david pearson / Alamy Stock Photo
The number of prescription items endorsed as ‘not dispensed’ by community pharmacists in England increased by nearly a fifth in one year, data obtained by The Pharmaceutical Journal has shown.
The figures, obtained by The Pharmaceutical Journal from NHS Business Services Authority (BSA) through a freedom of information request, revealed an 18.2% increase in the number of prescription items marked as ‘not dispensed’ on both paper and electronic prescriptions between 2021/2022 and 2022/2023.
The increase follows a two-year decline in the number of ‘not dispensed’ items between 2019/2020 and 2021/2022, when 5,861,258 items and 4,841,474 items were not dispensed, respectively.
The number of ‘not dispensed’ items then increased to 5,720,529 in 2022/2023.
This may owe to more patients no longer requiring prescriptions; being unable to pay the prescription charges and so choosing not to take it; or if the product is unavailable owing to medicines shortages.
However, it comes as comes as pharmacy and other bodies raise growing concerns about the impact of the prescription charge on patients’ access to medicines during the cost of living crisis.
In March 2023, a survey of 4,014 people with long-term conditions by the coalition found that 1 in 10 (9%) were not able to collect their prescriptions in the past 12 months because of the cost.
A survey of 269 community pharmacists by the Royal Pharmaceutical Society, conducted at the end of 2022, revealed that half (51%) of its respondents reported seeing an increase in the number of patients not collecting prescriptions in the past six months, owing to affordability issues.
Gareth Jones, director of external and corporate affairs at the National Pharmacy Association (NPA), said the exemption system was part of the problem. “Prescription charges can deter people from getting the medicines they are prescribed, especially people on low, fixed incomes,” he said.
Azeem Majeed, professor of primary care and public health at Imperial College London, agreed that, despite the high proportion of patients eligible for free prescriptions, “for those who have to pay, the NHS prescription charge can be a significant financial burden”.
“This could exacerbate societal and health inequalities if those on poorer incomes (but not eligible for free prescriptions) have to pay for the drugs they need,” he said.
The data from the NHSBSA also reveal that the increase in items endorsed as ‘not dispensed’ has disproportionately impacted patients living in areas with the second-highest proportion of people on income support, whose incomes are lower, but not low enough to qualify for income support programmes that would make them eligible for free prescriptions.
Using the government’s index of income deprivation, which ranks areas based on the proportion of people living there who receive benefits and tax credits, an analysis by The Pharmaceutical Journal shows that pharmacies in areas that have the second-highest proportion of people on income support saw the largest increase in the number of ‘not dispensed’ endorsements in the past year.
In these areas, the number of ‘not dispensed’ endorsements increased by 26%, from 718,081 items in 2021/2022 to 904,733 items in 2022/2023.
Pharmacies in areas with the highest proportion of people receiving this type of support — who would qualify for free prescriptions — saw a 15% increase in the number of items marked ‘not dispensed’, from 686,218 item in 2021/2022 to 789,641 in 2022/2023.
This comes after the government invested £200m in integrated care boards to help meet specific targets relating to NHS England’s Core20PLUS5 initiative, which is aimed to reduce health inequalities in the 20% most deprived areas.
A spokesperson for the Department of Health and Social Care said: “Almost nine out of every ten prescriptions are dispensed free of charge in England. Patients with long-term conditions or on a low income can apply for a range of prescription charge exemptions or additional support through the NHS Low Income Scheme.
“There are a number of reasons why prescriptions may not be dispensed, so it is important not to ascribe all to one cause.”

Health inequalities
The Royal Pharmaceutical Society’s policy on health inequalities was drawn up in January 2023 following a presentation by Michael Marmot, director of the Institute for Health Equity, at the RPS annual conference in November 2022. The presentation highlighted the stark health inequalities across Britain.
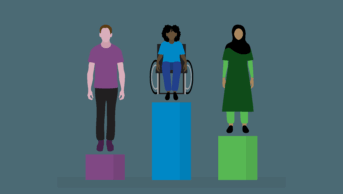
While community pharmacies are most frequently located in areas of high deprivation, people living in these areas do not access the full range of services that are available. To mitigate this, the policy calls on pharmacies to not only think about the services it provides but also how it provides them by considering three actions:
- Deepening understanding of health inequalities
- This means developing an insight into the demographics of the population served by pharmacies using population health statistics and by engaging with patients directly through local community or faith groups.
- Understanding and improving pharmacy culture
- This calls on the whole pharmacy team to create a welcoming culture for all patients, empowering them to take an active role in their own care, and improving communication skills within the team and with patients.
- Improving structural barriers
- This calls for improving accessibility of patient information resources and incorporating health inequalities into pharmacy training and education to tackle wider barriers to care.