Key points
- The promise of further clinical services conducted in pharmacies has long been discussed at a policy and professional level; however, management of long-term conditions such as hypertension does not routinely occur in pharmacies.
- There is strong trial evidence for the involvement of community pharmacy in the long-term management of hypertension. Systematic reviews and meta-analyses of these trials consistently demonstrate that this leads to a 6–7mmHg reduction in systolic blood pressure when compared with usual care.
- Several factors currently limit community pharmacy’s expansion into delivering and sustaining a hypertension management service, including: pharmacy infrastructure and staffing; medico-legal scope of practice; lack of integration into the patient pathway (including communication and information sharing); the policy and commissioning landscape; and community pharmacy’s current identity.
Introduction
Given the rising workload in primary care and the declining GP workforce, new models of care are needed to effectively treat and monitor long-term conditions, such as hypertension[1]
,[2],[3]
. Pharmacists can undertake a significant role in the management of hypertension, including supporting patients to improve adherence to antihypertensive drug treatment and by regularly monitoring their blood pressure (BP).
In 2005, the World Health Organization (WHO) produced a guideline proposing a community pharmacy-based hypertension model that could be adapted to any country[4]
. This consisted of three levels, where levels one and two related to prevention and early detection of hypertension, and level three related to ongoing hypertension monitoring. The goals of the model were to:
- Advise patients with hypertension on available treatment options;
- Identify potential medication-related problems and report them to a GP;
- Provide health education (e.g. lifestyle modifications) to patients with hypertension;
- Obtain and reinforce informed compliance;
- Teach patients about self-measurement of BP;
- Monitor treatment of patients with hypertension and refer those who do not achieve adequate BP control to their GP.
The model states the importance of pharmacist involvement in the follow-up of hypertensive patients, particularly between visits to the GP, to complement the role of the physician[4]
. In addition, the WHO attempted to provide guidelines for implementation, stating the following as important factors for consideration:
- Close co-operation with local GPs;
- The impact on the pharmacist’s time and other tasks;
- The provision of relevant training, checklists and necessary forms.
To date, figures related to the uptake of this model and evaluations of this programme are not available, and its uptake, ease of implementation and efficacy remains to be determined. Despite an abundance of other literature regarding the role of pharmacists in the detection and management of hypertension, no nationally commissioned hypertension service currently exists within the pharmacy contract in England[5]
.
This article aims to summarise the results of recent systematic reviews and other studies related to pharmacist involvement in hypertension. While its focus is on community pharmacy and primary care, some evidence from secondary care is also briefly presented. Evidence related to both hypertension screening programmes and management interventions are highlighted with a view of summarising the current work in this field alongside why such services have not yet translated into clinical practice in the UK. In addition to systematic reviews and primary literature about pharmacist-led hypertension services, a search of local sources (e.g. the Pharmaceutical Services Negotiating Committee [PSNC], the negotiating body for community pharmacy contractors in England, database) was also undertaken. The authors also ensured relevant papers not identified by searches were included to ensure suitable breadth and balance of the included data.
Hypertension
Persistently elevated BP, or hypertension, increases cardiovascular disease (CVD) risk
[6]
. Hypertension is associated with an increased risk of cardiovascular (e.g. myocardial infarction), cerebrovascular (e.g. stroke) and renovascular (e.g. renal damage and failure) events[7]
. The pathological mechanisms underlying these events result from the damage caused to small and large blood vessels, and result in structural and functional changes to vessel walls, impairing autoregulation of blood flow and altering capillary wall permeability[8]
,[9]
.
Epidemiological studies have shown that, regardless of previous CVD status, reductions in BP by 10mmHg (systolic) or 5mmHg (diastolic) result in a 22% (95% confidence interval [CI] 17–27%) relative risk (RR) reduction for coronary heart disease and 41% (95% CI 33–48%) RR reduction for stroke, in patients with a baseline systolic BP of more than 110mmHg and a diastolic BP higher than 70mmHg[10]
.
