Shutterstock.com
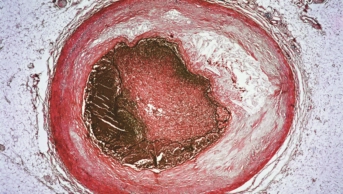
An injectable treatment has been launched for people who struggle to control their cholesterol levels through established diet and drug regimes, including patients with the genetic lipid disorder familial hypercholesterolaemia.
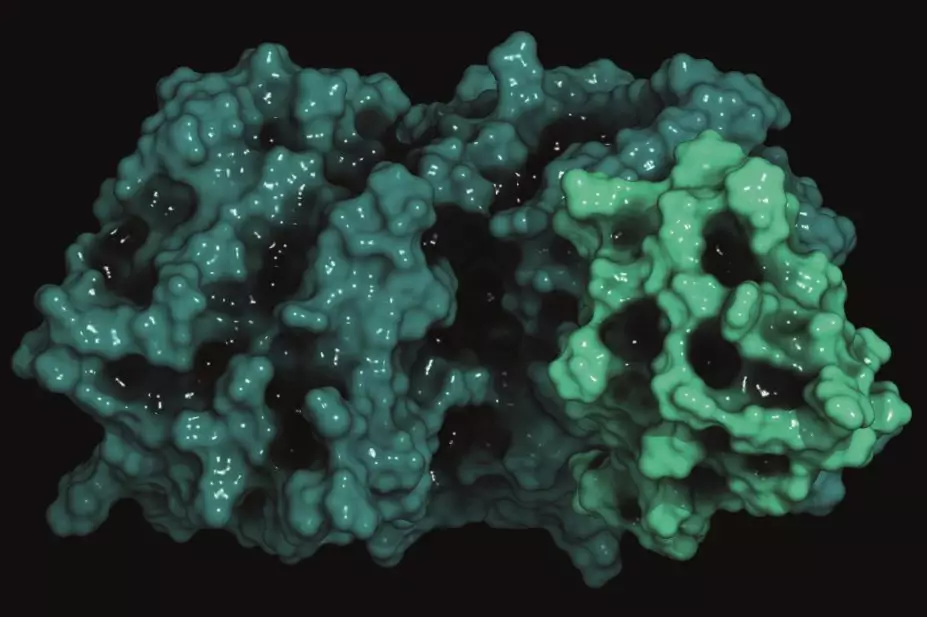
Amgen’s Repatha (evolocumab) is a monoclonal antibody and the first treatment to inhibit proprotein convertase subtilisin/kexin type 9 (PCSK9), an enzyme that reduces the liver’s ability to clear LDL cholesterol (‘bad’ cholesterol) from the blood. In clinical trials, evolocumab reduced LDL levels to 75% lower than atorvastatin alone.
Evolocumab was approved in Europe in May 2015 and in the United States in August 2015 for patients with primary hypercholesterolaemia who are unable to control their cholesterol with current therapies, or with familial hypercholesterolaemia. It is a fortnightly injection and can be used in tandem with statins, or without for patients who are intolerant of statins.
A National Institute for Health and Care Excellence (NICE) review is under way for treatment of primary hypercholesterolaemia and mixed dyslipidaemia, with recommendations expected in April 2016.
“It is possible to achieve satisfactory control of cholesterol in the vast majority of patients with modern, high intensity statin treatment,” says Dermot Neely, a trustee of HEART UK, and current co-chair of the familial hypercholesterolaemia guideline implementation team. “However, some patients are unable to tolerate a sufficient statin dose to reduce cholesterol enough to prevent progression of coronary disease.”
Neely says this new class of anti-PCSK9 drugs represents an important new option. “This new injectable treatment could help several thousand patients with heart disease and true statin intolerance. The cost, inevitably will be the limiting factor and we must therefore wait until NICE have completed their cost-effectiveness review which will define its role in routine NHS clinical practice,” he adds.
An ongoing trial, known as the FOURIER study, is looking at Repatha’s effects on rates of cardiovascular disease and death. This includes 27,564 patients worldwide, with 1,490 in the UK across 79 trial centres.