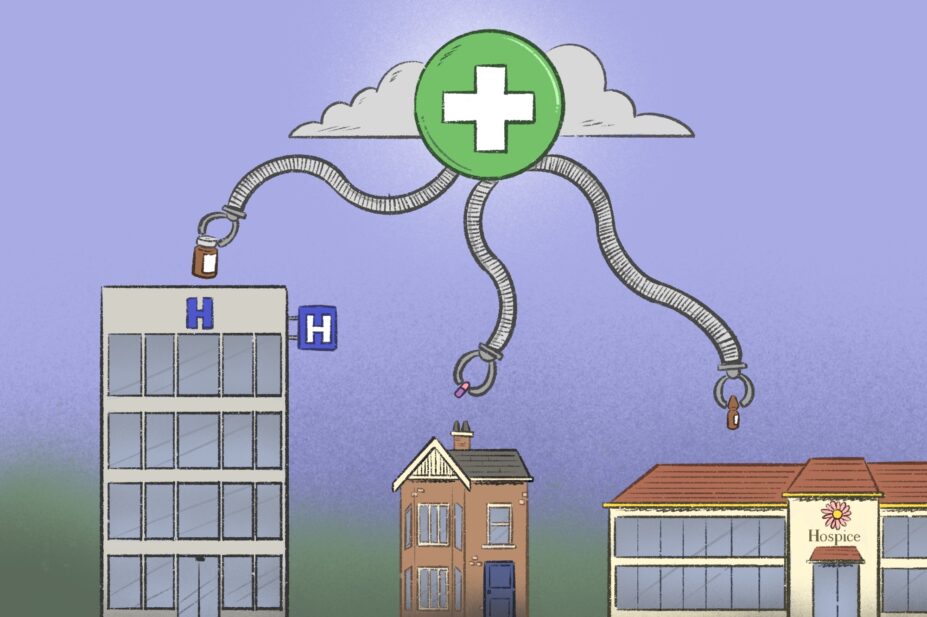
Wes Mountain/The Pharmaceutical Journal
Medicines management is an essential part of the complex activities required to deliver palliative care across organisations and locations, within and beyond the NHS. Good palliative care is only achieved when patients get maximum benefit and minimum harm from symptom control medication.
However, medicines management in palliative care is complex because it requires multi-step processes to be enacted in the context of pre-existing social factors, including: medication safety within a multi-occupancy home; interactions between different needs, such as symbolic interpretations of medication use in the context of end-of-life care; and capacity for advocacy1,2. Processes of decision-making, prescribing, monitoring and supply, administration and stopping or disposing of medications are even more problematic when someone moves between their home, hospital and hospice settings, requiring the coordination of care across service boundaries3.
Poor medication management leads to unnecessary suffering for patients, their families and carers
As a result, it is perhaps unsurprising that patients, carers and professionals experience several difficulties with trying to get the right palliative medications at the right time. Data suggest that approximately 20% of NHS serious incident reports (91 of 475 reports studied) involving patients receiving palliative care relate to prescription medications4. Of these, approximately 25% of palliative medication incidents relate to continuous subcutaneous infusions5.
Palliative medicines management in the NHS
Poor medication management leads to unnecessary suffering for patients, their families and carers. We need to develop systematic solutions to these problems that do not solely rely on individuals ‘going the extra mile’, as described by a family carer quoted in Box 1.
Box 1: Experience of a family carer
“I would pop back and forth [to the pharmacy]… because I was in there so much, we built up quite a good relationship. And so they would call me as soon as something was there. But that was mostly down to the fact that there’s one really good pharmacist in our local pharmacy. And she was really, really helpful. She was very proactive. When occasionally, there’d be a miscommunication between the palliative team and the GP about the nature of the prescription… she was really good about noticing if something didn’t really make sense, and then going back to the GP and then getting a change… but she was definitely going beyond the limits of what I think was reasonably her duties, and not everyone would have done that.”
The carer’s full account can be read here.
Neither the human nor system costs of not getting palliative medication management right have been adequately explored by policymakers, system designers, funders or providers. Hidden work that is unaccounted for in policies or service specifications is widespread and burdensome for patients, carers and professionals.
