Jon Barlow
Engaging with local community or faith groups can help pharmacy teams understand their local populations better, a strategy paper published by the Royal Pharmaceutical Society (RPS) says.
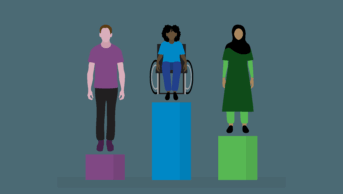
‘Tackling health inequalities: delivering accessible pharmaceutical care for everyone‘, published on 11 January 2023, sets out how pharmacy teams can help deliver accessible pharmaceutical care for everyone in their community.
As part of this, the paper says that pharmacists could study local demographic statistics and compare these to the people who use the pharmacy to see if any groups are missing. Pharmacy teams can then consider how they can reach people who are not currently accessing their services.
“Understanding a local population involves engaging with people directly,” the paper says. “This might be through approaching local community or faith groups, seeking views from patients or gaining insight from pharmacy staff members.
“The richness of understanding you gain from hearing from someone living in poverty every day is significantly greater than reading about socio-economic data; similarly, speaking with someone of a different faith can transform your understanding of cultural differences.”
The paper goes on to suggest how organisations can come together to “work to close these gaps”.
“Pharmacy teams should also consider working with others, such as community and third sector organisations, to identify the underserved and ‘missing’ populations.”
The RPS says staff involved in such outreach can be any member of the pharmacy team, not just pharmacists.
“These staff … could become health inequality champions, focused on understanding and meeting their local population’s needs,” the paper continues.
Other suggestions include providing a choice of languages and enabling access to interpreters; guarding against digital exclusion by ensuring that information provided through technology, such as apps and QR codes; and the implementation of digital prescription ordering systems and remote consulting.
The paper also suggests considering how easy the pharmacy is to find, as well as identifying any barriers to physical accessibility, both inside and outside the premises, and links to tools to help teams understand unconscious bias.
Claire Anderson, president of the RPS, commented: “As pharmacists, we need to think differently, proactively seek out people who may not be accessing our services, ensure we are welcoming and ultimately ensure that everyone can benefit from our support and care.”
Andrew Carruthers, chair of the RPS Scottish Pharmacy Board, added that the paper “aims to stimulate pharmacists’ thinking about how they provide care”.
“It brings together resources that they can then dip into over time to make improvements with the ultimate aim of delivering accessible pharmaceutical care to everyone,” he added.
Suhayla Dhanji Merali, highly specialist perinatal pharmacist at Central and North West London NHS Foundation Trust, and one of The Pharmaceutical Journal‘s Women to Watch 2022, commented: “From my experience within perinatal mental health, outreach work is a key tool, which enables communities with large ethnic minority populations to build awareness around mental health support. Awareness is the first step to enabling increased access to the services we provide within the NHS.
“We often need to step outside of our comfort zone and take the first step towards the populations we want to reach, so that we build relationships which inevitably allow us to support these individuals whose opinions on healthcare may be shaped by the community around them,” she added.

Health inequalities
The Royal Pharmaceutical Society’s policy on health inequalities was drawn up in January 2023 following a presentation by Michael Marmot, director of the Institute for Health Equity, at the RPS annual conference in November 2022. The presentation highlighted the stark health inequalities across Britain.
While community pharmacies are most frequently located in areas of high deprivation, people living in these areas do not access the full range of services that are available. To mitigate this, the policy calls on pharmacies to not only think about the services it provides but also how it provides them by considering three actions:
- Deepening understanding of health inequalities
- This means developing an insight into the demographics of the population served by pharmacies using population health statistics and by engaging with patients directly through local community or faith groups.
- Understanding and improving pharmacy culture
- This calls on the whole pharmacy team to create a welcoming culture for all patients, empowering them to take an active role in their own care, and improving communication skills within the team and with patients.
- Improving structural barriers
- This calls for improving accessibility of patient information resources and incorporating health inequalities into pharmacy training and education to tackle wider barriers to care.