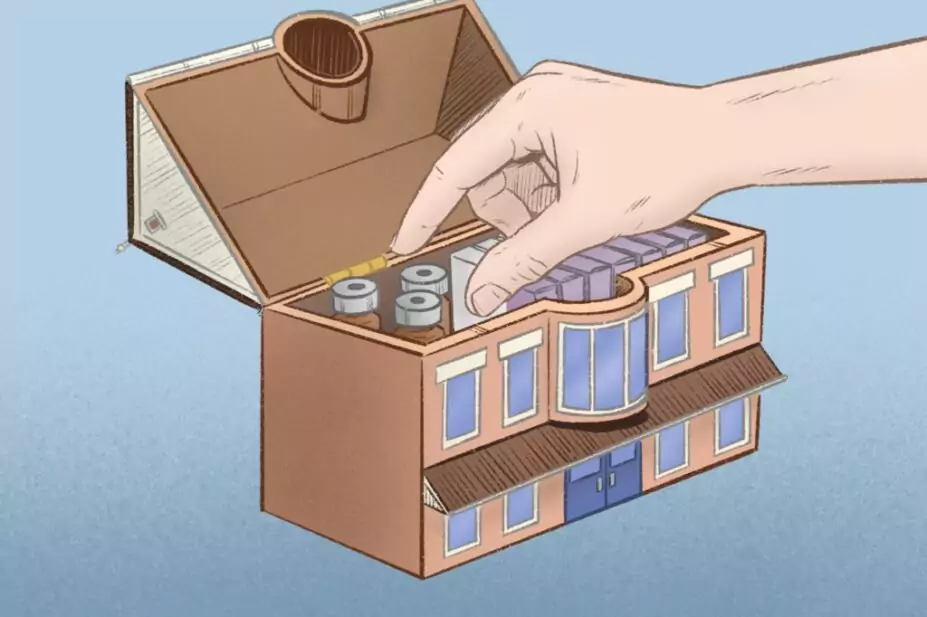
Wes Mountain/The Pharmaceutical Journal
Care homes play a critical role in providing comfort and specialised care to older people, particularly those requiring palliative care.
It is essential for every care home to have a strategy in place that supports a personalised approach to end-of-life care, drawing guidance from the National Institute for Health and Care Excellence (NICE)[1–3]. This guidance includes recommendations on the appropriate handling, storage and disposal of medicines, including controlled drugs (CDs), within care home settings.
CDs, such as morphine or midazolam, are often required by patients with advanced illnesses for symptom control, including to alleviate pain[4]. These medicines play a crucial role in enhancing patients’ comfort and dignity in their final stages of life.
When using these medicines in palliative care settings, including care homes, it is crucial that their administration is timely because patients often require immediate access to CDs to manage their symptoms effectively. Any delays can severely impact patients’ quality of life and cause distress for both patients and their families during an already emotionally challenging time.
However, care homes encounter a significant challenge in delivering high-quality palliative care owing to the strict regulations surrounding the management of CDs.
Residential homes, formally referred to as “care homes without nursing” by the Care Quality Commission (CQC), are not legally permitted to hold stocks of CDs and are instead restricted to holding CDs that are specifically prescribed and dispensed for individual residents.
Meanwhile, nursing homes, formally referred to by the CQC as “care homes with nursing”, are permitted to hold stocks of CDs but are severely restricted in which ones they can store.
Controlled drug licensing
The storage of certain CDs as stock items in nursing homes requires the possession of a UK Home Office CD licence. Nursing homes — of which there are 4,262 in England according to the CQC’s latest data — can hold stocks of CDs in schedules 3, 4, and 5 without the need for a Home Office licence.
A licence is mandatory for schedule 2 CDs in nursing homes where less than 50% of funding for the nursing home comes from public funds or charitable donations[5,6]. Schedule 2 CDs, including diamorphine and morphine, play a critical role in effectively managing the symptoms that regularly occur at the end-of-life.
Obtaining a Home Office CD licence is an expensive and time-consuming process, presenting significant challenges for nursing homes. The current cost of a license for the supply of CDs stands at £3,655, with additional annual renewal costs of up to £1,371. Unfortunately, this expense renders obtaining the licence unrealistic for most nursing homes, particularly for smaller care homes with limited resources[7]. Consequently, this could hinder their ability to provide adequate palliative care to their residents.
