The Heart of Birmingham Teaching Primary Care Trust serves an inner-city area with a population of 311,773 registered patients.[1]
The PCT faces many challenges because its residents experience some of the worst health inequalities in the UK. Life expectancy is short compared with the rest of England and varies considerably between wards by up to 8.5 years for men and six years for women.[2]
In the light of these challenges and world- class commissioning targets, the PCT adopted eight strategic objectives. These included improving services, access to services and outcomes for people with long-term conditions.[3]
One widely acknowledged method of improving patient access to health information and support is through greater use of pharmacy services.[4]
Studies have shown that patients visit pharmacies more than their general practices: 84 per cent of adults visit a pharmacy each year, with an average number of 14 visits a year, compared with an average of 5.5 GP consultations per registered patient per year.[5]
The use of pharmacies is, therefore, a natural focus for greater education and support of patients, including for long-term conditions such as asthma.
One service that can be offered by pharmacies to help optimise patient medication and information is the medicines use review (MUR). The range, number and quality of MURs undertaken by community pharmacies, however, varies greatly.
Research has indicated that this is likely to be due to skill-mix differences between pharmacy teams, including levels of confidence of pharmacists and incentives within local areas.[6]
To encourage an increased uptake of MURs, the PCT, Birmingham Local Pharmaceutical Committee and GlaxoSmithKline agreed an MUR partnership project, involving focused education and support to pharmacists over several months.
All partners share a common agenda to improve patient outcomes by providing high- quality and cost-effective treatment and management of appropriate patients with asthma; increasing the number of effective MURs conducted in Birmingham was recognised as a way to help achieve this goal.[7]
The joint working initiative was underpinned by the principles outlined by the Association of the British Pharmaceutical Industry.[8]
This paper considers whether a partnership approach between a PCT, an LPC and a pharmaceutical company might help to motivate pharmacies to begin providing MURs, or increase the number of MURs conducted. Furthermore, would this change in behaviour be sustained in the longer term once the project had ended?
Method
The project was designed to encourage pharmacies to undertake medicines use reviews on patients with asthma, with the aim of helping them to use their medicines more effectively, identify any problems and provide advice; where appropriate, recommendations about changes to medication would be made to the patient’s GP.
All community pharmacies in the PCT area were invited to participate in the project, which would provide them with education and support to start or increase the volume and quality of MURs conducted. Fifty-five per cent of pharmacies (n=44) agreed to take part in the project and receive education and support. In return they would commit to increasing their number of MUR asthma reviews. The project support ran for nine months between April and December 2008.
In preparation for an increase in the number of MURs, the participating pharmacies received two clinical training events in March 2008 delivered by a respiratory specialist nurse employed by the PCT. These focused on improving the pharmacists’ knowledge to conduct an effective MUR.
Among the areas covered were understanding respiratory equipment such as the In-Check Dial, a device that measures inspiratory effort when using an inhaler, and training to ensure accurate measurement of a patient’s asthma control via the asthma control test (ACT) questionnaire.[9]
The training also allowed pharmacists an opportunity to role-play an asthma MUR as a way of improving practice and confidence.
During the nine-month project, the project team monitored progress of participating pharmacies and provided further training sessions at four pharmacy protected learning events. The additional training sought to identify and address barriers to the increased uptake of the MURs, including those of clinical knowledge, confidence or of a logistical nature. The PCT and the LPC then provided solutions where possible, such as specific education sessions, to address these. A clinical refresher course was provided in September 2008 (month 7) by a consultant in respiratory medicine.
All patients with asthma were invited by pharmacists to undergo an MUR when presenting with prescriptions. Reviews included exploration of patients’ current treatment, their understanding and levels of self-reported adherence.
Asthma control was assessed via the asthma control test[7]
and any indications of sub-optimal asthma management by the patient were explored.
Results
Between April 2008 and March 2009, the percentage of pharmacies providing MUR services in the Heart of Birmingham Teaching PCT increased from 61.9 per cent to 88 per cent (an absolute increase of 26.1 per cent) when compared with the same period one year earlier (Table 1). Over the same period, the absolute increase observed across the West Midlands was 11.8 per cent, and across England 9.7 per cent.[10]
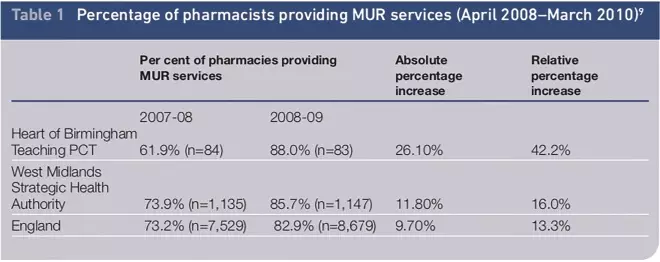
Table 1. Percentage of pharmacists providing MUR services (April 2008–March 2010)[9]
A comparison of the total number of MURs conducted in 2008–09 highlighted an absolute rise in the Heart of Birmingham Teaching PCT of 11.5 MURs per 1,000 patients. This was greater than both the increase observed by the strategic health authority (8.5) and the increase across England (8.1) (Table 2).