While both elevated systolic and diastolic BP are positively correlated with cardiovascular endpoints and renal disease, the association with systolic BP is stronger than diastolic BP in the general population[11],[12]
.
The prevalence of hypertension as the leading non-communicable disease globally, by number, has increased, affecting around a quarter of all adults, leading the WHO to describe this as a “global health crisis”[7],[13]
. The 2016 Health Survey for England examined the national prevalence of hypertension, based on BP measurements performed by nurses in 8,011 adults[14]
. The results suggested that 28% of adults in England are hypertensive and that 12% of adults have untreated hypertension[14]
. In 2018, the British Heart Foundation stated that better hypertension management could prevent 14,500 strokes and 9,710 heart attacks in England over three years, saving up to £202m and £72m, respectively[15]
.
Improvements are, therefore, needed across the current healthcare system for hypertension, from awareness and detection, to management and follow-up.
Classification and treatment targets
The 2019 guidance for hypertension from the National Institute for Health and Care Excellence (NICE), England’s health technology assessment body, iterates the BP classifications for adults without diabetes under the age of 80 years, which were originally set out in the 2011 guidance[6],
[16]
. It classifies hypertension into three stages:
- Stage one: clinic BP is >140/90mmHg and home or daytime ambulatory BP is >135/85mmHg;
- Stage two: clinic reading of 160/100mmHg or higher and subsequent daytime ambulatory or home monitoring average of 150/95mmHg or higher;
- Stage three or severe hypertension: clinic BP of 180mmHg (systolic) or 110mmHg (diastolic) or more[16]
.
Although exact BP thresholds or cut-off points are largely arbitrary, they are required for clinicians to know when to initiate and modify treatments based on predicted CVD risk[17]
.
In the 2011 NICE guidance for the management of hypertension, clinically important sub-populations, such as people with diabetes, were given lower BP targets of 140/80mmHg (or 130/80mmHg if there was evidence of previous or existing kidney, eye or cerebrovascular damage)[18]
. However, the 2019 guidance states that the evidence for lower targets in patients with type 2 diabetes mellitus (T2DM) without complications is limited and that previous recommendations were based on two small studies in people without hypertension[16]
. The updated guidance further acknowledges that evidence from large trials, such as the ‘Action to Control Cardiovascular Risk in Diabetes (ACCORD)’ study, suggests that lower BP targets (e.g. ≤120mmHg systolic) did not reduce the rate of cardiovascular events in patients with T2DM over and above the 140mmHg systolic BP threshold[19]
. Therefore, the 2019 guidance states that patients with T2DM should have BP targets in line with patients without T2DM — an important change for patient management[16]
.
The 2017 American Heart Association and the American College of Cardiology hypertension guidance redefined hypertension to lower levels compared with British and European recommendations[20]
. Stage 1 hypertension was lowered to 130–139mmHg systolic or 80–89mmHg diastolic BP, and stage 2 hypertension to ≥140mmHg systolic or ≥90mmHg diastolic BP. This redefinition of hypertension is estimated to increase the proportion of adults in the United States defined as being hypertensive by 14%, from 32% to 46%[20]
.
Although the European Society of Hypertension and European Society of Cardiology 2018 guidelines largely echo the NICE classifications, they further stratify hypertensive categories for ‘pre-hypertensive stages’[21]
. These additional classifications include ‘optimal’ (<120/80mmHg clinic), ‘normal’ (120/80–129/84mmHg clinic) and ‘high-normal’ (130/85mmHg to 139/89mmHg) BP[21]
.
