Shutterstock.com
The COVID-19 pandemic hit the London borough of Brent hard; we have suffered the highest age–adjusted cumulative death rate in the UK.
During the first wave of the pandemic, there was a large number of hospital admissions owing to a high peak of infection.
Much of the high death rate could be attributed to the ‘compacted’ nature of the pandemic in Brent, where many people became ill in a short space of time, overwhelming A&E and intensive therapy units at an early stage of the pandemic, when knowledge about clinical management of the virus was only just developing.
However, it is also clear that there is a direct correlation between poverty, black and minority ethnic (BME) groups in Brent, and infection and mortality rates from COVID-19. As in many areas, the pandemic shone a spotlight on the existing health inequalities in Brent, and the relationship between long-term conditions such as diabetes, cardiovascular conditions, high blood pressure, chronic obstructive pulmonary disorder and asthma, and mortality following COVID-19 infection.
Brent Health Matters (BHM) is a specialist service within the outer north-west division of Central London Community Healthcare NHS Trust, which focuses on promoting public health and tackling health inequalities within Brent.
As the BHM clinical team, we focus on building relationships with patients who have not been engaging with their GP, offering a comprehensive health check in the patient’s home, including blood tests if required, and specifically focusing on type 2 diabetes mellitus.
Our clinical team includes nurses, dietitians, healthcare coordinators and pharmacists. We, the two BHM clinical pharmacists, were recruited to our posts in Easter 2022. As well as working to develop our role within BHM, we conduct structured medication reviews for patients who are non-engaging, housebound and on multiple, high-risk medications.
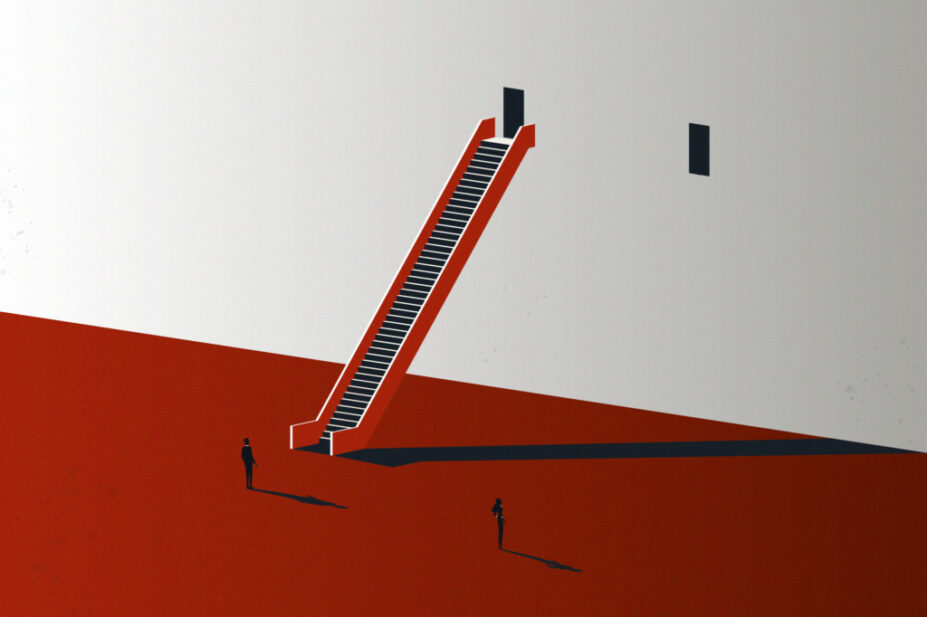
Often, these individuals just feel let down by the system … and we have the incredibly rewarding, yet onerous, task of reinstating their faith in the healthcare system
To achieve our goal of tackling health inequalities within Brent, we started by engaging with those patients who have been identified as “non-engaging” by their GP practice. The BHM clinical team were responsible for visiting the patient’s residence to not only provide the intended healthcare, but also conduct a welfare check. Often, these individuals just feel let down by the system for a multitude of reasons and we have the incredibly rewarding, yet onerous, task of reinstating their faith in the healthcare system. This may be through a holistic approach, regular contact and onward referrals to services that may be of great benefit to the individual.
Then, for our secondary workstream, we co-ordinated large-scale health events, where people were encouraged to have a comprehensive health check, including measuring body mass index, blood glucose, diabetes risk score and blood pressure. We also have a single-lead electrocardiogram system to help detect any heart rhythm abnormalities.