While policies promote increasing palliative care in community settings, the system still lacks equitable and inclusive ways to make this happen6. Commissioning of pharmacy services and inclusion of pharmacists into palliative care are highly variable across the UK, despite the 2023 NHS England specification for adult palliative and end-of-life care services, including a requirement for input from pharmacists with specialist skills and experience in palliative care within multidisciplinary teams7. Furthermore, integration of pharmacy services is a core tenet of the World Health Organization (WHO) strategy to improve palliative care worldwide8.
What needs to change?
Ensuring access to ‘the right medicines, at the right time, in the right place’ for symptom control in palliative care requires a whole systems approach.
We conducted a theoretically informed empirical ethnography ‘Getting prescription medications right at home, in hospital & hospice’ using ‘activity theory’ — a ‘whole system’ method to understand experiences of everyone involved in managing palliative medications9. This identified ‘hot’ (widely recognised challenges) and ‘cold’ (issues requiring greater attention) spots in the current system that need to be addressed to improve safety and confidence.
Participants identified the inclusion of pharmacists (and other pharmacy professionals) as essential for improving medication management processes in palliative care services. People receiving palliative care medication for symptom control should have direct and regular access to a pharmacist, trained in palliative care. They should also be able to receive a structured medication review and have shared decision-making conversations about deprescribing. This can only be achieved if the NHS increases the use of palliative care pharmacists in community services, acute hospital teams and hospices to enable working across system boundaries10.
Our evidence-based toolkit
Healthcare professionals will always need to work around system flaws to provide personalised palliative care, even as we advocate for wider structural changes in how palliative medicines are managed.
Meaningful choice can rarely, if ever, be achieved without engaging in positive risk-taking
Meaningful choice, including prioritising ‘what matters most’ for someone receiving palliative care, can rarely, if ever, be achieved without engaging in positive risk-taking. Therefore, building trust between patients, carers and healthcare professionals — and reducing the sense of isolation — is an essential component to improving palliative medicines management.
To assist with this, we created an evidence-based toolkit (see Box 2) to help bridge the gap between research and practice. The toolkit has been developed to support personalised improvements in palliative medication management systems in different contexts. Evidence to support the toolkit comes from observing more than 120 hours of everyday practice and informal conversations at home, in hospitals and in hospices. We spoke to 83 patients, informal carers and healthcare professionals, mapping out who does what and when.
The toolkit can be used as a self-assessment tool to highlight potential ways of improving the planning, funding and provision of services. We have also found it effective in prompting communication between stakeholders across system boundaries, helping to develop shared solutions and learn from each other11.
Box 2: Toolkit contents
- System quality indicators for commissioners and policymakers;
- Research infographic, summarising the take-home important messages from the research;
- Summary report, outlining recommendations for addressing hot and cold spots in the system, as well as a guide to using the other toolkit resources, including applying the model and using the palliative postcards in healthcare professional education and training;
- Interactive pictorial model of ideal and intended medication management processes, with illustrative stories and themed examples from our research, plus a detailed mapping of the realities of medication management;
- Top tips for patients and carers;
- Top tips for healthcare professionals;
- System quality indicators for commissioners and policymakers.
Adequate resourcing
We need better systems that help people collaborate effectively. Finding ways to facilitate a two-way discussion in real time, across roles, teams, organisations and locations, should be prioritised over asynchronous communication, where messages are left for someone to pick up. Building strong working relationships with colleagues in this way can help reduce workload and make the wider healthcare system more effective. Patients and carers need to be supported to talk about how they take their medications without fear of judgement, and they need to understand and identify the different professionals who can help them across various care settings.
Community pharmacy teams, hospital pharmacists and pharmacists in hospices working with people who are receiving palliative care must be adequately resourced and trained to support medication reviews with patients and carers, tailor advice to individual needs, explain reasons for changes in medications and advise on the practicalities of self-administration.
The burden placed on carers would also be reduced through services that deliver medication to homes. These services would also collect medications that are no longer required (including after a patient dies), even if they were dispensed from another pharmacy. Greater use of specialist link workers, such as integrated care community pharmacy technicians, could facilitate better communication between different parts of the healthcare system.