The change in US guidance is underpinned by recent evidence advocating the benefits of more intensive BP lowering on cardiovascular outcomes and mortality
[22]. This evidence includes a 2016 systematic review by Ettehad et al. of large-scale BP-lowering trials (defined as a minimum of 1,000 patient-years of follow-up in each study arm) including the ‘Systolic Blood Pressure Intervention Trial (SPRINT)’ that showed strong evidence for BP lowering to systolic levels of less than 130mmHg[22]
,[23]
. The meta-analysis of more than 600,000 patients (comprised predominantly of a secondary-prevention population) showed a significant RR reduction for both major CVD events and all-cause mortality for every 10mmHg reduction in BP from a baseline systolic BP of >160mmHg, 150–159mmHg, 140–149mmHg (a non-significant reduction in all-cause mortality), 130–139mmHg and <130mmHg[23]
.
In contrast to the findings of Ettehad et al., a 2018 systematic review of mostly primary-prevention populations by Brunstrom et al. showed that while BP lowering was associated with a reduced risk for death and major cardiovascular events when systolic BP was ≥160mmHg (RR 0.93; 95% CI 0.87–1.00) and 140–159mmHg (RR 0.78; 95% CI 0.70–0.87) in trial populations with a baseline systolic BP of <140mmHg, treatment was not significantly associated with reduced mortality (RR 0.98; 95% CI 0.90–1.06) or a reduction in major cardiovascular events (RR 0.97; 95% CI 0.90–1.04)[24]
. However, it should be noted that they used a different set of trials and pooled results via a random effects meta-analysis rather than the fixed effects model used in Ettehad et al.[23]
.
The definition of elevated BP measured in a community pharmacy setting is also indistinct. Until recently, both the Royal Pharmaceutical Society (RPS), the professional leadership body for pharmacists and pharmacy in Great Britain, and the WHO suggested that the standard clinic 140/90mmHg threshold for hypertension is appropriate for interpreting pharmacy-measured BP[4],[25]
. This recommendation, however, was not based on evidence from diagnostic accuracy studies comparing this relationship. Instead, the recommendation assumes that pharmacies, as clinically related settings containing a healthcare professional, would be associated with a similar ‘white-coat’ effect on BP (i.e. where clinic readings are higher than out-of-office BP measurements) as documented during GP measurements[26]
.
More recent evidence from a systematic review has suggested that pharmacy-measured BP may be more appropriately interpreted using the out-of-office threshold of 135/85mmHg, particularly when screening undiagnosed patients[27]
. These results appear to concur with other evidence showing that BP measured by a nurse is, on average, 7mmHg lower than GP-measured BP in a clinic[28]
. Further, adequately powered, primary studies are required to conclusively assert that the white-coat effect is less pronounced in the pharmacy setting than in a GP clinic but, if confirmed, this could result in more accurate and convenient BP measuring arrangements for patients.
Screening for high blood pressure in pharmacies
Introduced in England in 2009, the NHS health check is a systematic screening programme for patients aged 40–74 years with no history of CVD[29]
. It consists of questions about lifestyle factors and family medical history, as well as measurements of clinical parameters such as height, weight, BP, cholesterol and, where appropriate, blood glucose levels[30]
. Commissioning of pharmacy NHS health checks occur locally; therefore, unlike the national coverage offered by general practices, pharmacy NHS health checks are commissioned by local authorities based on local population need[31]
. The delivery of NHS health checks in pharmacy has been advocated to improve access in hard-to-reach populations (i.e. GP non-attenders), in an attempt to reduce health inequalities from population-level screening programmes[32]
.
In a study examining data from 190 NHS health checks performed in four pharmacies, 35% of patients (n=67) were referred to either weight support services, smoking cessation, alcohol reduction or exercise schemes, with 17% of patients (n=33) accepting these referrals[31]
. Of the 33 patients referred directly to their GP after the pharmacy health check (owing to >20% predicted ten-year CVD risk or elevated BP [>140/90mmHg]), only 6% of patients (n=2) were confirmed to have attended their referral. Limited additional evidence relates to NHS health checks in community pharmacy specifically, and the evidence for the health check service is mixed, both in terms of uptake and the resulting difference in clinical outcomes between attenders and non-attenders[33],[34]
.