Patients were then offered a consultation with one of our senior nurses, pharmacists or dietitians, who discussed the results with them and, in some cases — using clinical discretion — would take them on to our caseload for further review.
The NHS King’s College clinical significance rating score is designed to categorise the significance of clinical interventions, based on the impact they have on the patient. This ranges from grade I (good practice without the intent to have a clinical effect on the patient) to grade V (averted death or major permanent harm). Between August 2022 and January 2023, the BHM clinical pharmacists made 82 grade III and 8 grade IV clinical interventions (see Box).
In 2020/2021, the cost of medicines prescribed in primary care in England was a staggering £9.42bn; therefore, it is imperative to keep cost effectiveness in mind. Moreover, reducing medicines wastage is a fundamental principle of medicines optimisation. For the 71 patients seen from between July 2022 and April 2023, the potential net cost saving to date is £512.91. The average cost of a non-elective admission is £3,571; therefore, the total cost saving for preventing eight non-elective admissions is £28,568, making the total potential saving for 71 patients more than £29,000.
As pharmacists in the BHM programme, we fulfil a very niche role that enables us to spend a great deal of time with our patients, allowing us to build a rapport and engage with them. As we are not limited by strict time constraints like pharmacists in other sectors, our patients feel listened to in the comfort of their own homes, often providing us with great feedback, which is incredibly rewarding.
The BHM programme continues to focus on patient engagement, which is measured via our key performance indicators, which include the number of referrals to other specialist services; number of diabetic foot checks completed; number of medication reviews completed; and the number of patients supported to register with a GP practice. The BHM pharmacists will continue to work closely with our counterparts in other sectors to ensure a seamless transfer of care.
Our future aspirations include integrating with primary care network pharmacists to receive referrals for those patients with complex polypharmacy, who are non-engaging and have poor management of their health conditions. Alongside this, we would like to undertake further courses to enhance our specialist skills; for example, working towards becoming advanced clinical practitioners.
Box: Patient story
‘Patient LH’
- Aged 76 years;
- From Pakistan;
- Patient and two children live in a single room within a shared flat;
- Two children aged under 10 years not attending school;
- Coronary angioplasty with stent insertion in Pakistan, taking medications that are posted over from Pakistan by wife.
Pharmaceutical interventions completed:
- Patient prescribed six indicated medications after his procedure in Pakistan, but GP only issued two indicated medications, one of which was based on outdated guidance;
- Referral to cardiology made by GP at the recommendation of the pharmacist. This was chased by pharmacist several times owing to urgency of requiring indicated medications;
- Patient seen by cardiology team three months later and appropriate medications prescribed;
- When completing medicines reconciliation, new errors identified from hospital: prescribed nebivolol 1.25mg tablets; given nebivolol 5mg tablets instead of 1.25mg (four times the prescribed dose); wrong label attached to medication — rosuvastatin label; no rosuvastatin supplied from hospital.
Actions taken:
- Prescribing hospital and pharmacy notified of error;
- Incorrect medications removed from home;
- Correct medications prescribed by GP;
- DATIX completed.
Clinical and social outcomes:
- Five medicines prescribed after cardiology review;
- Patient no longer experiencing chest pain to the same extent;
- Housing issue currently under investigation;
- Local school admission provided for his two children.
Health inequalities
The Royal Pharmaceutical Society’s policy on health inequalities was drawn up in January 2023 following a presentation by Michael Marmot, director of the Institute for Health Equity, at the RPS annual conference in November 2022. The presentation highlighted the stark health inequalities across Britain.
While community pharmacies are most frequently located in areas of high deprivation, people living in these areas do not access the full range of services that are available. To mitigate this, the policy calls on pharmacies to not only think about the services it provides but also how it provides them by considering three actions:
- Deepening understanding of health inequalities
- This means developing an insight into the demographics of the population served by pharmacies using population health statistics and by engaging with patients directly through local community or faith groups.
- Understanding and improving pharmacy culture
- This calls on the whole pharmacy team to create a welcoming culture for all patients, empowering them to take an active role in their own care, and improving communication skills within the team and with patients.
- Improving structural barriers
- This calls for improving accessibility of patient information resources and incorporating health inequalities into pharmacy training and education to tackle wider barriers to care.