A healthcare system that learns from experience is one that seeks to improve. However, evidence and learning need to be translated into practical pragmatic tools for practice. A toolkit such as ours offers a way for everyone invested in improving palliative medicines management to work together to reduce waste and increase effective use of resources, in addition to improving the quality of care.
To make this change, sustainable pharmacists and pharmacy services must be integrated into palliative care models, regardless of whether the patient is at home, in hospital or in a hospice.
Find out more:
The official launch of the toolkit took place at the Marie Curie Virtual Conference on 13 February 2025.
Further information about applying the toolkit can be found in ‘What we learned from the REACT palliative care service’, published on 3 February 2025, by Zoe Edwards, research lead, advanced clinical practitioner, pharmacist, senior research fellow, Affinity Care Primary Care Network, University of Bradford.
Additional resources for community pharmacies are available from the RPS/Marie Curie Daffodil Standards initiative.
Acknowledgements
Written on behalf of the ‘Getting palliative prescription medications right at home, in hospital and hospice’ study team:
- Bryony Dean Franklin (UCL School of Pharmacy, London; Imperial College Healthcare NHS Trust, London);
- Margaret Ogden (PPI co-investigator);
- Anu Kajamaa (Faculty of Education and Psychology, University of Oulu, Finland); and
- Karen Mattick (University of Exeter Medical School, University of Exeter, Devon).
- 1.Pask S, Pinto C, Bristowe K, et al. A framework for complexity in palliative care: A qualitative study with patients, family carers and professionals. Palliat Med. 2018;32(6):1078-1090. doi:10.1177/0269216318757622
- 2.Redmond P, Grimes TC, McDonnell R, Boland F, Hughes C, Fahey T. Impact of medication reconciliation for improving transitions of care. Cochrane Database of Systematic Reviews. 2018;2018(8). doi:10.1002/14651858.cd010791.pub2
- 3.Medication without harm: Policy brief. World Health Organization. 2024. Accessed February 2025. https://www.who.int/publications/i/item/9789240062764
- 4.Yardley I, Yardley S, Williams H, Carson-Stevens A, Donaldson LJ. Patient safety in palliative care: A mixed-methods study of reports to a national database of serious incidents. Palliat Med. 2018;32(8):1353-1362. doi:10.1177/0269216318776846
- 5.Brown A, Yardley S, Bowers B, et al. Multiple points of system failure underpin continuous subcutaneous infusion safety incidents in palliative care: A mixed methods analysis. Palliat Med. 2024;39(1):7-21. doi:10.1177/02692163241287639
- 6.Palliative and end of life care . UK Parliament. 2022. Accessed February 2025. https://researchbriefings.files.parliament.uk/documents/POST-PN-0675/POST-PN-0675.pdf
- 7.Specialist Palliative and End of Life Care Services Adult Service Specification . NHS England. January 2023. Accessed February 2025. https://www.england.nhs.uk/wp-content/uploads/2023/01/B1674-specialist-palliative-and-end-of-life-care-services-adult-service-specification.pdf
- 8.Palliative care. World Health Organization. 2020. Accessed February 2025. https://www.who.int/news-room/fact-sheets/detail/palliative-care
- 9.Yardley S, Francis SA, Dean Franklin B, Ogden M, Kajamaa A, Mattick K. Getting palliative medications right across the contexts of homes, hospitals and hospices: protocol to synthesise scoping review and ethnographic methods in an activity theory analysis. BMJ Open. 2022;12(3):e061754. doi:10.1136/bmjopen-2022-061754
- 10.Getting palliative medications right at home, in hospital and hospice. UCL. 2024. Accessed February 2025. https://www.ucl.ac.uk/psychiatry/sites/psychiatry/files/system_quality_indicators.pdf
- 11.Francis SA, Ogden M, Bradley N, Yardley S. P-174 Getting palliative medications right: a multicentre impact project translating research into practice. Poster Presentations. Published online November 2024:A75.2-A76. doi:10.1136/spcare-2024-hunc.190
You may also be interested in
Government to ‘strengthen’ out-of-hours support for palliative care services

Support for pharmacies providing palliative care urged as hospices get cash injection
