
Shutterstock.com
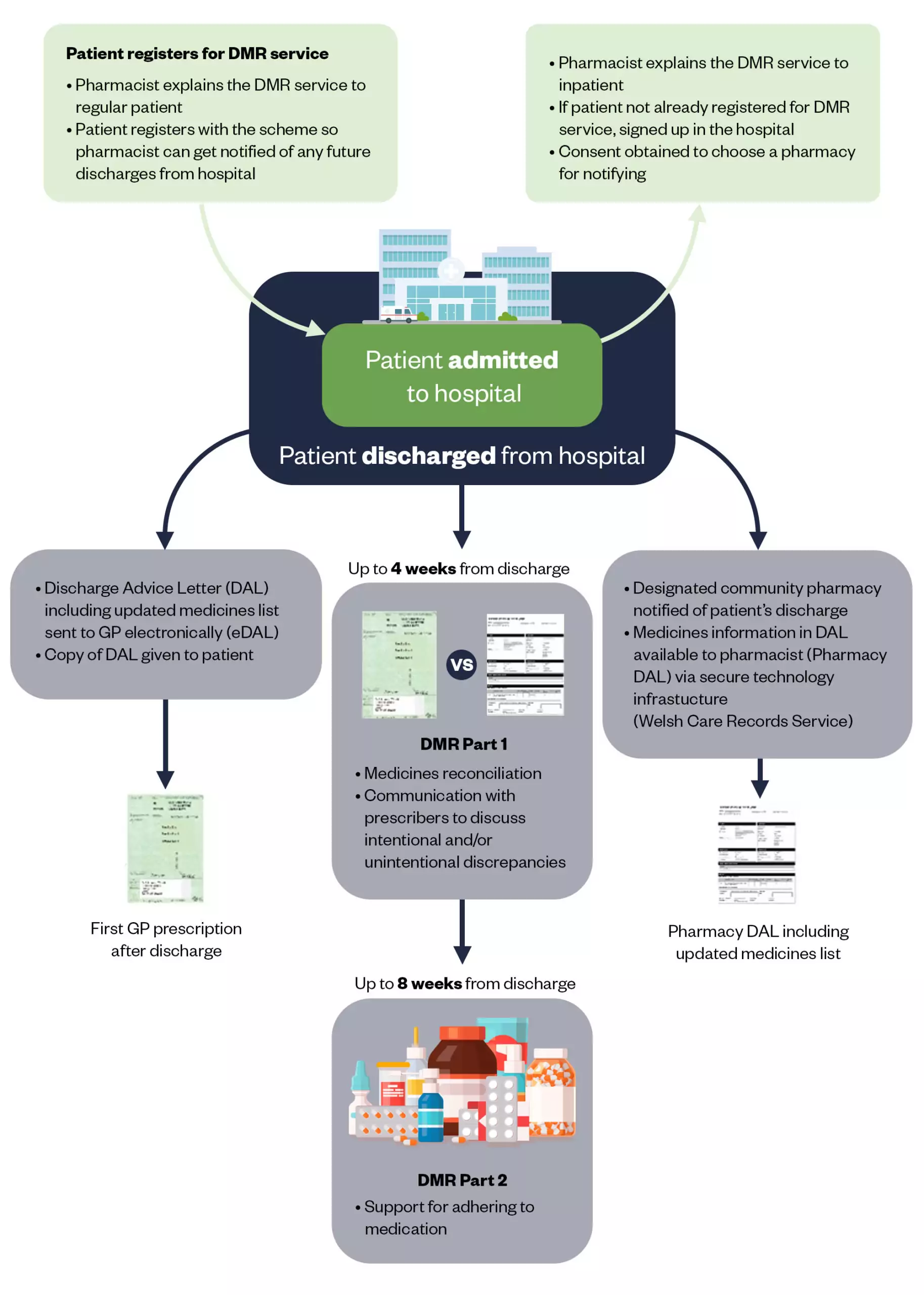
To improve the continuity of care between sectors, the Welsh government supported the introduction of a new community pharmacy service in Wales in 2011: the discharge medicines review (DMR). At the time, this service involved the pharmacist receiving paper discharge advice letters that were generated after a patient’s stay in a care setting, such as in hospital, and checking that the medicines information on that letter matched the medicines prescribed by the GP (see Figure).
