Introduction
Medicines use reviews (MURs) are about helping patients use their medicines more effectively. The aims of MURs are to improve patients’ knowledge of, and adherence to, medicines by establishing their actual use and understanding of their medicines.[1]
The MUR service faces several challenges, such as lack of time and staff cover.[2],[3]
Another major challenge is the lack of acceptance of the pharmacist’s role in carrying out MURs by both GPs and patients. Patients are also more used to a six-monthly or annual review at their surgery than reviews by pharmacists.[3]
The National Pharmacy Association and Primary Care Pharmacists’ Association propose evaluation of MURs by using quality of service measures, including patient feedback analysis, assessment of the quality of referrals to GPs and community pharmacists’ assessment of their service.[4]
The evaluation of pharmacist and GP perceptions of MURs has been widely reported.[2],[5],[6]
. there is little evidence to support the effectiveness of MURs in fulfilling the aims.
The aim of this study was to determine whether patients benefit following MURs and whether certain groups of patients derived more benefit than others. This was assessed using three outcome measures:
- Analysing patients’ perceived benefit from MURs
- Pharmacists’ interventions following MURs
- The outcomes of public health initiatives arising as a result of MURs
Method
NHS ethics approval was sought but deemed unnecessary since the study was a service evaluation. Postal questionnaires were sent in December 2008 to all patients who had undergone an MUR over the three-month period from August to October 2008 at Dean & Smedley Pharmacy, Derby. Patients were asked to return completed questionnaires in prepaid envelopes. MURs were carried out by two regular pharmacists at this branch. Some MURs were conducted for patients taking fewer than three medicines as prescription intervention MURs.
The questionnaire consisted of three statements designed to ascertain patients’ perceived benefit from the MUR, with respect to knowledge gained about their medicines, side effects and compliance. A five-point Likert scale (“strongly agree” through to “strongly disagree”) was used to elicit responses to statements on the questionnaire. The questionnaire also collected patient demographic data, patients’ medical conditions and the number of prescribed medicines taken.
Completed MUR forms were studied to determine what proportion of MURs had led to an intervention suggested by pharmacists. Patient medication records (PMRs) were examined to see how many of these interventions were implemented. MUR forms were also examined to determine whether the pharmacist had explored the patient’s smoking status and if enrolment on to the pharmacy smoking cessation scheme was advised, where appropriate. For patients who did enrol onto a smoking cessation scheme following an MUR, the success rate of smoking cessation was observed.
Results
There were 152 MURs carried out during the study period. A response rate of 53 per cent (81 out of 152 patients) was generated from the postal patient questionnaire, of which 40 patients are male and 41 are female. Table 1 shows the age range of the patients and Table 2 shows the number of prescribed medicines for the patients. The population sampled was found to be affected by a variety of medical conditions (Table 3).