A systematic review by Willis et al. summarised the evidence related to screening for diabetes and CVD risk factors in pharmacies for 16 studies (n=108,414 participants, mean age 55 years), 4 of which were conducted in the UK[35]
. Meta-analysis was conducted on nine of the studies and, owing to significant heterogeneity between the studies, pooled statistics were not reported. However, rates of referral to primary care ranged from 6% to 73% (nine studies, n=99,708 referrals), and uptake of referral to the GP ranged from 13% to 92% (six studies, n=10,113 referrals). The findings show that studies of opportunistic pharmacy-based screening interventions could be successful in identifying people at high risk of CVD or T2DM. It also showed that a high proportion of individuals found to be at high risk of CVD do not attend a follow-up appointment with their GP and, therefore, suggested that future screening interventions in pharmacies are designed to increase the chances of follow-up appointments, perhaps via closer working relationships with practices. Other studies have been able to demonstrate better BP outcomes resulting from a physician–pharmacist collaborative model for hypertension care[36]
. A literature review on team-based hypertension care recommended that future work needs to determine the best populations to target with a team-based BP service and how best to implement team-based approaches in a way that utilises pharmacists working in community, general practice and hospital settings[37]
. Some of the operational factors that require addressing for this to take place are discussed later in this article.
The ‘Heart MOT’ study, a targeted, pharmacy-based, CVD risk assessment service for primary prevention, reports an evaluation of opportunistic CVD screening in 23 community pharmacies in the West Midlands[38]
. It aimed to evaluate the feasibility of delivering CVD screening in pharmacies and to assess whether high-risk and ‘disadvantaged’ patient groups could be effectively targeted[38]
. Data were reported for 1,130 patients, 33% (n=370) of whom were referred to their GP owing to elevated BP (>140/90mmHg). The study estimated that a CVD screening service would be feasible to implement in practice and could reach hard-to-reach populations (e.g. younger males, people from socio-economically deprived backgrounds and minority ethnic groups)[38]
.
A large systematic CVD screening programme delivered across 184 pharmacies in Austria (n=6,800 participants) demonstrated that pharmacists were able to detect elevated BP readings (>140/90mmHg) in 44% (n=2,992) of participants and the screening initiative was reported as being feasible to deliver[39]
. Further studies of CVD risk screening in pharmacies have replicated these findings elsewhere in the world[40]
. While healthcare systems and pharmacies across Europe and the rest of the world are different to those in the UK, these studies demonstrate that UK pharmacists could feasibly deliver services.
Screening in practice
The PSNC holds a local and national level database of commissioned services, pilot studies and other ongoing projects across community pharmacies in England[41]
. Between April 2013 and December 2018, several hypertension-related projects were entered into the database (see Table). The largest of these reported projects are in:
- Wakefield: ‘The Blood Pressure Drop In’ was a six-week pilot campaign in the Wakefield area focusing on the early detection of high BP in 2014[42]
. The campaign encouraged individuals aged over 40 years, with no pre-existing diagnosis of high BP, to have their BP measured in a pharmacy. People with high BP readings (>140/90mmHg) were encouraged to visit their GP and were offered lifestyle advice and support. Of the 3,632 patients tested, 20% were found to have high BP that was previously undiagnosed; - Northamptonshire, Bedfordshire and Milton Keynes: A pilot screening programme for hypertension and atrial fibrillation (AF) in community pharmacy[43]
. Patients aged over of 40 years received advice on reducing their future risk of CVD by addressing modifiable risk factors (e.g. excess weight, dietary salt or alcohol). The scheme offered patients with a pharmacy BP of ≥140/90mmHg home testing to confirm diagnosis of hypertension. The pilot service ran from February 2018 for three months and involved checking a patient’s pulse for patients aged over 65 years, to screen for possible AF; - Cheshire and Merseyside: A BP screening programme for adults over 18 years, aiming to take a minimum of 3,000 BP screening measurements across 120 healthy living pharmacies (HLPs) by the end of March 2019[41]
.