A well-functioning system for anticipatory medication hinges on seamless collaboration between healthcare providers, pharmacists, and care home staff
These regulations are pivotal for safeguarding public health, preventing misuse and reinforcing governance; however, it is equally vital to ensure that they do not hinder timely access to CDs for meeting patients’ needs, particularly in palliative care settings. Streamlining the licensing process and providing support to nursing homes when accessing CDs would help strike a crucial balance between ensuring patient safety and ensuring prompt access to palliative care.
During the COVID-19 outbreak, there was a temporary standard operating procedure that allowed for a safe and effective medicines reuse scheme in care homes, which was widely welcomed[8]. This procedure allowed for a quicker provision of CDs by permitting a medication prescribed for one resident to be reused for another. While this procedure did not technically alter the licensing regulations described, it created a unique situation where CDs were not kept as stock but could be repurposed for another person in need. This raised a grey area, justifying that a CD licence may not be required during a pandemic situation; however, this was a temporary measure and was since withdrawn in England in April 2022, highlighting the need for further consideration and potential adjustments to the existing regulations.
Bowers et al. argued that all nursing homes should be able to hold a stock of end-of-life drugs that can be rapidly accessed and administered following a prescription and also called for the permanent implementation of these COVID-related changes[9]. However, this would require a more cost-effective approach for care homes to obtain CD licences and for updates to the Human Medicines Regulations 2012 to be implemented, following collaboration between healthcare professionals, legal experts and regulatory authorities.
Access to stock
Without access to a stock of CDs, prescribing anticipatory medication requires each prescription to be dispensed individually, which can be time consuming and impractical. Given that approximately 80% of nursing home residents are in their final year of life, a considerable number may need anticipatory medication at any one time[9]. Prescribing and storing CDs for each resident with a potential need is not feasible owing to limited storage space in care home CD cabinets.
This situation not only poses storage issues but also increases the potential for errors and creates an overburden of stock checks. Moreover, such excessive prescribing is wasteful and goes against the NHS’s carbon goal, which aims to minimise environmental impact by avoiding unnecessary prescribing[10,11].
Providing care homes with access to a small stock of CDs would alleviate these challenges, making it more feasible for prescribers to offer anticipatory medication. This approach would enhance timely and effective symptom control for residents, particularly during out-of-hours situations, ultimately improving the quality of palliative care provided.
Certain considerations — such as the size and specialisation of the nursing home, especially if it focuses on palliative care — should influence the decision to maintain a stock of medication. In the case of small nursing homes, it may not be imperative to keep a stock if they have robust local arrangements ensuring medicines are promptly accessible when needed.
Furthermore, implementing a widespread practice of stocking CDs in all nursing homes on a large scale could potentially lead to supply constraints. This could, in turn, restrict access to these medicines in other settings and potentially diminish their availability in the broader community.
It is paramount to strike the right balance in this regard, but it is essential to eliminate any barriers for those nursing homes where maintaining a stock would significantly benefit patients. This is precisely where expert pharmacy guidance and counsel become invaluable.
A complex challenge
Finding the right balance between timely symptom control and avoiding unnecessary dispensing is a complex challenge within care homes. Establishing a well-structured system for anticipatory medication that considers individual patient needs while also addressing environmental impact is crucial.
A well-functioning system for anticipatory medication hinges on seamless collaboration between healthcare providers, pharmacists and care home staff. This involves ensuring medicines are readily available in care homes, with clear guidance for swift administration based on evolving patient needs. This approach aligns with the government’s ‘One Chance to Get it Right‘ principle, underscoring the significance of prompt access to vital medications. It is ultimately aimed to provide residents in their final stages of life with timely and effective relief from symptoms, prioritising their comfort and dignity and reducing stress and anxiety among carers and family members.
Pharmacy professionals should lead and advocate for essential changes in licensing processes, aiming to enable nursing homes to maintain a stock of CDs. Their expertise in training staff and conducting audits is pivotal in ensuring safe and effective medication management. By taking the lead in these efforts, pharmacists can play a crucial role in advancing palliative care in care homes.
