encouraging of pilot schemes and there are a number ongoing. It’s now in the hands of the Department of Health and Social Care. The problem for them is, have you got the money for it? The ball is in the court of the Department of Health.”
Katie Clark, policy and public affairs officer at the Terrence Higgins Trust, a UK HIV and sexual health charity, said too many people were still struggling to get PrEP.
“The roll out of PrEP in the England has contributed to a steep decline in new HIV diagnoses among gay, bisexual and other men who have sex with men in London since 2014,” she said.
“But PrEP has the potential to do so much more, particularly for women. Our joint ‘Not PrEPared’ report revealed significant barriers to access and found that no local authority has more than five women accessing it. You can’t access something you don’t know about and that’s why we’re working to increase awareness of PrEP in all communities affected by HIV.
“We’re also calling for PrEP access to be extended to primary care settings to reach those who don’t usually attend sexual health clinics — as the government committed in the HIV Action Plan. For example, community pharmacies are in a good position to provide PrEP to people reluctant to access sexual health services and access online would take pressure off over-burdened sexual health services.”
In May 2022, The Pharmaceutical Journal learned that community pharmacies could be asked to target high risk or underserved groups with PrEP to prevent HIV infection, but only if specialist clinics were shown to not be capable of reaching everyone they should.
At the time, the English HIV and Sexual Health Commissioners’ Group, a network of local authority and clinical commissioning group commissioners across England, said that first there was “work to do” to fully understand the barriers to PrEP uptake in level 3 sexual health clinics before access is expanded to other settings.
PrEP has been routinely available in specialist sexual health services since 2020. Local authorities in England are responsible for commissioning comprehensive open access to most sexual and reproductive health services, including HIV prevention, testing and access to PrEP, through the public health grant, funded at £3.5bn in 2023/2024.


