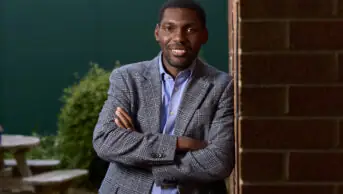
Paul Stuart
Tase Oputu has had a varied career in the lead up to her election as chair of the Royal Pharmaceutical Society’s English Pharmacy Board in June 2023.
From working in Tanzania with Voluntary Services Overseas, to her role as a former school governor, to holding several senior hospital pharmacy manager roles in hospitals in London and the South East of England, her experience has made her “skilled at effectively bringing people together”, she said in her — ultimately successful — nomination statement.
These experiences will inevitably prove invaluable as the profession navigates a wellbeing crisis and an array of major changes that include pharmacists becoming independent prescribers at the point of registration from 2026.
The Pharmaceutical Journal spoke with Oputu about how she plans to rise to the challenge and focus on her passion for supporting inclusion and diversity.
Why did you stand for chair of the English Pharmacy Board?
Anybody who knows me knows that I stand for inclusion and diversity, and I am very vocal in encouraging people to put themselves forward for senior positions, not just in their day-to-day work, but in positions of influence, and especially in our pharmacy bodies. So, any opportunity we have to be part of decision making or influencing policy that’s going to affect us as pharmacy professionals is important to take. The hashtag has been ‘representation matters’, and it’s important because of the experience that we have as black and minority ethnic pharmacists.
I make the distinction between black and minority ethnic because, actually, the experience of black pharmacy professionals is quite different. I’ve been a pharmacist now for 28 years, and I have been very surprised at how few black pharmacists have made it to senior positions. I was one of the first black pharmacy professionals to be on the English Pharmacy Board, and I was so surprised that it was me that was going to be that person. It was a shock to me. I couldn’t believe it.
We need to lean in — we need to have a seat at the table
And then the opportunity arose to stand for chair and I could have chosen not to stand, but I chose to stand to say that, actually, even if I didn’t get it, I still put myself forward. And, therefore, I was being true to what I stand for, which is that we need to put ourselves into these positions. We need to lean in. We need to have a seat at the table. We need to be part of this and not stand back.
What has been the reaction of fellow pharmacists since you were elected?
I have had contact from numerous people, and I’ve been absolutely humbled by the reaction. And what’s made me feel that I did the right thing is that I have heard them say that they are now going to put themselves forward just from seeing me in this position, and that they feel that they can do it, and even if it’s just one other person that puts themselves forward and is successful, then it’s 100% satisfaction for me for that to happen.
Do you have a role in supporting the health and wellbeing of practising pharmacists?
The RPS workforce wellbeing survey that came out a few months ago, showing that over 80% of pharmacists were at risk of burnout, was just so distressing.
Part of our role in the RPS, and so part of my role, is making sure that we’re able to take that data and drive some of the advocacy work that we do on things like protected learning time. I think that’s the most important thing at the moment — advocating for pharmacists to have an understanding of downtime, and having a good work-life balance.
It’s also important to come at it from an inclusion point of view because people can experience even more stress and strain through things such as bullying and harassment, through discrimination, just for being themselves at work.
We need to ensure that we have leaders and individual pharmacy staff who are culturally competent, who demonstrate anti-racist behaviours, who are allies to all the different protected characteristics, which all feed into wellbeing and how people are at work because we want pharmacy to be an attractive profession.
It may be a bit more tangential, but because of the pressure of medicines shortages, the impression that people may have of pharmacy is that it isn’t an attractive career because you don’t have time to do anything and you’re just constantly chasing your tail.
But we want pharmacy to be a really attractive profession for people to be in, for people to see that we’re welcoming, that we’re culturally competent, that we understand each other and that we’re nice to each other. That’s where I think that my role with advocacy can bring all that together.
What difference will all newly registered pharmacists from 2025/2026 being qualified as independent prescribers make to the profession?
It’s a step change. It’s one of the biggest things to happen to the pharmacy profession. And for us in the RPS, it really is about how we support those clinicians now through their life as prescribers, from the moment when they arrive as early-career prescribers to becoming more specialist. Personally, I think that the patient who walks through the door probably sees the pharmacist more as a clinician these days. And that’s been a little bit of an evolution.
That ability to do more clinical work will be where we can have a really big impact on health inequalities
That ability to do more clinical work will be where we can have a really big impact on health inequalities. As a pharmacist you know your patients, you know the patients who are coming to you regularly, you know what the problems are, what the issues are, and we are increasingly now able to support them through being able to prescribe. You can identify those people who may not have ordinarily gone to their GP for a certain problem, and those are the patients who will benefit so much more by having us as prescribers in the community.
But I don’t want it to be forgotten that there is a legacy of pharmacists who are not independent prescribers, some who never want to be independent prescribers and don’t want to go down that particular route.
There are also pharmacists who are not patient facing — my role, for example, is not patient facing —and there is so much that they also contribute to the care and wellbeing of patients.
So, independent prescribing is one thing, but we have a breadth and a depth within the pharmacy profession of so many different skill sets and areas.
The recently published Community Pharmacy Workforce Survey showed that there was a vacancy rate of 16% in community pharmacy. Did you experience similar problems in hospital pharmacy?
I don’t have exact data, but my experience is that it has been hard to find staff. We’d have vacancies, and I can’t say that those vacancies were never filled, but too often we would get vacancies.
But there is a growing recognition now — with pharmacy being the third largest health professional workforce — of the value of pharmacy professionals for their clinical skills in particular, which means that, as that value is recognised, the services that we offer also increase. And that also creates a little bit of tension between who’s there to actually deliver those extra services. So, the aspiration to increase those numbers is really, really important.
The ‘NHS Long Term Workforce Plan’ set out an intention to train almost 5,000 new pharmacists each year by 2031/2032. Is this realistic?
What I do know is that we have to make sure that we’ve got really good pharmacy workforce numbers everywhere — in the NHS, in community pharmacy — so we need to know where everybody is, and where the gaps are. It would have been very disappointing if there hadn’t been a target to get to. So, let’s try to reach that.
The plan also said the government would consider introducing pharmacy degree apprenticeships — what’s your view on this?
It offers something for people who cannot or do not want to be at university, and, in terms of access to the profession, is an MPharm the be all and end all, or the only way to access the profession?
But what I would say is important is that we are all part of an open conversation about it, and that it doesn’t just happen with one set of employers and not include the rest of the profession.
Education and training need to be part of that conversation, the professional leadership bodies need to be part of that conversation, and I don’t think we should be limited in our options.
When it comes to sustainability in healthcare and the NHS, do you think the pharmacy profession understands it?
I would say that the RPS really is leading the way in terms of pharmacy leadership on this and — a disclaimer — I will say that I’m quite passionate about this particular topic as well.
That passion has kind of been ignited through the RPS in terms of the divesting piece of work, and also the setting up of its sustainability policies.
But I’m a bit worried about saying that people get it, because I think ‘oh well, I get it’, therefore everybody must get it, but maybe people don’t. The health impacts of climate change and air pollution can’t be ignored. It’s real. It’s happening now all around us. And from my perspective — remember that I’m very passionate about inclusion and diversity — these things, such as climate change and air pollution, do have a disproportionate impact on the people who are contributing the least to it.
You may also be interested in

Henry Gregg: ‘The only way to slow down pharmacy closures is to start closing that £2.6bn funding gap’

Dale and Appelbe’s Pharmacy and Medicines Law: covering ‘essential ground in the most highly regulated areas of healthcare’