| Location | Service name | Description on Pharmaceutical Services Negotiating Committee database | Commissioner | Status as of December 2019 |
|---|---|---|---|---|
| Bedfordshire, Luton & Milton Keynes | Screening for hypertension and atrial fibrillation in community pharmacy | Local sustainability and transformation partnership developed a pilot service to target patients for hypertension and atrial fibrillation screening through community pharmacies | Milton Keynes Council | Completed |
| Bury | Bury find and treat hypertension and atrial fibrillation | No information provided | Bury Council | Ongoing |
| Cheshire & Merseyside | British Heart Foundation blood pressure innovation award | Healthy living pharmacies (HLPs) to offer blood pressure and pulse screening for atrial fibrillation (AF) | British Heart Foundation | Round 1 completed; round 2 ongoing |
| Derbyshire & Nottinghamshire | Community pharmacy blood pressure and atrial fibrillation drop-in project | Early detection of hypertension and AF | NHS England North Midlands | Ongoing |
| East Riding of Yorkshire & Hull | Blood pressure testing service | Increase the detection of undiagnosed high blood pressure through HLPs | NHS England Yorkshire and the Humber | Ongoing |
| Frimley | Blood pressure and atrial fibrillation screening project | Opportunistic health checks in community pharmacy, including blood pressure (BP) and pulse checks to identify hypertension and/or AF | Surrey Heath Clinical Commissioning Group (CCG) | Ongoing |
| Halton | Screening for hypertension and atrial fibrillation in community pharmacy | Patients at risk of developing hypertension to receive advice on reducing their cardiovascular disease (CVD) risk. If clinic BP >140/90mmHg, ambulatory BP monitoring will be offered from the pharmacy to confirm diagnosis of hypertension | Halton CCG | Completed |
| Kensington and Chelsea | Testing and detection of high blood pressure | No information provided | No information provided | Ongoing |
| Leeds | Leeds blood pressure wise service | Opportunistic BP screening in community pharmacies for the detection of hypertension with an emphasis on AF | Leeds City Council | Ongoing |
| Newcastle Gateshead | Let’s tackle high blood pressure | BP monitoring, healthy living advice, brief interventions and identification of hypertension using home BP monitoring | Newcastle Gateshead CCG | Ongoing |
| Thurrock | Hypertension and atrial fibrillation screening in pharmacies | Screening high-risk patients for hypertension and AF | Thurrock Council | Completed |
| Wakefield | Blood pressure drop-in pilot | Pilot intervention offering a BP, and providing appropriate information, local opportunities and products to individuals, promoting a healthier lifestyle | Leeds City Council | Completed |
To date, few, if any, published evaluations of these schemes are available beyond summary data on the numbers of patients screened. Evaluations are needed regarding the implementation of these services, any funding sources, impact on other pharmacy tasks, as well as clinical outcomes. Without these data, pilots are unlikely to develop into fully fledged services and risk repeating the same mistakes as previous small-scale pilots undertaken in other areas.
The Company Chemists’ Association (CCA) report ‘Combatting high blood pressure in the community’, published in January 2019, included a practice-based audit that sought to quantify the current contribution of community pharmacy teams in addressing high blood pressure[44]
. Data were collated from 5,220 pharmacies representing just under 40% of the pharmacy sector in England. Over the week-long audit period, pharmacies reported:
- A total of 221,091 hypertension-related contacts between pharmacy teams and patients — 74% of whom were already diagnosed with hypertension;
- A total of 131,372 contacts directly related to the patient’s medication;
- A total of 56,282 instances of provision of healthy lifestyle advice;
- A total of 30,169 BP measurements being undertaken — 20% of which recorded levels of 140/90mmHg or higher.
