Abstract
Aim
To explore community pharmacists’ training needs for the provision of services to drug misusers.
Design
Cross-sectional survey.
Subjects and setting
Pharmacy managers of all registered community pharmacies in NHS Grampian, Scotland (n=120).
Method
Administration of a self-completed postal questionnaire based on a previously validated measure. Two reminders were sent out. Questions included previous training in drug misuse, attitudes to developing motivational interviewing skills and perceived training needs.
Results
99 pharmacists (82.5%) completed the questionnaire. 79 (80.6%) had experience of dispensing methadone. Interest in learning motivational interviewing skills was indicated by 67 pharmacists (67.7%). 53 pharmacists (53.5%) had received previous professional training on the management of drug misuse; 70 (73.7%) wanted further professional training on drug misuse.
Conclusions
Pharmacists’ interest in learning motivational interviewing techniques indicated that the feasibility of such training should be explored. Despite a high proportion of respondents dispensing methadone, almost half had not received professional training on the management of drug misuse. Community pharmacists are interested in receiving more training on this topic and local provision of specialist training should be considered.
In the past decade, the role of community pharmacists in the treatment of drug misusers in the UK has developed rapidly. Many pharmacists now have considerable experience of service delivery and working with this client group.1,2 Currently, there are 1,162 community pharmacies in Scotland of which 71 per cent dispense drugs for drug misusers; specifically 69 per cent dispense methadone for over 9,000 patients. Sixty-five per cent of these patients consume their methadone under pharmacist supervision in the pharmacy.1
Drug misusers receiving methadone under supervised self-administration visit the pharmacy daily for their methadone dose. In a study of drug misusers’ views of pharmacy services it was clear that a good relationship, built on friendly exchanges with the pharmacist and other staff, was extremely important in how drug misusers feel about themselves and behave in the pharmacy.3,4 It is recognised in the literature that pharmacists see methadone patients more often than any other health or social professional.2 It has also been suggested at a strategic level that pharmacists could have a wider role in the management of drug misusers.5
In conducting previous research in this field pharmacists have commented that they could “do something” constructive while a drug misuser takes his or her supervised methadone.6 For example, they could provide counselling specifically related to opiate dependence.
Before developing this concept further, we undertook a training needs assessment of community pharmacists, based in the NHS Grampian area of Scotland, for developing specific counselling skills geared to drug misusers. Previous research indicates that 66.5 per cent of community pharmacists in Scotland have received training in drug misuse.7 In Grampian specifically, the proportion was 71.4 per cent. Enhancement of community pharmacists’ skills in the management of drug misusers is particularly relevant at this time.
A new community pharmacy contract is currently being developed in Scotland8 and services for the management of drug misusers are likely to be delivered under locally negotiated contracts. Service specifications for those are likely to be developed nationally, and training and demonstration of new competences such as motivational interviewing might be relevant to include. In England and Wales, the new contract is already in operation with drug misuse services classified as an advanced service. A national survey of pharmacies in England and Wales is ongoing (personal communication, Victoria Manning, King’s College London).
Methods
All 123 community pharmacies currently operating in NHS Grampian in December 2004 were identified from the NHS Grampian General Pharmaceutical Services list.
A brief questionnaire was developed based on a validated questionnaire used previously.1 Topics covered included demographics, services to drug misusers and training in drug misuse with additional new sections on training in health behavioural change techniques. This paper presents the data in training on drug misuse and health behavioural change.
The questionnaire and a reply-paid envelope were posted to the responsible community pharmacist in each pharmacy at the beginning of December 2004 (120 in total, since three pharmacists each had responsibility for two part-time pharmacies). Where necessary, up to two reminders were sent during January 2005. Data were entered into an ACCESS database and exported into SPSS for analyses. Descriptive statistics were produced.
The manager and scientific adviser of Grampian Research Ethics Committee advised that this project did not require ethical review under the terms of the governance arrangements for research ethics committees in the UK.
Results
Response rate and demography
Ninety-nine pharmacists (82.5 per cent) completed and returned the questionnaire. Table 1 shows sample characteristics of participants. Seventy-nine participants (80.6 per cent) had experience of dispensing methadone to persons being prescribed it for drug misuse.

The median number of current methadone clients was 8 (interquartile range 3, 20). Of those dispensing methadone, 75 (94.9 per cent) supervised consumption in the pharmacy with the median number of clients supervised being 6 (interquartile range 2, 14). Participants were asked if they offered clients face-to-face advice on the management of drug misuse. Seventeen (17.5 per cent) indicated they always did, 63 (65 per cent) indicated they sometimes did and 17 (17.5 per cent) indicated they never did.
Training on drug misuse
Just over half of participants indicated they had received professional training on the management of drug misuse (Table 2).
