Shutterstock.com
Source: Shutterstock.com
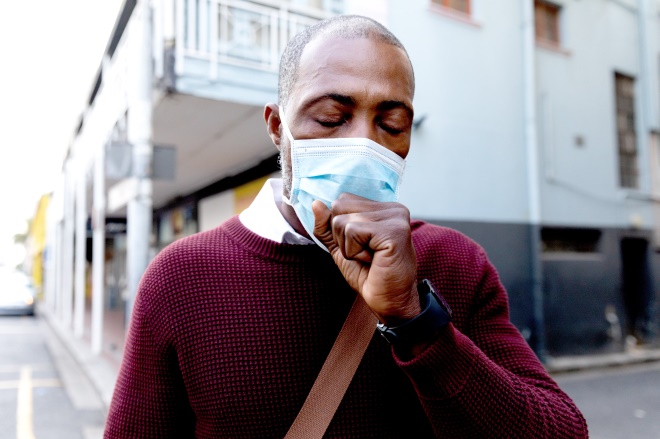
Public Health England (PHE) has published the results of a review into how different factors – including ethnicity, gender and obesity – can impact on people’s health outcomes from COVID-19. This may prove an important milestone in the understanding we have of this disease.
Previous published evidence indicates that male sex, older age, prior health conditions and deprivation may be associated with a higher risk of death from COVID-19. And there is increasing evidence that black, Asian and minority ethnic (BAME) populations are at greater risk.
The latest figures from the Intensive Care National Audit and Research Centre show that 67% of patients in critical care units with COVID-19 in England, Wales and Northern Ireland were white, while 27% were of a BAME background. This is despite people of a BAME background making up only 13% of the population in England and Wales in the 2011 census.
Patients of non-white ethnicity with COVID-19 also appear to be younger than those of white ethnicity (56 years vs. 60 years) and appear more likely to die from the disease. Excess deaths (observed vs expected) are around 1.5 times higher than expected for the Indian population, 2.8 times higher for the Pakistani population and 4.3 times higher for the black African population.
The PHE review confirms the trends highlighted in these data and builds on them. It points out that the death rates observed may be even worse than first thought, as baseline all-cause mortality data show that in usual times there are lower mortality rates in Asian and Black ethnic groups than the white population. This situation has been completely reversed by COVID-19.
Of course, as the PHE review points out, there may be several contributing factors as to why this is and the BAME group is heterogeneous.
For instance, it is well known that there is an overrepresentation of BAME populations living in areas with lower socio-economic status, and deprivation doubles the risk of dying from COVID-19.
Particular comorbidities, such as hypertension, cardiovascular disease and diabetes, are more prevalent in people with severe COVID-19. These comorbidities are also more prevalent in some BAME populations and may explain the increased risk of morbidity and mortality in this group.
Occupation may also play a role in the infection risk that various groups are exposed to. Indeed,
The Guardian reports that 61% of healthcare workers, including pharmacists, who have died from COVID-19 were from minority ethnic backgrounds, despite minority ethnic populations making up 44% of all NHS staff. At least four pharmacy staff who have died have all been from minority ethnic groups. A survey by the Royal College of Nursing indicates that BAME nurses may be exposed to much greater risk of infection with COVID-19, owing to a lack of personal protective equipment, compared with their white colleagues.
There could also be a cultural dimension: for example, public health messages in English may not be getting through to everyone. Different health-seeking behaviours and the increased amount of intergenerational cohabitation in some BAME populations may also play a part in the spread of the virus.
Data are still being collected, and it is encouraging that the long-standing health inequalities some BAME populations face are being looked into at the highest level, but it should not have taken a deadly virus for this to come to the fore.
The NHS has set up a new Race and Health Observatory, to help identify the specific health challenges facing people from BAME backgrounds and employers are being urged to risk-assess BAME employees — although there are concerns about how this is being applied in community pharmacy.
However, it is not as if we have not seen this before. This is a continuation of the trend seen in the H1N1 bird flu pandemic in 2009/2010. In England, those of non-white ethnicity experienced an 84% increased mortality risk compared to white populations during this pandemic, with the highest risk in those of Pakistani ethnicity.
As the Royal Pharmaceutical Society has stated, to some extent the PHE review merely “restates the problem”. The opportunity to finally address these inequalities cannot be missed again.