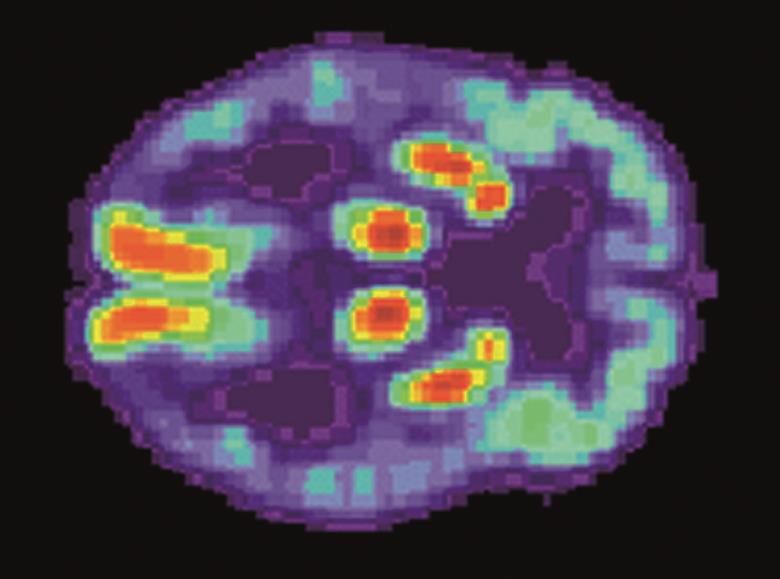
US National Institute on Aging, Alzheimer's Disease Education and Referral Center
The anti-inflammatory drug mefenamic acid can reverse memory loss and brain inflammation in a mouse model of Alzheimer’s disease, a study shows.
“Our research shows for the first time that mefenamic acid, a simple non-steroidal anti-inflammatory drug [NSAID], can target an important inflammatory pathway called the NLRP3 inflammasome, which damages brain cells,” says lead author David Brough, a senior lecturer at the faculty of biology, medicine and health at the University of Manchester.
“Until now, no drug has been available to target this pathway, so we are very excited by this result.”
The team, who report their findings in Nature Communications
[1]
(online, 11 August 2016), studied the effect of the fenamate class of NSAIDs on the NLRP3 inflammasome. This multi-protein complex, which is involved in the activation of the proinflammatory cytokine interleukin(IL)-1B, has been implicated in multiple aspects of Alzheimer’s disease, as well as a number of other inflammatory diseases such as atherosclerosis and type 2 diabetes.
They first showed in in vitro studies that fenamate NSAIDs (flufenamic acid, meclofenamic acid and mefenamic acid) are able to inhibit the NLRP3 inflammasome. Other NSAIDs, such as ibuprofen and diclofenac, did not.
The researchers then tested the effects of mefenamic acid (which they selected due to its routine use in clinical practice) in a mouse model of Alzheimer’s disease. By administering mefenamic acid over 28 days to these mice, they found that memory deficits, measured via novel object recognition, were completely reversed. And, the markers of inflammation, in the form of microglial activation and IL-1B expression, that would be expected in this disease model were reduced to levels comparable with wild-type mice.
The researchers say that much more research is needed to confirm whether the effects are similar in humans. But they say there are distinct advantages to exploring the use of existing drugs for Alzheimer’s disease.
“Because this drug is already available and the toxicity and pharmacokinetics of the drug is known, the time for it to reach patients should, in theory, be shorter than if we were developing completely new drugs,” says Brough.
Currently only one compound, known as MCC950, has been shown as a potent NLRP3-selective inhibitor, but it is not yet clinically available.
Another strategy being explored for the treatment of Alzheimer’s is the use of biologicals to target IL-1B. But the researchers say that as these types of therapy are expensive and do not readily penetrate the brain, fenamates could have real potential as either monotherapy or an adjunct to other treatments.
“We are now preparing applications to perform early phase II trials to determine a proof-of-concept that the molecules have an effect on neuroinflammation in humans,” Brough adds.
Diego Gomez-Nicola, a lecturer in biological sciences at the University of Southampton, says that the research is an important contribution to the field. There is a growing body of evidence that inflammation accelerates the progress of Alzheimer’s disease and several groups, including his, are working towards strategies that target this inflammation in a clinical setting.
“It would be interesting to see these experiments validated in other animals models of Alzheimer’s disease-like pathology, as well as understanding the mechanism by which targeting the inflammasome prevents neuropathology,” he says.
Doug Brown, director of research and development at Alzheimer’s Society, which helped fund the research, said the results are promising.
“Testing drugs already in use for other conditions is a priority for Alzheimer’s Society – it could allow us to shortcut the fifteen years or so needed to develop a new dementia drug from scratch,” said Brown. However, he added that there is not yet enough evidence to use NSAIDs against Alzheimer’s disease and cautioned that the risk of side effects must be taken into account.
References
[1] Daniels MJD, Rivers-Auty J, Schilling T et al. Fenamate NSAIDs inhibit the NLRP3 inflammasome and protect against Alzheimer’s disease in rodent models. Nature Communications 2016;7:12504. doi: 10.1038/ncomms12504