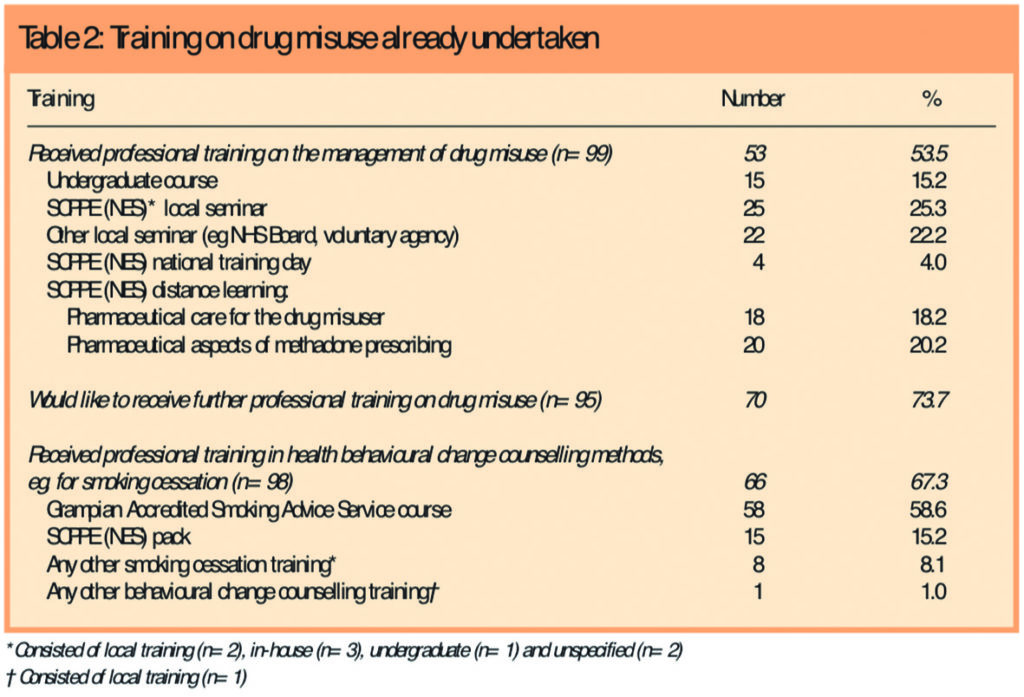
Most commonly this was through locally held events organised either by the Scottish Centre for Post-Qualification Pharmaceutical Education (SCPPE) — now NHS Education Scotland (NES) Pharmacy — NHS Grampian or by a local voluntary agency, or through distance learning co-ordinated by the SCCPE. Almost three-quarters of participants (73.7 per cent) indicated they would like to receive further professional training on drug misuse.
Training on health behavioural change methods
Two-thirds of participants (67.3 per cent) had received training in health behavioural change counselling methods (Table 2). With the exception of one respondent, the training attended had been related to smoking cessation, mostly provided locally.
Perceived training needs
In response to an open question 35 pharmacists (35.4 per cent) identified areas where they wanted further training in managing drug misuse. These are categorised in Table 3. Motivational and counselling skills were specified most frequently, followed by management of drug misuse generally and management of withdrawal specifically.

Sixty-seven respondents (67.7 per cent) provided contact details for the purpose of participation in research on the value of training in specific counselling skills for use in managing opioid dependent clients.
Discussion
The needs assessment indicated that most community pharmacists in NHS Grampian were providing services for drug misusers. However, only just over half had received specialised training in this topic, and over two thirds reported a need for (further) training.
The response rate of 82.5 per cent must be regarded as high for participation of any professional group in a postal survey. We can be reasonably confident that the findings of this survey represent the majority of community pharmacists based in NHS Grampian. Because the topic of the survey was drug misuse, it could be argued that the sample may be biased towards pharmacists with an interest in serving this client group. In the present sample, 80.6 per cent of respondents were involved in dispensing methadone. This proportion is higher than the 71.5 per cent of community pharmacists who were reported to dispense drugs to drug misusers in Scotland as a whole in 2000.7 However, given the steady increase in demand for the service, and the areas of particularly high misuse in NHS Grampian, this figure has face validity. Nonetheless it may be that pharmacists who do not dispense methadone were represented to a greater extent among the non-responders.
Given the high proportion of respondents dispensing methadone, it is surprising that only just over half had received training in the management of drug misuse. Most of this was accessed from local, rather than national providers. This proportion is substantially lower than the Scottish proportion receiving training in drug misuse which was 66.8 per cent in 2000.7 Over two-thirds of participants indicated that they would like to receive further professional training on drug misuse and it may be timely to review local course provision in this topical area. Further issues of accessibility may need to be explored. The Royal College of General Practitioners provides training on the management of drug misuse which has been extended beyond GPs to provide training to other professionals, including pharmacists.9 The Scottish Executive has supported 20 pharmacists who are currently undergoing this training.10 NES Pharmacy provides training and is currently revising a distance learning package which may address some of the issues raised by pharmacists, particularly in more remote areas. However, this will not address counselling skills development. Scottish Training on Drugs and Alcohol (STRADA)11 exists to improve the skills of professional staff addressing drug and alcohol misuse throughout Scotland. Courses are freely available to those employed in health, social work services and non-statutory organisations. Community pharmacists are eligible to attend these courses but daytime provision makes attendance dependent on securing locum cover in addition to all other issues of access. NHS boards could offer greater support either financially or by facilitating locum cover to enable additional pharmacists to take up such opportunities.
