Shutterstock.com
A hospital reduced the need for red blood cell transfusions by 40% for patients undergoing a full knee or hip replacement when they routinely gave them tranexamic acid, according to research published in the Canadian Journal of Anesthesia
[1]
on 4 September 2015.
The treatment also has the potential to save thousands of dollars since the cost of the drug is C$10 compared with C$1,200 for a blood transfusion, the researchers point out. These results add to a growing body of evidence that tranexamic acid is a safe and effective way to reduce the need for blood transfusions during surgery.
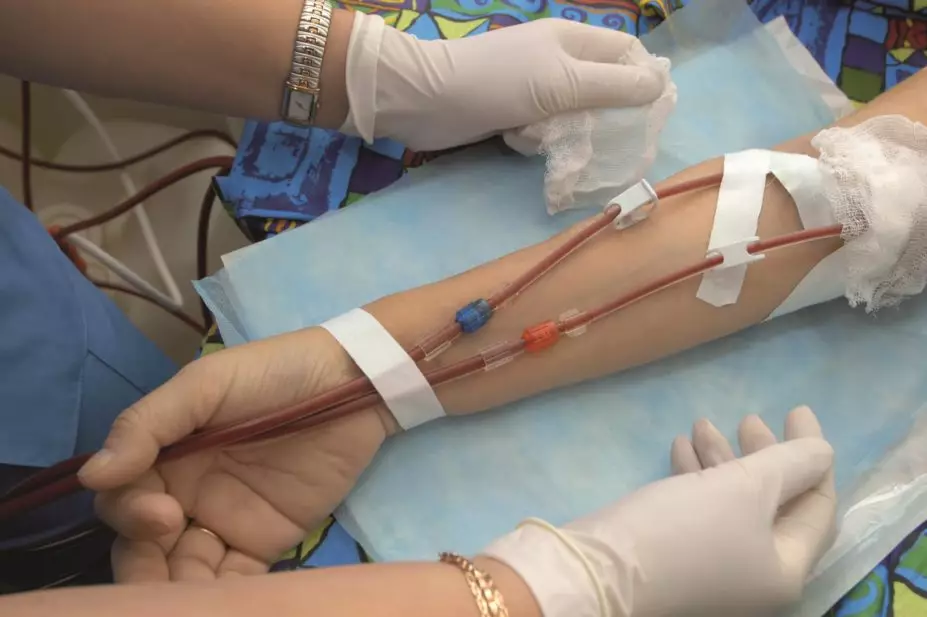
Researchers at the department of anaesthesia, St. Michael’s Hospital, University of Toronto, introduced a new protocol stipulating that all eligible patients undergoing a knee or hip replacement should be given a 20mg/kg intravenous dose of tranexamic acid. Use of tranexamic acid increased from 45.8% in the pre-protocol group to 95.3% in the post-protocol group.
The need for blood transfusion fell from 8.8% to 5.2% (P=0.043). Patients with a recent history of stroke, heart attack, blood clots or seizure disorder, renal insufficiency, or placement of a bare metal coronary stent were excluded from the trial, which ran between 21 October 2013 and 30 April 2014.
In an accompanying comment piece[2]
, Fiona Ralley, director of perioperative patient blood management at Western University, Canada, says there is now more than enough evidence to conclude that tranexamic acid should be routinely used in patients undergoing joint replacement.
“Until recently, concerns over tranexamic acid’s theoretical potential to increase postoperative venous thrombotic events (VTE) have unfortunately delayed or even prevented its broader use among arthroplasty patients,” she adds.
She says that several large studies have found no increased risk of blood clot after surgery for patients given the drug. But studies have routinely shown that its use reduces the need for blood transfusion by around 50%.
“Certainly, there is an overabundance of evidence that tranexamic acid reduces blood loss,” she says. “The introduction of protocols as implemented by Baker et al. will go a long way to ensure that this currently underused drug will be given to the right patient, in the right dose, and at the right time.”
In the current study, the length of hospital stay was the same for both patient groups and there was no statistically significant increase in the number of adverse events. However, there was an increase in the number of patients with acute kidney injury after the tranexamic acid protocol was implemented, going from 9 cases to 16. Although this was resolved within two days for all patients.
“Other hospitals and surgical centres should consider making tranexamic acid mandatory for similar surgeries because it can improve quality of care, decrease the need for blood transfusions and even save money,” says anaesthesiologist and lead researcher Greg Hare from St Michael’s Hospital.
“Making tranexamic acid mandatory for eligible patients has made care more efficient, ensuring the best possible care for our patients,” he adds.
References
[1] Baker J, Pavenski K, Razak P et al. Universal tranexamic acid therapy to minimize transfusion for major joint arthroplasty: a retrospective analysis of protocol implementation. Canadian Journal of Anesthesia 2015. doi:10.1007/s12630-015-0460-6.
[2] Ralley F. Tranexamic acid: When is enough (data) enough? Canadian Journal of Anesthesia 2015. doi:10.1007/s12630-015-0461-5.


