Shutterstock.com
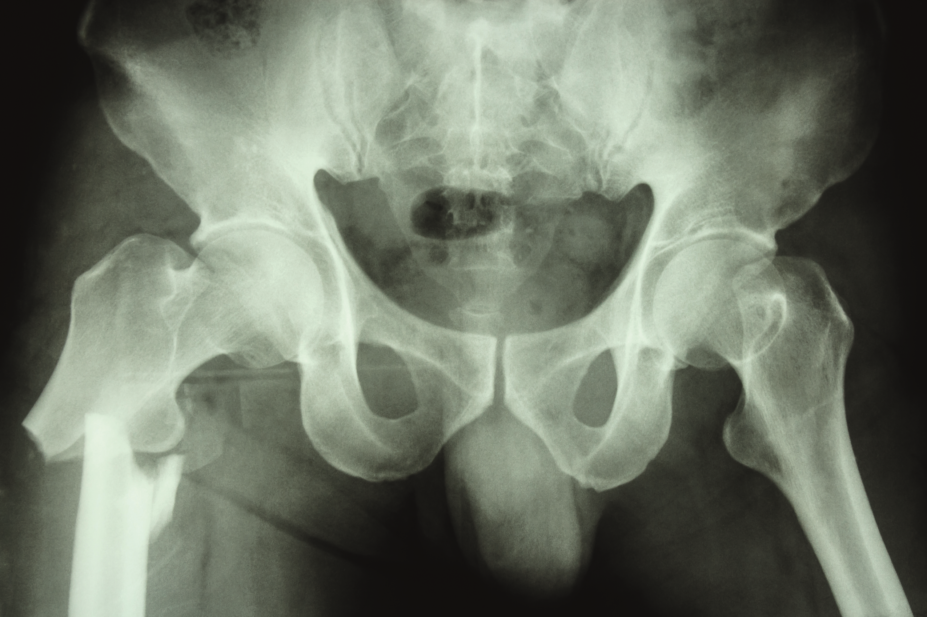
Antidepressants increase the risk of hip fracture in older people living in the community, including those with Alzheimer’s disease (AD), according to research published in the International Journal of Geriatric Psychiatry
[1]
(online, 5 January 2017).
This increased risk was associated with use of the three most frequently used antidepressant groups: selective serotonin reuptake inhibitors (SSRIs), mirtazapine, and selective noradrenaline reuptake inhibitors (SNRIs). Researchers also discovered that the association persisted even after adjusting for use of other medication that increases the risk of falls, osteoporosis, socioeconomic status and history of psychiatric diseases, as well as chronic diseases that increase the risk of falls or fractures.
“If the antidepressant treatment is necessary, other risk factors for falling should be carefully considered,” the authors say.
The researchers, based at the University of Eastern Finland in Kuopio, compared data on 50,491 people diagnosed with AD in Finland between 2005 and 2011 with data for 100,982 individuals without the condition.
For each person with AD there were two controls matched by age and sex. Participants were followed up for four years from the date of AD diagnosis (corresponding date for controls), and their mean age was 80 years.
Antidepressant use was associated with an increased risk of hip fracture among persons with and without AD (adjusted hazard ratio 1.61, 95% confidence interval [CI] 1.45–1.80 and 2.71, 95% CI 2.35–3.14, respectively) compared with non-use. During antidepressant use, the age-adjusted rate of hip fractures was 3.01 per 100 person-years (95% CI 2.75–3.34) among persons with AD and 2.28 (1.94–2.61) among persons without AD.
The risk of fracture was most prominent at the beginning of antidepressant use, but remained elevated with continued use up to four years.
Commenting on the study, Adam Darowski, a consultant geriatrician at the John Radcliffe Hospital in Oxford, who has an interest in falls, says the results show that the effect of antidepressants on the risk of hip fracture in people with AD is similar to, and not significantly worse, than that in the general older population.
Antidepressants have the potential to be “enormously harmful” in older people, he says.
“Doctors shouldn’t be giving antidepressants where there is some alternative,” he adds, pointing out that a lot of people are taking antidepressants because they needed them ten years ago.
“Anyone who is on antidepressants should have their antidepressant prescription reviewed regularly as to whether they need that drug and as to whether they need that dose of the drug. Could their antidepressant burden be reduced?”
Antidepressants are used not only for the treatment of depression, but also for the treatment of chronic pain and behavioural and psychological symptoms of dementia, including insomnia, anxiety and agitation. Darowski recommends against using antidepressants for sleep and says that, while they are effective for neuropathic pain, there are other options that can be explored.
Antidepressants cause falls in older people through several mechanisms, including sedation and orthostatic hypotension.
“The newer drugs (SSRIs and SNRIs) are generally not sedating,” Darowski explains. “As a group, they cause orthostatic hypotension, but these drugs differ substantially from each other in their pharmacology, and there is little data as to whether some are better than others. No data on falls or fractures are available on the newer melatonergic antidepressant agomelatine, which would not be expected to affect either balance or blood pressure.”
References
[1] Torvinen-Kiiskinen S, Tolppanen A-M, Koponen M et al. Antidepressant use and risk of hip fractures among community-dwelling persons with and without Alzheimer’s disease. International Journal of Geriatric Psychiatry 2017 doi: 10.1002/gps.4667