A greater proportion of community pharmacists had taken part in training related to health behavioural change methods with a specific emphasis on smoking cessation. Given the established evidence base that counselling provided by community pharmacists can improve smokers’ quitting rates,12 it is encouraging that two-thirds of participants had participated in such training. It has been hypothesised that improving outcomes for opiate-dependent pharmacy clients may be better achieved if behavioural change counselling skills, specifically motivational interviewing,13 were imparted to community pharmacists.14 However despite the wide evaluation of motivational interviewing in the treatment of addictions generally, there is a lack of evidence relating to community pharmacists administering such methods for pharmacy treatment adherence generally15 or in the treatment of drug misusers specifically. When respondents were asked to identify specific areas they would like to cover in training, motivational interviewing and counselling skills were mentioned most by those specifying particular areas of interest. As our survey was offered within the context of assessing interest in this area of training, there will have been an element of suggestion influencing responses. Nonetheless, the idea of learning motivational interviewing skills related specifically to drug misusers was met with enthusiasm with two-thirds of respondents indicating a willingness to be involved in further research aimed at developing such training in community pharmacists.
The future
Since conducting this survey, we have secured funding from the Chief Scientists’ Office of the Scottish Executive and we are in the process of developing and evaluating a novel training package of motivational interviewing skills for community pharmacists for use in the management of drug misuse.
About the authors
Isobel Cameron, MA, Dip Applied Psychometrics, is research fellow,
Catriona Matheson, PhD, MRPharmS, is senior research fellow, and Christine Bond, PhD, FRPharmS, is professor of primary care in the Department of General Practice and Primary Care at the University of Aberdeen.
Correspondence to: Dr C. I. Matheson, Department of General Practice and Primary Care, Foresterhill Health Centre, Westburn Road, Aberdeen AB25 2AY
References
- Matheson C, Bond CM, Pitcairn J. Community pharmacy services for drug misusers in Scotland: what difference does 5 years make? Addiction 2002;97:1405–11.
- Sheridan J, Barber N. Drug misuse and HIV prevention: attitudes and practices of community pharmacists with respect to two London Family Health Authorities. Addiction Research 1997;5:11–21.
- Matheson C. Views of illicit drug users on their treatment and behaviour in Scottish community pharmacies: implications for the harm reduction strategy. Health Education Journal 1998;57:31–41.
- Matheson C. Privacy and stigma in the pharmacy: the illicit drug user’s perspective and implications for pharmacy practice. Pharmaceutical Journal 1998;260:639–41.
- Scottish Executive Pharmacy Working party on Drug Misuse Drug Misuse and Community Pharmacy. Implications for pharmaceutical care. Edinburgh: Scottish Executive; 2004.
- Matheson CI, Bond CM, Cameron IM, Lawrie T, McNamee P, Robinson A, Eagles L .A feasibility study of supervised administration of buprenorphine in community pharmacies. Final Report, Chief Scientist Office, Scottish Executive, 2004 (Ref CZG/2/103).
- Matheson, CI, Bond CM, Pitcairn J. Scottish community pharmacy services for drug misusers: a five-year follow up survey of attitudes and practice. Final Report, Chief Scientist Office, Scottish Executive, 2001 (Ref CZ9/4/2/7).
- Scottish Parliament. Smoking, Health and Social Care (Scotland) Act 2005. Edinburgh: Stationery Office Ltd; 2005.
- Royal College of General Practitioners. RCGP Substance Misuse Unit. Available at www.rcgp.org.uk/drug/ (accessed 5 may 2006).
- Funding announced for pharmacists to undertake management of drug misuse training. Pharmaceutical Journal 2005;275:435.
- Scottish Training on Drugs and Alcohol. Available at www.projectstrada.org/website/ (accessed 5 May 2006).
- Sinclair HK, Bond CM, Lennox AS, Silcock J, Winfield AJ. Knowledge of and attitudes to smoking cessation: the effect of stage of change training for community pharmacy staff. Health Bulletin 1998;56:526–39.
- Motivational interviewing. Available at www.motivationalinterview.org (accessed 5 May 2006).
- Scales R, Miller J, Burden R. Why wrestle when you can dance? Optimizing outcomes with motivational interviewing. Journal of the Anerican Pharmaceutical Association 2003:43(Suppl):S46–7.
- Possidente CJ, Bucci KK, McClain WJ. Motivational interviewing: a tool to improve medication adherence? 2005 American Journal of Health-System Pharmcists; 2005;62:1311–4.