In June 2023, our team attended the first Health Services Journal Digital Awards, where we were proud to be finalists and represent Wales with our 12-year-long journey of bringing digital transformation to the DMR service. This transformation was a collaborative approach between Digital Health and Care Wales, Community Pharmacy Wales (CPW), Cardiff School of Pharmacy and Pharmaceutical Sciences and the Welsh government. The collaboration has ensured a continuing development of the service based on service users’ needs. We thought this is a unique opportunity to share our learning with our pharmacy professional colleagues across the UK.
In 2014, the evaluation of the paper-based service reported a discrepancy rate of 1.3 items per DMR, meaning that — on average — for each review there was at least one discrepancy (intentional or unintentional) between the medicines prescribed by the primary care team post discharge and those that the patient should be receiving according to the discharging care setting. The evaluation also revealed an attractive 3:1 return on investment with £3m freed up through avoided A&E attendances, hospital admissions and drug wastage.
However, delivery of the service was challenging for community pharmacy staff owing to several barriers: identifying patients when discharged from hospital; timely access to the patient’s discharge information; and time consuming paperwork.
Not only did we take great care during the digital transformation to ensure no one was digitally excluded, but we also increased equity of care
Discussions with stakeholders suggested that technology could play an important role in overcoming these challenges. Funding was successfully secured from the government to develop an electronic DMR module in ‘Choose pharmacy’, the national pharmacy IT platform, and allow patients to nominate a pharmacy from which they can access the service.
As part of the development process, we interviewed patients and found that most were comfortable with giving pharmacists access to medication-related information in their records. We also asked community pharmacists what discharge information was essential for completing a DMR and how they would like to receive the information. There was a clear preference for electronic transmission, which informed the development of the electronic discharge letter pilot in 43 pharmacies in 2015. This was in line with the Professional Records Standards Body’s e-discharge standard.
An evaluation of the pilot in November 2015 revealed that pharmacists were very satisfied with the electronic functionality as it streamlined documentation and reduced transcribing errors. The electronic discharge letter was also perceived to have improved continuity between primary and secondary care. Following the pilot, the electronic discharge letter was gradually rolled out to pharmacies across Wales.
Engagement with key stakeholders has been, and is, central to all advancements of the functionality: there is a clinical reference group with representation from community pharmacist users and also CPW. Both provide assurance to the project board that the system meets the requirements.
Not only did we take great care during the digital transformation to ensure no one was digitally excluded, but we also increased equity of care. Patients were not required to use the technology and community pharmacists were already familiar with the ‘Choose Pharmacy’ IT system used.
More recently, we enabled pharmacy technicians to provide the DMR service, following a successful pilot. Pharmacists and technicians also now have access to the full electronic discharge letter, not just the medicines-related content. Hospital staff, meanwhile, said they wanted to view outcomes from completed DMRs on the patients they discharged. These became available for hospital staff to view from 2020.
As NHS Wales implements hospital e-prescribing systems, we are also ensuring that discharge medicines information is integrated into the hospital discharge letter and shared with pharmacies, maintaining the DMR’s electronic functionality.
Lastly, because we designed the system to provide easy access to structured data, we were able to complete several additional projects, including:
- In 2018, we completed a cross-sectional study, and established a reduction in the risk of medication errors, a key impact of the DMR on out-of-hospital care;
- In 2020, we completed a national routine data linkage study and found that having a DMR after a hospital discharge was associated with reduced risk of readmission within 40 days, improving patient safety.
Now, more than a decade on, we have a digital system that improves out-of-hospital care for all patients and, because we worked hard on the scalability of it, the benefits have materialised across the country. Since the introduction of the digital functionality, more than 63,000 DMRs have been completed, including more than 1,200 every month in the past year. If we extrapolate the 3:1 return of investment, the DMR has saved NHS Wales approximately £9m in the past decade. We are still going strong with improving the system, to continue meeting service users’ and population needs.
To promote all of this, we developed information videos aimed at hospital teams, community pharmacy teams and the public.
Figure: An overview of the Discharge Medicines Review Service in Wales
The Pharmaceutical Journal, reproduction from IPJ Vol. 38, June 2020
Acknowledgements
Our core team members are:
- Cheryl Way, national pharmacy and medicines management lead at Digital Health and Care Wales;
- Judy Thomas, director of contractor services at Community Pharmacy Wales;
- Andrew Evans, chief pharmaceutical officer for Wales;
- Karen Hodson, professor in pharmacy practice, MSc course director in clinical pharmacy and non-medical prescribing at Cardiff University.
We would also like to thank Rob James, who researched aspects of the DMR during his PhD at Cardiff University.