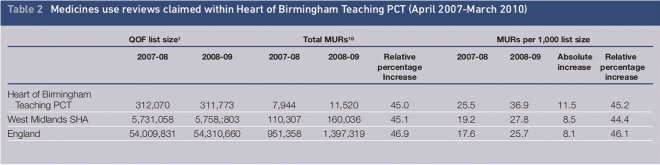
Table 2. Medicines use reviews claimed within Heart of Birmingham Teaching PCT (April 2007–March 2010)
The sustainability of the total number of MURs was assessed to February 2010. Over the 11-month period to when the latest data were available, there was a rise of a further 15.4 per cent on the 2008–09 totals for the corresponding 11 months (n=9,739 to 11,235). Additional information was collected on 944 of the MURs conducted by pharmacies participating in the project. In these reviews, 33 per cent of patients (n=307) were believed by the pharmacists to be non- compliant with their medication. Of these, 15 per cent (n=46) were referred to their GP, while 13 per cent of compliant patients were also referred (n=80) (Table 3).
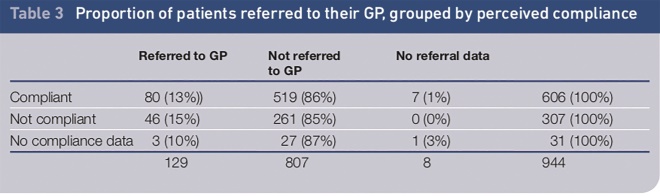
Table 3. Proportion of patients referred to their GP, grouped by perceived compliance
The likelihood of patient referral to a GP was not significantly different between those regarded as compliant and those who were non-compliant. However, patients were found to be more likely to be referred if their asthma control test score was lower, which indicated less control of their symptoms. The average asthma control test scores for patients referred to a GP was 13.8 (SD 4.24, CI 13.1–14.6) while the average asthma control test score for those not referred to a GP was 16.8 (SD 4.98, CI 16.4–17.1). It has been suggested that a score of 20 or higher was found to be the most discriminating cut-off to define totally controlled or well controlled asthma; a score of 15 or lower was identified as the most discriminating cut-off to define asthma that was poorly controlled or not controlled at all.[11]
No formal qualitative evaluation of the project was conducted to elicit detailed views about the project’s impact, but the anecdotal feedback and formal comments offered suggest that the project had motivated some pharmacies and provided them with the knowledge and confidence to initiate a new MUR service:
The MUR project kick-started the MUR process within the pharmacy — starting mainly with asthma MURs — but soon branching out across different disease areas. (Pharmacist)
Increased know-how and confidence to conduct an MUR was reported, including increased knowledge around devices, inhaler technique education, spacers and general clinical awareness. Communication skills for engaging patients and reviewing their needs were also enhanced by the project:
The project gave additional confidence in communicating to patients. The confidence came from clinical confidence and experience. (Pharmacist)
[The project] created greater links with patients, improved the communication between patients and pharmacists. It helped me learn how to speak to patients to uncover their needs. (Pharmacist)
Importantly, pharmacists also reported positive patient outcomes from the reviews.
The patients who received MURs generally had very poor inhaler technique, even after regular visits to the GP and asthma clinics. By correcting their inhaler technique, the patients were made to feel better. By delivering the education, the confidence in the pharmacist was increased. (Pharmacist)
… by using the In-Check [Dial] we were able to clarify, was the device right for the patients? This was very valuable for the patients. (Pharmacist)
Discussion
The project was implemented as a practical service development exercise rather than an academic project with a view to publication. For this reason, baseline measurements and data are limited, which restricts the degree to which the findings can be extrapolated to other areas. The project nonetheless provides interesting insights that may support the development of similar initiatives.
The aim was to measure two primary objectives. First, could the delivery of a nine-month supported MUR educational project in the primary care trust drive an increase in the number of MURs conducted within the PCT? Second, would this detailed approach enhance the skills of pharmacists and motivate them sufficiently to ensure a sustained increase one year after the end of the project?
Data comparing the number of pharmacies conducting MURs during the 12 months that incorporated the project, to the number in the comparable period one year earlier, shows notable increases in the PCT relative to both the national average and that for the strategic health authority. This may provide quantitative evidence to support qualitative views expressed that the project motivated pharmacies to begin conducting MURs.
It is encouraging that the total number of MURs per 1,000 list size increased by a greater amount in the primary care trust than across both the strategic health authority and England, despite starting at a higher baseline. It may be perceived that a ceiling effect may limit any potential increase from such an intervention, but this did not appear to be the case. It is also encouraging that having increased MUR uptake significantly during the project that it continued to increase in 2009-10, albeit by a more modest amount. This may be evidence of the sustainability of this project and the legacy of a detailed and supportive intervention.
Despite the encouraging results, we must be cautious about making any direct association to the project as it was not possible within the scope of this work to control for external factors and wider influences on MUR uptake. For example, comparisons of those pharmacies wholly immersed in the project with those not included would not be valid.
Several pharmacies not formally involved in the project were exposed to some materials and education messages. Similarly, energy and enthusiasm created by the project may have been disseminated among the pharmacy community, hence making any comparisons subject to bias.