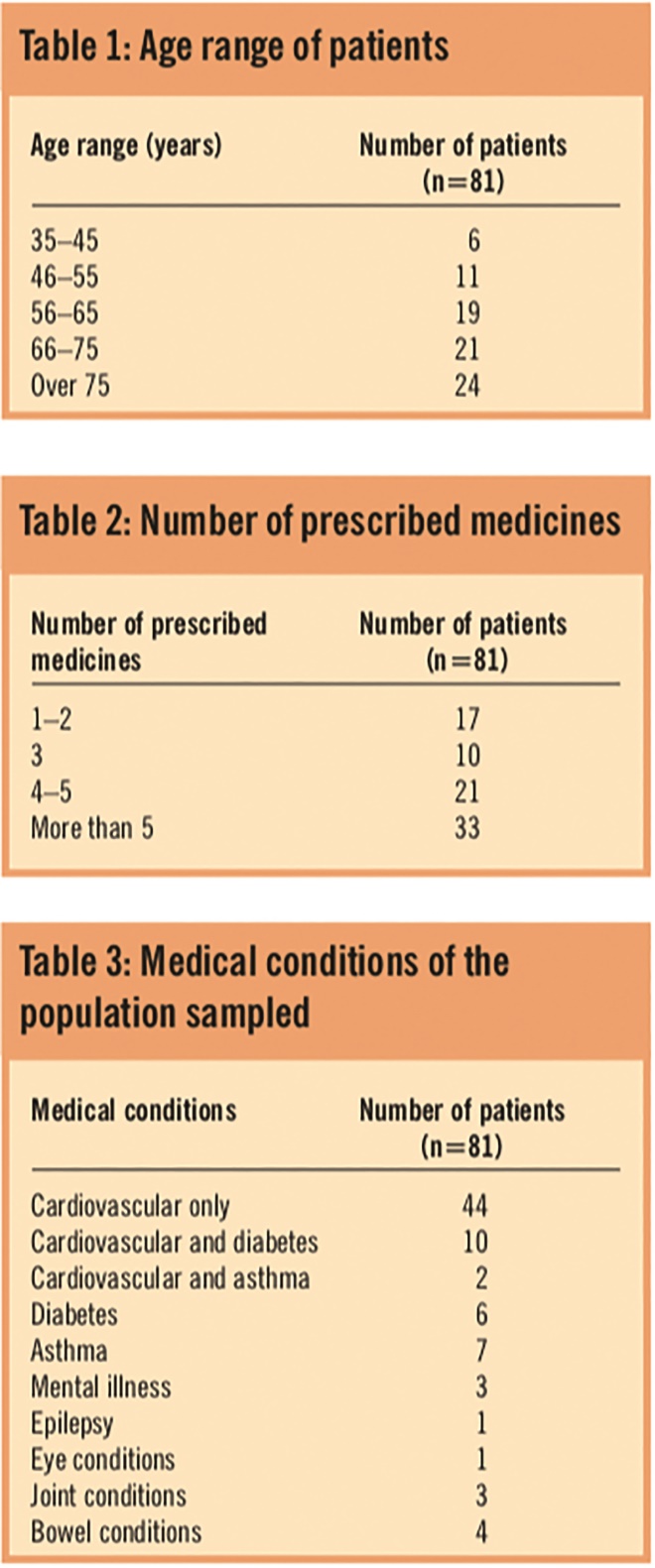
Tables 1, 2 and 3: Age range of patients; Number of prescribed medicines; and Medical conditions of the population sampled
Statements
In response to the statement “I learnt more about my medicine(s) after the MUR with the pharmacist”, 55 respondents (68 per cent) either strongly agreed or agreed. Subgroup analysis by age showed a trend towards older patients learning more about their medicines than younger patients (35/45 [78 per cent] >65 years versus 20/36 [56 per cent] <65 years). However, this was not statistically significant (χ2=3.57, P=0.06). There was no significant difference in the proportion of patients perceiving benefit between patients taking three or more prescribed medicines versus patients taking less than three medicines (45/64 [70 per cent] versus 10/17 [59 per cent], respectively; χ2=0.37, P=0.54).
In response to the statement “the medicines use review has made me more aware of side effects from my medicine(s)”, 47 (58 per cent) either strongly agreed or agreed that MURs have made them more aware of side effects from their prescribed medicines, 14 (17 per cent) were uncertain and 19 (23 per cent) either disagreed or strongly disagreed. A significantly greater number of older patients thought the MURs made them more aware of their medicines’ side-effects than younger patients (32/45 [71 per cent] >65 years versus 15/36 (42 per cent) <65 year, χ2=5.96, P=0.01). There was no significant difference in the proportion of patients perceiving benefit between patients taking three or more prescribed medicines versus patients taking less than three medicines (39/64 [61 per cent] versus 8/17 [47 per cent], respectively; χ2= 0.57, P=0.45).
In response to the statement “I feel that I take my medicine(s) in the right way and at the correct time after speaking to the pharmacist”, 67 (83 per cent) either strongly agreed or agreed with this statement. There was a trend towards patients over 65 years thinking they had gained more benefit than patients under 65 years. This was not statistically significant (40/45 [89 per cent] >65 years versus 27/36 [75 per cent] <65 years; χ2=1.82, P=0.18). There was no significant difference in the proportion of patients perceiving benefit between patients taking three or more prescribed medicines versus patients taking fewer than three medicines (53/64 [83 per cent] versus 14/17 [82 per cent], respectively; χ2=0.00, P=0.96).
Pharmacist interventions
Of the 152 MURs conducted during the study period, the pharmacist made 15 interventions (9.9 per cent): addressing three prescription errors; two changing of medication due to side effects; seven dose optimisation; two addressing non-compliance; and one change of formulation. Of the 15 interventions, five were found to have been implemented on examination of PMRs.
Promoting healthy lifestyles
Out of the 152 patients, 83 (55 per cent) were asked about their smoking status and 11 were found to be smokers. These 11 patients were offered support to stop smoking using the Derby City Primary Care Trust’s “Fresh start” smoking cessation programme that is offered in the pharmacy. Of the 11 patients who were found to be smokers, four enrolled onto the “Fresh start” programme and successfully quit smoking.
