“Pharmacy has had more ‘visions’ than a hippie community,” said Jonathan Buisson, government relations senior manager at Alliance Healthcare.
He was speaking during a Q&A session at The Pharmacy Show in Birmingham on 15 October 2023, challenging a panel of community pharmacy representatives on why the sector then has “a poverty of ambition” at the negotiating table with the government.
“Why aren’t we asking for £5bn in funding with a big programme of services that we could be delivering?” he added.
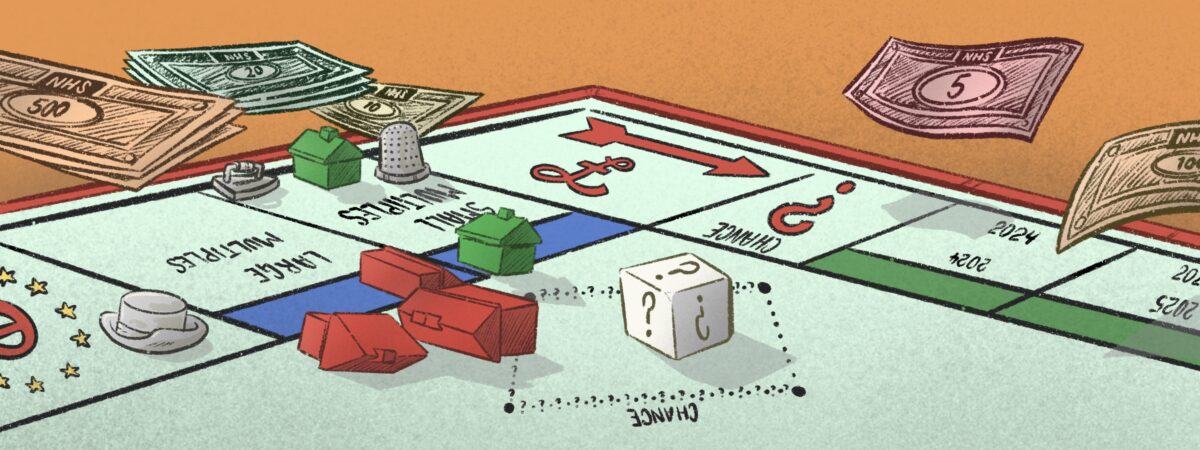
With the five-year community pharmacy contract ending in March 2024, Buisson’s question is becoming increasingly urgent. According to the government’s own figures, community pharmacies in England have lost £1.6bn since 2015/2016, largely owing to the impact of inflation on government funding that has been frozen at £2.592bn each year since 2017/2018.
The result is a persistent decline in the number of pharmacies in England, with the latest NHS data published in October 2023 revealing that there are now 11,414 active community pharmacies — the lowest number since 2015/2016.
Large multiples are also withdrawing from the pharmacy market. In June 2023, Boots announced plans to close 300 branches in 12 months and, in October 2023, The Pharmaceutical Journal revealed that LloydsPharmacy has dramatically reduced its branch numbers by 90% over the past 18 months.
All the while, pressure on pharmacies is increasing. According to NHS data, community pharmacies dispensed 94,500 items each on average in 2022/2023 — an increase of 13.5% from the average of 83,300 items in 2015/2016.
Also speaking at The Pharmacy Show, Janet Morrison, chief executive of Community Pharmacy England (CPE), conceded that that five-year contract has had “cumulatively, a terrible, terrible impact” on the sector.
“I don’t think anyone is ever going to say, ‘let’s have a five-year deal again’,” she said.
However, it is hard to say how much influence CPE will have at the negotiating table before the impending general election in 2025. NHS England will soon be conducting its own evaluation of community pharmacy clinical services to help it “make effective decisions regarding clinical services for the future community pharmacy sector”.
What is certain is that, as talks start for the 2024/2025 contract, there is no shortage of evidence that more funding could unlock a wide range of community pharmacy services that will benefit patients and the NHS as a whole.
As Buisson, and many others, noted at The Pharmacy Show, nearly every pharmacy representative body has set out its expectations for the future of the sector. Within the past year alone, the National Pharmacy Association, the Company Chemists’ Association, the Royal Pharmaceutical Society and CPE have all published such reports.
There are several common threads between these expectations, including implementing a ‘Pharmacy First’ service in England, wider use of independent prescribing, more screening services, more vaccination services and using pharmacogenomics as part of medicine optimisation.
They are understandably broad in scope, using national data for the largest impact. The CCA report, for example, says that pharmacies could screen more than 5 million people each year for undiagnosed hypertension, shifting care for 200,000 newly diagnosed patients with hypertension away from GP practices each year.
This sounds like a hopeful prospect. But in Derby, where there are vast health inequalities, we have heard that some patients are reluctant to enter a pharmacy, leaving it up to pharmacy teams to build their own hypertension services in local community centres instead.
With these ‘visions’ from pharmacy bodies so focused on the national issues, the danger is that the vital local ambitions get lost. With that in mind, The Pharmaceutical Journal would like to invite any UK pharmacy professional to submit a case study that shines a light on the quiet triumphs of small services. These will be published as part of a collection of articles on the future of pharmacy. We want to hear about initiatives set up to meet local ambitions that could be replicated in communities facing similar circumstances across the country. Whether the service is limited to a small area or across a wide region, in a community or hospital setting, we would like to hear about it.
We’ve heard the views of what national influencers think pharmacy should look like in the next five to ten years, but now it is your turn. What are your local ambitions for pharmacy practice? What unique initiatives are essential to these ambitions going forward, and how can they be replicated elsewhere? As pharmacy faces increasing demands from the government and from patients, now is the time for innovation in the way services are provided. PJ
Send us your examples
Please email us with a brief description of any locally commissioned initiative you are involved in that has successfully addressed the needs of your patients and could also be offered in similar localities: editor@pharmaceutical-journal.com
We are interested in any scheme — big or small — targeting any population group. In your email, please outline the project, who was involved, any results (no matter how provisional) and anything else you would like to say. An editor from The Pharmaceutical Journal will be in touch to discuss next steps.