Furthermore, 4% (n=9,102) of the total 221,091 patients were referred to their GP for hypertension-related reasons, although the specific reasons for referral were not stated. This referral rate was in line with previous literature examining hypertension-related referrals from the new medicine service (NMS) — a service providing support for people with long-term conditions who have been newly prescribed a medicine to help improve medicines adherence — in pharmacies. Some 4.5% (n=5,895) of the 131,419 patients studied were referred back to their GP after the first two weeks of treatment, with the most common reason for this being antihypertensive medication side effects[45]
.
In terms of screening of elevated BP, around 35% of the pharmacies audited had taken part in a public health promotion related to BP within the past year, such as the ‘Know your numbers’ campaign, ‘May measurement month’, or promotions related to their HLP status[46],[47],[48]
.
Other evidence related to community pharmacy’s involvement with BP screening includes a 2016 campaign by Asda pharmacies offering home BP monitors at not-for-profit prices of around £7.50, resulting in around 94,000 sales to encourage self-monitoring[49]
.
BP kiosks (such as ‘PharmaSmart’ kiosks) are positioned in many pharmacies in North America for patients to self-test their BP[50]
. Patients are provided a receipt-like slip of paper with their results and have the option to enter other details for a CVD risk assessment. Stationary kiosks provide a less-formal way for patients to self-screen for elevated BP than traditional methods of detection, and similar ‘solid-cuff’ monitors are found in some GP surgery waiting rooms in the UK[51]
.
Hypertension management
Overall, few randomised studies have examined the effectiveness of BP screening initiatives in community pharmacies. In contrast, several trials of pharmacist-led management or co-management of hypertension exist.
Evidence for pharmacist-led management of hypertension
A systematic review of 16 randomised controlled trials (RCTs) of community pharmacist-led interventions to reduce BP were summarised in a systematic review by Cheema et al., published in 2014[52]
. The Supplementary Table provides a summary of each study and their respective interventions. Patients were recruited into the trials either via referral from their GP or from them opportunistically presenting to the pharmacy to collect their medication. Common interventions included providing face-to-face consultations with patients in the pharmacy, as well as providing feedback and results to the patient’s GP to implement any changes required. The transfer of this information to general practice occurred through letters or faxes to the practice, via the patient verbally, or through email and telephone communication with the practice. All studies required the community pharmacist to either measure BP in the pharmacy or to interpret BP readings from home or the GP clinic before making clinical recommendations; however, the threshold of ‘high’ or ‘normal’ BP varied between the studies (see Supplementary Table).
In general, the interventions delivered by pharmacists were medication-related and included:
- Establishing and improving adherence to BP medicines;
- Identification of medicine-related problems and side effects;
- Making recommendations regarding medication choices to lower BP;
- Advising on diet and lifestyle, including alcohol reduction and referral to smoking cessation schemes.
Pharmacists received up to two days’ training at the start of the trials to deliver the consultations.
In 11 of the 16 RCTs in the meta-analysis, pooled systolic BP changes in the pharmacy intervention arms were 6.1mmHg lower on average than in the usual GP care groups (95% CI –8.4 to –3.8), with ‘moderate’ statistical heterogeneity observed in the meta-analysis (I2=36%; P=0.11). In context, this level of BP lowering could equate to a 20% RR for stroke and a 10% RR for coronary heart disease[10]
. Diastolic BP was also altered by an average of –2.51mmHg (95% CI: –3.46 to –1.55), compared with usual care. This was heterogeneous and encompassed either truly usual care (GP management), or some educational or informative elements delivered to the patients.
