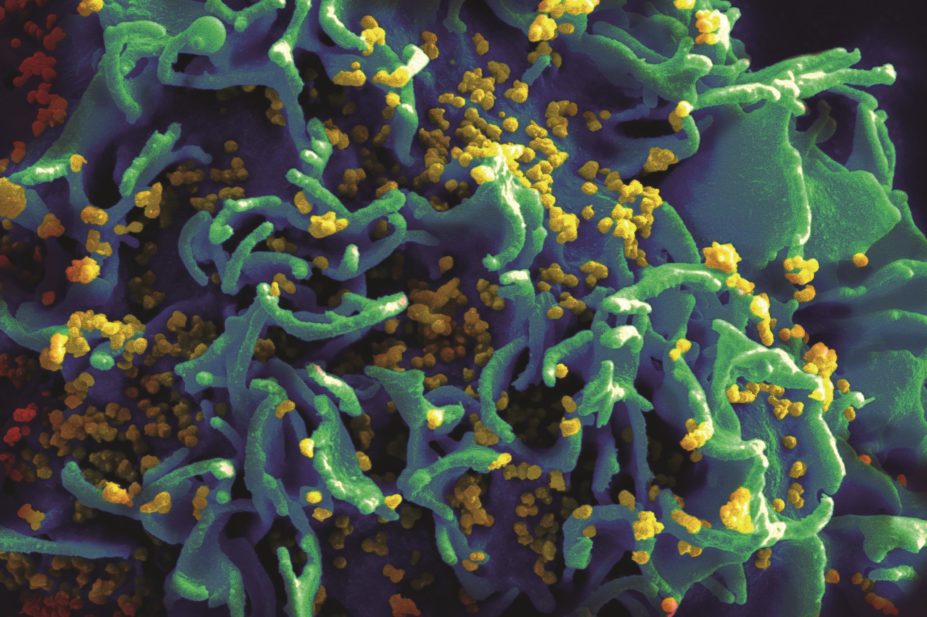
National Institutes of Health (NIH) / Wikimedia Commons
The number of people living with HIV in the UK continues to grow. Recent estimates from Public Health England in a new report ‘HIV in the UK 2016’ reveal that more than 100,000 people are living with the condition, but more than 13,000 are unaware of their status. Early diagnosis and treatment is pivotal in order to reduce transmission and provide a better prognosis for patients.
With the success of antiretroviral therapy (ART) and an increase in people newly diagnosed at an older age, the report shows that a generation of patients with HIV is living with a normal life expectancy. Currently, around one in three people living in England is aged 50 years or over. It is predicted that, by 2028, the proportion is expected to rise to more than 50%. Therefore HIV services will need to adapt to look after this growing group of patients.
The influential think tank, the King’s Fund, released its research report ‘The future of HIV services in England’ on 25 April 2017, outlining how HIV services have progressed in England, and the current challenges and opportunities that need to be grasped to ensure services can continue to meet the needs of patients.
The good, the bad and the ugly
The suppression of viral activity is a key marker of success for HIV clinical services. The Joint United Nations Programme on HIV/AIDS (UNAIDS) has set targets for HIV treatment and care to be achieved by 2020, and says that the epidemic can be reduced if:
- At least 90% of people with HIV have a diagnosis;
- 90% of the 90% diagnosed receive ART;
- 90% of those receiving ART achieve viral suppression.
The UK currently exceeds the targets for treatment access and viral suppression.
However, in terms of diagnosis, the UK is falling behind. One major factor that can affect how people access HIV testing and seek care is stigma, which has a significantly negative impact on the physical and mental wellbeing of HIV patients. Discrimination against individuals with HIV can result in reduced adherence to treatment and worse treatment outcomes. Additionally, stigma also undermines HIV prevention campaigns because it can lead to increased risk taking, non-disclosure and avoidance of health services.
In its report, the King’s Fund criticised the impact of the government’s 2012 reforms, when the Health and Social Care Act was created. With it, a new and complex model for commissioning and providing HIV prevention and care followed. A recent example of the impact of this was the scandal surrounding funding of pre-exposure prophylaxis (PrEP), used to prevent HIV infection, when NHS England decided it was legally unable to fund the medicine and said it was up to local authorities to decide. Eventually, after several court cases and appeals, the courts ruled it was within NHS England’s remit to decide whether or not PrEP should be funded.
The think tank recommended a stronger, more effective system of leadership, drawing together providers, commissioners and HIV patients, in order to overcome the fragmented system. It also recommended that local plans should focus on integration of services and be developed within the broader framework of sustainability and transformation plans (STPs).
HIV services in primary care
According to the King’s Fund research, although the quality of care patients received from specialist clinics was rated positive, feedback on the services provided by non-HIV specialists was mixed, and for GPs the feedback was mainly negative. Extending the role of HIV services into primary care could be one way of transforming them to meet future changing demand. But primary healthcare professionals, including GPs and pharmacists, will need to step up their knowledge and understanding of HIV if they are to provide better care for these patients.


