Shutterstock
The National Institute for Health and Care Excellence (NICE), the UK’s cost-effectiveness body, has recommended two new cholesterol-lowering drugs for adults with primary hypercholesterolaemia or mixed dyslipidaemia who are at extremely high risk of heart attacks and strokes.
Alirocumab (Praluent, Sanofi) and evolucumab (Repatha, Amgen), known as PCSK9 inhibitors, are recommended for people whose cholesterol levels are not adequately controlled with other drugs, such as statins, when they can’t tolerate statins because of side effects, or because they have another condition which means they can’t take them.

Source: Kausik Ray
In terms of effectiveness, the drugs are “probably the biggest advance in cholesterol-lowering medications since statins”, says Kausik Ray, professor of public health and honorary consultant cardiologist at Imperial College London.
PCSK9 inhibitors are likely to make “a real difference” to patients with very high levels of cholesterol, particularly those with familial hypercholesterolaemia, a condition that affects about 1 in 250 people, Ray adds.
People with familial hypercholesterolaemia have raised cholesterol levels from birth, so their risk of cardiovascular disease increases to as much as 50% in males by the age of 50 years old and to at least 30% in women by the age of 60 years old.
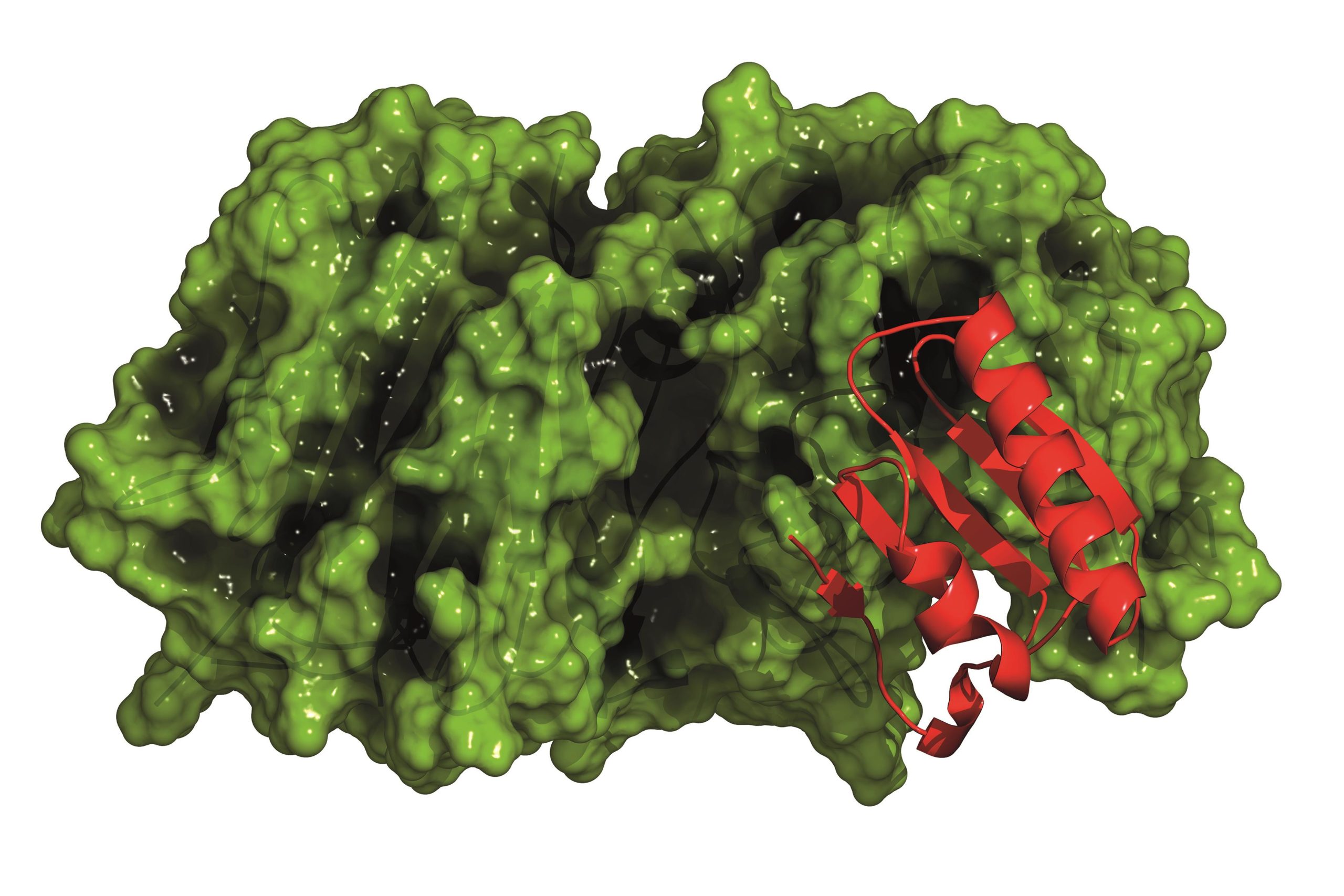
PCSK9 inhibitors work differently to statins, which slow down the liver’s production of cholesterol. PCSK9 is a protein that regulates the number of receptors for ‘bad’ cholesterol (low-density lipoprotein cholesterol [LDL-C]) on the liver’s surface. By reducing this protein, alirocumab and evolocumab increase the availability of receptors for ‘bad’ cholesterol and therefore lower the levels of ‘bad’ cholesterol in the blood.
Both drugs are given by self-administered injection once every two weeks, or once a month for the 420mg dose of evolocumab. As a result, Ray says that the potential for multiple adverse side effects that are associated with statins, which are small molecules and are orally ingested, is lower.
Carole Longson, director of the NICE’s centre for health technology evaluation, says that while its appraisal committee concludes that both drugs are effective in reducing levels of ‘bad cholesterol’ in people with hypercholesterolaemia or mixed dyslipidaemia when compared with placebo, ezetimibe or statins, both drugs are relatively expensive.
The annual cost of evolocumab per patient is about £4,448.60 for 140mg every two weeks. Alirocumab costs £4,383 for 75mg or 150mg every two weeks. This compares with an annual cost of around £350.00 for ezetemibe.
“The draft guidance recommends alirocumab and evolocumab as a cost effective use of NHS resources only with the discounts agreed with the [drug] companies,” Longson adds.
NICE will not disclose the level of the discount agreed, but says use of alirocumab and evolocumab is cost-effective with an LDL-C level above 3.5mmol/l where the patient has existing cardiovascular disease alongside heterozygous familial hypercholesterolaemia (HeFH) or a very high risk of further cardiovascular events without HeFH.
It also specifies an LDL-C level above 4.0mmol/l for treatment of patients with cardiovascular disease who have a high risk (without HeFH); and an LDL-C level above 5.0mmol/l for patients with HeFH who do not have cardiovascular disease.
Ray says that the narrow indication and the fact that the drugs are likely to be initiated in hospitals at specialist clinics means that they are unlikely to be overprescribed.


