Pharmacy teams are often only seen as medicines experts, but we do so much more than that. In community pharmacy, we frequently step in to fill the gaps left by social care. In GP and primary care network settings, pharmacy roles range from managing long-term conditions to writing repeat prescriptions — and much more. But to meet the ambitions of the new NHS ten-year plan, we need a cultural shift and broader mindset. We need an increase in the workforce across all roles and every healthcare professional working together to utilise everyone’s strengths, deliver consistent care, minimise the postcode lottery and close the ever-widening health inequalities gap.
As outlined in the NHS ten-year plan, community pharmacy “will have a vital role in the proposed neighbourhood health service, bringing health to the heart of the high street”. While this is exciting, it is not anything that we didn’t already know and it is already happening every day. Community pharmacy has long been the heart of its neighbourhood. Conversations about increasing access to healthcare, freeing up appointments and investing in better estates are not new. There are already more than 10,000 pharmacy premises in England where patients can walk in at any time, often without an appointment, including evenings and weekends.
The ten-year plan is a blueprint, but it doesn’t give us great detail, so we need to think innovatively
The ten-year plan is a blueprint, but it doesn’t give us great detail, so we need to think innovatively. For example, could government investment be directed into our existing community pharmacy estates — such as building a second consultation room — and moving various services fully into community pharmacy, either from secondary care or other sectors in primary care, particularly general practice?
In February 2025, a report published by the the Company Chemists’ Association (CCA) — ‘Increasing vaccination uptake through community pharmacy’ — discusses the value of commissioning community pharmacies to deliver more vaccinations. This is something that would be straightforward to implement as so many pharmacies already deliver flu and COVID-19 vaccinations, as well as many private vaccinations. This could free up more than 10 million GP vaccination appointments each year.
What is the main barrier to doing this? Financial stability.
We need to ensure the remuneration is appropriate and from new funding. Concerns from GPs often relate to potentially losing funding — since they are private businesses too — and confidence in the clinical skills of pharmacy teams. Some GPs also prefer to mix minor illness appointments with more complex cases to break up the day and catch up on clinic work.
However, freeing up capacity should be seen differently: it’s not just an opportunity to see more complex cases, but to spend a bit longer with patients. A 15-minute appointment could give clinicians some breathing space — imagine the benefits for patients.
We all need to work together in primary care to make this work — that includes better relationships between pharmacy and surgery teams. All healthcare professional training should include cross-sector training; for example, GP trainees spending time in community pharmacy and pharmacy trainees working in general practice.
Long-term ambition with short-term action
Every community pharmacy in England is a ‘Healthy Living Pharmacy’ under contractual framework requirements, with the ambition being ‘Making every contact count’. This is a crucial component of shifting the focus from sickness to prevention. The ten-year plan talks about giving community pharmacy a bigger role in prevention by expanding pharmacy’s role in vaccine delivery and screening for cardiovascular disease and diabetes risk. Over time, community pharmacy will be securely joined up to the single patient record to help provide a seamless service — and to give GPs oversight of patient management.
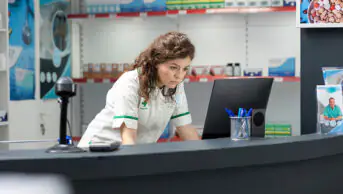
The vision is that all at-risk patients could have an annual health check at their community pharmacy — measuring blood pressure, cholesterol, HB1aC, BMI and waist circumference. This does not need to stop at screening — pharmacies could run a 12-week programme with weekly check-ins, coaching patients to making lifestyle changes to reduce any concerning readings, as well as helping people make sustainable behavioural lifestyle habits. As more pharmacists quality as independent prescribers, they could start to prescribe for these conditions directly. For this, we need full digital integration with NHS systems, sharing information via patient records and the ability to order blood tests and prescribe safely.
The ten-year plan also talks about expanding the role of community pharmacy in managing long-term conditions, linking them to the single patient record. This must go beyond ‘just’ prescribing, focusing on helping people live longer, healthier lives through behavioural change support. Does this need to be done by a pharmacist or a pharmacy technician, or could it be done by a trained healthy living champion? This will be time-consuming on pharmacy and will need to be remunerated appropriately, but I know that this investment (likely to be more affordable than other healthcare professionals) will save the NHS money in the long run.
Action points
So, what do we need in community pharmacy to maximise our role in the ten-year plan?
- We need to look inwards, at our workforce and skill mix, and embrace portfolio careers. We need protected learning time, and to ensure that every member of the team is working to the top of their licence;
- Using automation wherever we can to free up capacity for teams to spend time with patients. Cost is often a barrier, but contractors may need to consider investing now to save money in the future and to increase revenue in the long term;
- The Department of Health and Social Care and HM Treasury must invest in community pharmacy now to ensure that ‘sickness to prevention’ is a central focus, so that fewer people end up using NHS services and maintain good health in the community;
- Interoperability with the rest of the NHS;
- Community pharmacy and general practice should work together and trust each other — there is enough work out there for everyone.
Community pharmacy has a great future and a big role to play in the NHS ten-year plan. What we have shown time and time again is how we work with pace, agility and versatility. If anyone can make change happen, it’s community pharmacy.
Conflicts of interest
Shilpa Shah is chief executive of North East London Local Pharmaceutical Committee. She writes in her own capacity.
You may also be interested in
CCA calls for next Welsh government to accelerate digital access for pharmacies

GPs should have dedicated, monitored email address for pharmacy communications, says new contract