- 1Seymour JE, Kumar A, Froggatt K. Do nursing homes for older people have the support they need to provide end-of-life care? A mixed methods enquiry in England. Palliat Med. 2011;25:125–38. https://doi.org/10.1177/0269216310387964
- 2Controlled drugs: safe use and management. NICE guideline [NG46]. National Institute for Health and Care Excellence. 2016. https://www.nice.org.uk/guidance/ng46 (accessed November 2023)
- 3Managing medicines in care homes. Social care guideline [SC1]. National Institute for Health and Care Excellence. 2014. https://www.nice.org.uk/Guidance/SC1 (accessed November 2023)
- 4Palliative care for adults: strong opioids for pain relief. Clinical guideline [CG140]. National Institute for Health and Care Excellence. 2012. https://www.nice.org.uk/Guidance/CG140 (accessed November 2023)
- 5Controlled drugs in care homes. Care Quality Commission. 2023. https://www.cqc.org.uk/guidance-providers/adult-social-care/controlled-drugs-care-homes (accessed November 2023)
- 6Domestic controlled drug licensing in healthcare settings. Home Office . 2014. https://www.gov.uk/government/publications/domestic-controlled-drug-licensing-in-healthcare-settings (accessed November 2023)
- 7Controlled drugs and precursor chemicals: licence fees. Home Office . 2021. https://www.gov.uk/guidance/controlled-drugs-licence-fees (accessed November 2023)
- 8Novel coronavirus (COVID-19) standard operating procedure: running a medicines reuse scheme in a care home or hospice setting [Withdrawn]. Department of Health and Social Care. 2020. https://www.gov.uk/government/publications/coronavirus-covid-19-reuse-of-medicines-in-a-care-home-or-hospice/novel-coronavirus-covid-19-standard-operating-procedure-running-a-medicines-re-use-scheme-in-a-care-home-or-hospice-setting (accessed November 2023)
- 9Bowers B, Howard P, Madden B, et al. Is end-of-life anticipatory prescribing always enough? BMJ. 2023;p1106. https://doi.org/10.1136/bmj.p1106
- 10How to use the NEW 2022 GSF PIG in your practice. Gold Standards Framework. 2022. https://www.goldstandardsframework.org.uk/How-to-use-the-NEW-2022-GSF-PIG-in-your-practice (accessed November 2023)
- 11Delivering a ‘Net Zero’ National Health Service. NHS England. 2020. https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf (accessed November 2023)
3 comments
You must be logged in to post a comment.
You may also be interested in

Patient access to 24/7 palliative care medicines is ‘insufficient’, finds House of Commons-commissioned report

Lead paediatric palliative care pharmacists should be part of local plans, says RPS

Thank you, Emyr, for continuing to bang the drum on this topic. I worked on a project with a couple of Care Homes about 15 years ago when they were permitted to hold a small stock of CDs without a licence but by the time we got everyone's agreement, the law changed and the burden of the licence was regarded as too onerous for the home's owners.
I have long felt that we have developed such a blanket aversion to risk with CDs that it negatively impacts on patient care. It would be pefectly feasible to safely store, audit and use a small quantity of CDs in a nursing home with pharmacy support.
That period during Covid when we were able to use professional discretion was such a positive period for palliative care pharmacists and nursing staff and I know that no harm came to anyone in the area where I was working. Using very careful recording and monitoring we were able to save a huge amount of money and minimise the appalling waste too. I'd be happy to help if I can in any way to highlight this again although I'm now retired.
As someone involved in applying for CD license for an addictions setting it is a complicated process, and the HO offer little or no advice during the process, or communicate very clearly after it whether the license is granted or not. New licenses require a visit. And the advice on the visit seems to be dependant on the person who comes.
Noting each individual named on the license must be DBS checked (even if they've been checked for other reasons or hold the Scottish equivalent) and you need to name the person responsible for destroying stock CDs on it too - so they have to be identified. And if any of those names change you have to update the license and pay another fee (and DBS check).
I can understand the care homes not wanting to go anywhere near that process, and the government could do with refreshing the process to be clearer and more supportive and more able to prioritise patient care.
As a pharmacist leading a medicines optimisation in care homes (MOCH) team in Sussex along with my counterparts who together provide the service across the whole of Sussex we are very interested in seeing this legislation change for nursing homes.