We were also aware of MUR uptake promotional activity in a large pharmacy chain that did not join the project. These factors may skew any associations and conclusions about differences between the pharmacy groups in or out of the project.
Nevertheless, despite the difficulties in interpreting the data, we are encouraged that the findings of MUR uptake were positive and the overall target of the project was achieved. We are also encouraged that the rate of MURs conducted was sustained in the 11-month period after the project concluded, and continued to climb.
One natural challenge to the defined goal of the project to increase the volume of MURs, is that increased numbers is no guarantee of increased quality or value to patients. The qualitative feedback, however, suggests that may have been an outcome. Healthcare professional feedback is consistent with the objectives to enhance skills and confidence and position pharmacists to add greater value to patients in the community. This was also viewed as positive.
The use of the asthma control test in reviews and the increased likelihood of referral of those with lower scores, may also be hypothesised as being an indicator of a good quality review.
It is difficult to draw too many conclusions from the limited referral data gathered, but the significant difference in the propensity of pharmacists to refer according to the asthma control test score may support a hypothesis that this is a practical and acceptable tool in this setting, to support decision-making and patient dialogue. Research into the appropriateness of referrals, however, would be necessary as part of exploring this.
Further lessons can be drawn from the collaboration with a pharmaceutical company. GSK provided support in the development, delivery and follow through of the project. Their role was non-promotional and consistent with the goal of helping the PCT to optimise the management of asthma patients and ensure appropriate patients received appropriate classes of medication in line with guidelines from the British Thoracic Society and National Institute for Health and Clinical Excellence. The benefit for GSK is that if this improvement occurs, they would be likely to see an increase in prescriptions of their medicines roughly equal to the current proportion of prescriptions in this therapeutic area.
GlaxoSmithKline provided the In-Check Dial devices and non-promotional patient focused materials to support MURs. The company also supported the primary care trust to raise the profile of the project with pharmacies, helped with the project management of the initiative and maintained momentum within pharmacies by providing personal encouragement and the offer of support throughout the nine-month period.
Conclusion
This joint project between the primary care trust, local pharmaceutical committee and GlaxoSmithKline resulted in a significant increase in MURs and the number of pharmacies conducting these. The increased delivery of MURs was sustained after the conclusion of the project.
We believe the education and support offered to these pharmacies overcame some of the well-researched barriers to these services being offered more widely to patients. The clinical training provided by this project is likely to have enhanced the skills and increased the confidence of community pharmacists to offer MURs and may have a long-term beneficial effect.
This project has shown that if pharmacists are supported with training and support they are likely to increase the number of services offered to the local populations.
About the authors
John Morrison is head of medicines management, Sajj Raja is community pharmacy development manager/ prescribing adviser and Isaac Otomewo is prescribing adviser, all at Heart of Birmingham Teaching Primary Care Trust.
Duncan Short is health outcomes consultant for Wales and the Midlands and Heath Heatlie is programme lead, modelling and analytics, both at GlaxoSmithKline UK
Correspondence to: John Morrison (email: John.Morrison6@nhs.net
References
[1] NHS Information Centre [Online]. Quality and Outcomes Framework for 2009. Available at: www.ic.nhs.uk. (accessed 18 May 2011).
[2] Heart of Birmingham Teaching Primary Care Trust Public Health Report 2009/10. 2010. Available at: www.bhwp.nhs.uk/ (accessed on 18 May 2011).
[3] Heart of Birmingham Annual Report 2007/08. Available at: www.hobtpct.nhs.uk (accessed 6 July 2011).
[4] Department of Health. 2008. Community Pharmacy Use: Quantitative and Qualitative Research. Available at: www.dh.gov.uk/ (accessed 18 May 2011).
[5] NHS Information Centre 2009. Trends in Consultation Rates in General Practice 1995 to 2008: Analysis of the QResearch database. Available at: www.ic.nhs.uk (accessed 18 May 2011).
[6] Blenkinsopp A, Celino G, Bond C Inch J. Medicines use reviews: the first year of a new community pharmacy service. Pharmaceutical Journal 2007;278:218–23.
[7] Portlock J, Holden M, Patel S. 2009. A community pharmacy asthma MUR project in Hampshire and Isle of Wight. Pharmaceutical Journal 2009;282:109.
[8] ABPI. Guidance notes on joint working between pharmaceutical companies and the NHS and others for the benefit of patients. 2009. Available from: www.abpi.org.uk/ (accessed 6 July 2011).
[9] Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P et al. 2004. Development of the Asthma Control Test: a survey for assessing asthma control. Journal of Allergy and Clinical Immunology 2004;113:59–65.
[10] NHS Information Centre [Online]. 2009. General Pharmaceutical Services in England 1999-2000 to 2008-09. Available at: www.ic.nhs.uk/ (accessed 18 May 2011).
[11] Schatz M, Mosen DM, Kosinski M, Vollmer WM, Magid DJ, O’Connor E, et al. Validity of the Asthma Control Test completed at home. American Journal of Managed Care. 2007;13:661–7.
