Shutterstock.com
More research is needed to assess the harmful effects on oncology healthcare staff of administering cytotoxic drugs and whether enough is being done to protect them, a research report by consumer and business analyst MindMetre Research says.
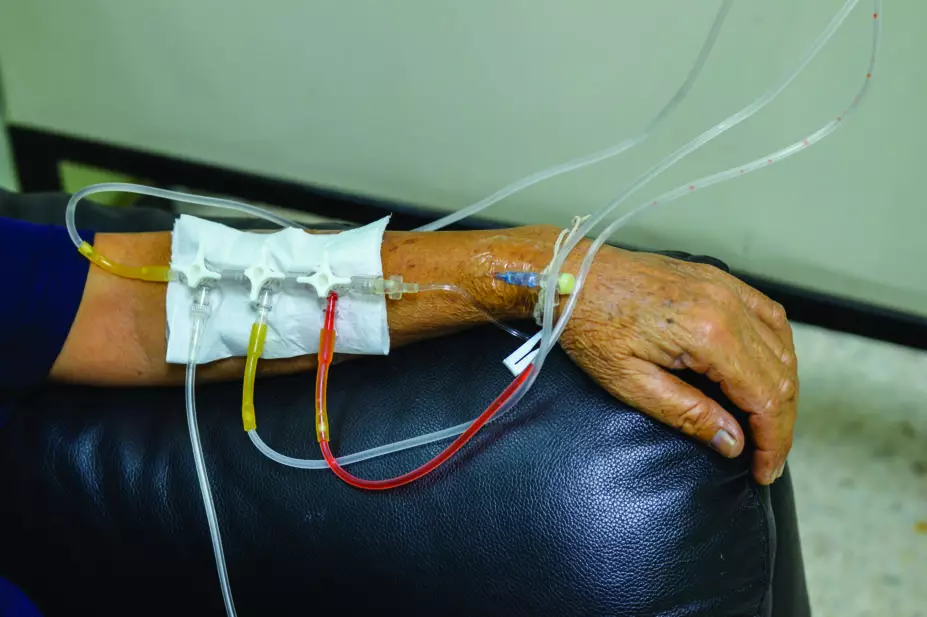
While the risks to pharmacy staff who prepare hazardous drugs are well documented and regulated, the risk of potentially harmful exposure to those administering such drugs seem to have been overlooked, says the report.
It points to results from a number of United States and European studies which indicate that oncology nurses administering chemotherapy are experiencing symptoms, such as hair loss and an unusually high rate of miscarriage, which is likely to be the result of exposure to these cyototoxic drugs.
The MindMetre researchers say that the potential damage to staff of administering hazardous cancer drugs should at least be further scrutinised.
The report also looks at whether measurement and monitoring of cytotoxic drug contamination levels is sufficiently rigorous. The use of ‘closed systems’ to prevent any escape of hazardous drug or vapour, from the point of preparation to administration and disposal, is mandated by regulations in the United States and many European nations. But, according to the report, many current transfer and administration protocols may not be compliant and contamination is not being regularly monitored at ward level. There is no Europe-wide legislation, guidelines or minimum standards to precisely define administration processes.

Source: Courtesy MindMetre Research
Paul Lindsell, managing director at MindMetre Research, says that regulation and prevention of the occupational risks are not rigorous enough
Paul Lindsell, managing director of MindMetre Research, says: “The evidence strongly suggests that nurses who are regularly administering chemotherapy drugs are at risk of developing health problems as a result of their prolonged exposure to cytotoxic chemicals. It appears that regulation and, more importantly, prevention of the occupational risks that these healthcare workers face is not rigorous enough, which raises serious questions of morality.”
He adds: “It has become increasingly apparent that policy makers and experts need to consider closed systems as a vital alternative to current methods of administration, and crucially, there needs to be stricter and more rigorously enforced guidelines in place to ensure the welfare of nurses and patients alike.”


