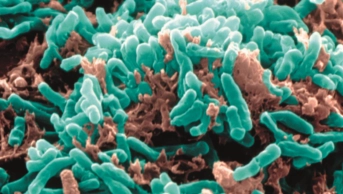
Shutterstock.com
Pharmacy involvement is “absent” from 43% of tuberculosis (TB) services in England, according to a report from the Getting It Right First Time projects team at the Royal National Orthopaedic Hospital (RNOH/GIRFT).
The ‘RNOH/GIRFT review of tuberculosis report‘, published on 14 March 2025 and commissioned by NHS England, cited UK Health Security Agency data that show there was an 11% rise in TB notifications in England in 2023, when 4,855 people were notified with TB compared with 4,380 people in 2022.
The report said this increase was keeping England “off target for WHO [World Health Organization] eradication” of the disease by 2035.
The increase in cases has been concentrated in large urban areas in the most deprived postcodes, with the rate of notification “especially high” among homeless people and prisoners, at over 28 per 100,000, in contrast to the all-England rate at 7.8 per 100,000.
As a result, the report said England remains off target for WHO eradication of TB, which would require reducing the number of notifications to 1.05 per 100,000 population.
The report noted that while “pharmacy time was essential” for TB services, “it was disappointing that the role of pharmacy in TB services was poorly recognised, being absent in 43% of services”.
“This needs to be addressed as part of any service expansion… We recommend an incremental amount of pharmacy time based upon contacts and notifications [for TB services].”
The report added that it should be the responsibility of providers and integrated care boards (ICBs) that a senior pharmacist of band 7 or higher should be attached to and support each TB service on a pro rata basis.
It also recommended that the role of pharmacy support for regional multidisciplinary teams should be included in the future development and funding of such services.
It also says providers should ensure that a senior pharmacist provides support and education for ward-based pharmacists when TB expertise is not available, and says pharmacists should work with dispensing teams and the TB service to ensure that information given to patients is “appropriate in both language and content, recognising that some individuals on active or preventative treatment may not be able to read”.
Anti-TB drug shortages also emerged as “a significant problem” in the report, with 97% of services experiencing drug shortages, creating “a significant impact on patient care and on clinical teams’ workload, as exemplified by a higher tablet burden for patients, potentially affecting drug adherence and increasing the risk of drug errors”.
“There should be a national infrastructure to minimise future drug shortages [and] ensure there is a clear cascade of information centrally from NHS England via pharmacists if there are potential shortages,” the authors wrote.
“Plans should be in place across regions and nationally for shared support and to minimise stockpiling.”
Responding to the recommendations, Nathan Burley, advanced public health/sexual health services pharmacist at NHS Greater Glasgow and Clyde, said: “TB treatment involves the use of multiple antimicrobial agents. These agents themselves can cause considerable side effects and interact with many other medicines, whilst adherence to the regimen for extended durations is of paramount importance to ensure treatment success and minimise the risk of resistance.
“It is essential to have pharmacist input right from the outset of treatment in all healthcare systems, ideally as part of both secondary and primary care teams treating patients. There have also been recent stock issues affecting TB drugs and again highlights why pharmacists are crucial — for treatment success and the many antimicrobial stewardship reasons above.”
A spokesperson for NHS England said: “Many recommendations can be implemented through ICBs and providers modifying services, with support from local authorities to embed changes. NHS England will be working with partners — where relevant — to support implementation of these recommendations, for the benefit of patients.”
The RNOH/GIRFT team has now been asked by NHS England to develop and deliver a framework to support this implementation, which began in January 2025 and will take 12 months.