Discussion
This study has demonstrated that MURs do result in some benefit for patients. It is certainly the case that many patients perceive they benefit from MURs, particularly with respect to timing and method of administration. Although there is little research on patients’ views of MURs, one study showed that pharmacists believe MURs enhance patients’ correct use of medicines.[6]
Furthermore, a previous audit conducted by Lloydspharmacy showed customer satisfaction with the MUR service.[7]
It is encouraging that a high proportion of patients thought they learnt more about their medicines after their MURs (68 per cent) and over half of the patients in this study thought they learnt more about their medicines’ side effects. Previous research has demonstrated that GPs’ views of a useful MUR include one where the pharmacist ensures that patients understand more about their medicines.[2]
This is in line with the Department of Health’s competency framework for MURs, which recommends that pharmacists develop patients’ knowledge about their medicines.[8]
This study has also shown that more patients over the age of 65 years thought they benefited from MURs than patients under 65 years old. This is especially the case for taking medicines in the right way and at the correct time. It is possible that this can be attributed to a higher level of baseline knowledge in the under-65-years age group before the MUR. However, there are no data in this study to support this, and it remains a matter for speculation.
Only 3 per cent of the 152 MURs in this study resulted in an intervention that led to implementation of a change in patients’ prescriptions. Although this is a seemingly low percentage, MURs target a wide patient population. They will therefore benefit fewer people than a service targeting a highly selective population. Furthermore, since this study was conducted in one pharmacy, which mainly services one large GP practice, this might be a reflection on good local prescribing patterns.
The potential role for MURs to be used for promoting healthy lifestyles is demonstrated in this study. Four patients stopped smoking as a result of being signposted to a smoking cessation service from an MUR. Only 55 per cent of patients were asked about their smoking status. It might be possible that, if all patients having MURs were asked about their smoking status, this may result in a higher proportion of patients taking up the smoking cessation service.
This study is limited by being a single-centre study. It was conducted in one pharmacy in one geographical area, so caution must be exercised before generalising these results. A larger, multi-centre study with a more diverse population group is required to see if similar results are obtained. Another weakness of this study, as with all questionnaire-based studies, is the response rate. Although a response rate of 53 per cent is encouraging, a higher response rate would improve the reliability of this study. The challenge remains to design a study that measures real parameters of patient benefit. This study has measured perceived patient benefit, interventions implemented and the outcome of promoting healthy lifestyles. It is assumed that the positive outcomes of these measures are likely to benefit patients, but we cannot be sure that they translate into real benefit.
Acknowledgement
We would like to thank Dean & Smedley Family Pharmacy for enabling the study to be conducted at the Derby branch.
About the authors
Susan Youssef, MRPharmS, is a community pharmacist and senior lecturer in pharmacy practice, Shahid Hussain was 4th year pharmacy student, and David Upton, MRPharmS, is former professor of pharmacy practice and research, all at De Montfort University, Leicester.
Correspondence to: Susan Youssef, senior lecturer in pharmacy practice, Leicester School of Pharmacy, De Montfort University, The Gateway, Leicester LE1 9BH
(e-mail syoussef@dmu.ac.uk)
References
[1] Pharmaceutical Services Negotiating Committee. Advanced Services. Available at www.psnc.org.uk (accessed 1 February 2010).
[2] Wilcock M, Harding G. General practitioners’ perceptions of medicines use reviews by pharmacists. The Pharmaceutical Journal 2007;279:501–3.
[3] Foulsham R, Siabi N, Nijjer S, Dhillon S. Ready, steady pause and take stock! Time to reflect on medicine use review. The Pharmaceutical Journal 2006;276:414.
[4] NPA and PCA to support MUR evaluations. The Pharmaceutical Journal 2008;280:386.
[5] Wilcock M, Harding G. What do pharmacists think of MURs and do they change prescribed medication? The Pharmaceutical Journal 2008;281:163–7.
[6] Urban R, Rivers P, Morgan J. Perceptions of medicines use reviews — the views of community pharmacists within a West Yorkshire primary care trust. The Pharmaceutical Journal 2008;281:303–5.
[7] Lloydspharmacy MUR audit reveals customer satisfaction but pharmacists still challenged. The Pharmaceutical Journal 2006;277:628.
[8] Department of Health. Implementing the new Community Pharmacy Contractual Framework (2005). Available at www.dh.gov.uk (accessed 1 February 2010).