A Cochrane review is currently assessing interventions delivered by allied health professionals, including pharmacists, to improve the control of hypertension[53],[54]
. Interim findings, pooling data from more than 40 RCTs (published up to August 2017) of pharmacist-led interventions from primary care, secondary care and community settings, suggest that pharmacist-led interventions are more effective than doctor-led usual care (see Figure 1). Overall, there was considerable heterogeneity between the studies, which employed a range of interventions; however, pooled findings showed that pharmacists deliver greater changes in both systolic (–7.2mmHg; 95% CI –5.8 to –8.7; I2=85%, 46 studies, 9,777 participants) and diastolic (–3.3mmHg; 95% CI –2.5 to –4.1; I2 = 75%, 43 studies, 9,052 participants) BP. Pharmacist-led care was also associated with a greater likelihood of achieving BP targets (odds ratio [OR] 2.7; 95% CI 2.2–3.3; I2 =69%; 36 studies, 6,747 participants) and use of antihypertensive medication (OR 1.8; 95% CI 1.3–2.5; I2 =70%; 15 studies; 3,316 participants). The pharmacist-led interventions studied appear consistently effective across primary care, secondary care and community settings, and applied to a wide range of ethnic groups. Important components of effective interventions were face-to-face delivery of care, high frequency of intervention (i.e. monthly) and the ability for the pharmacist to change medicines[54]
.
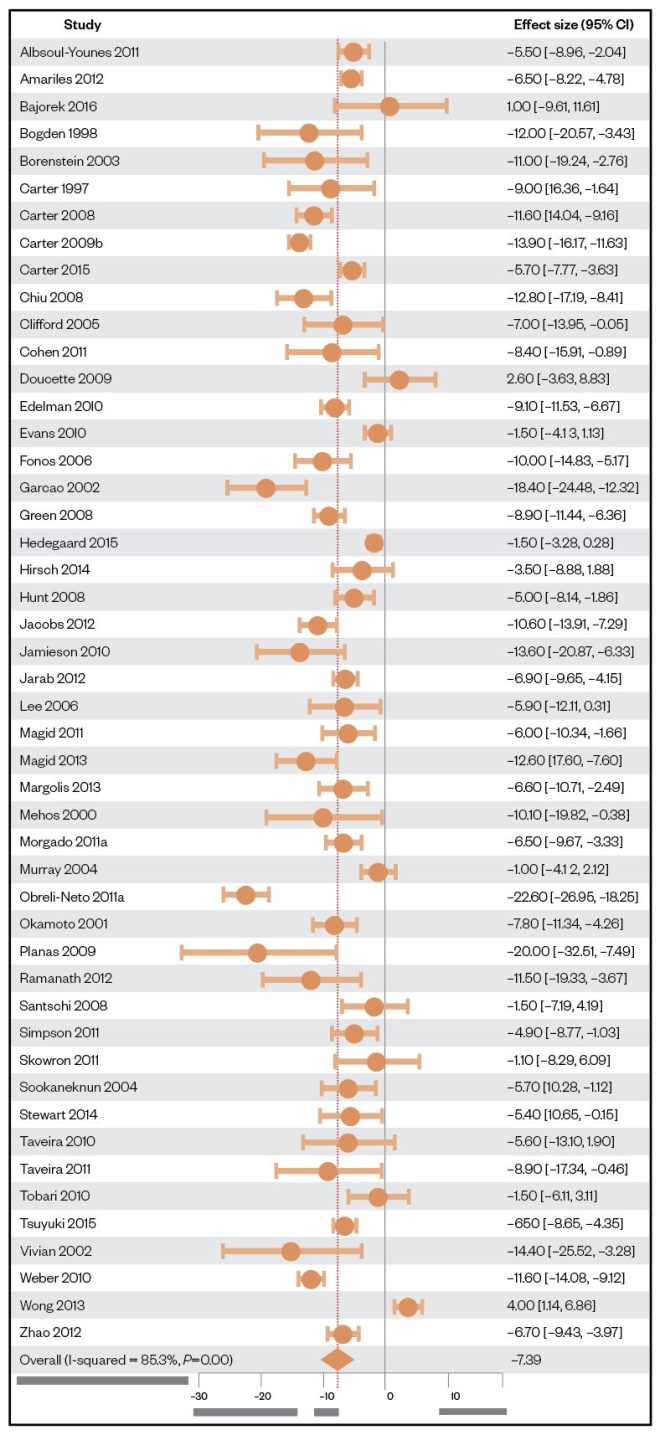
Figure 1: Comparison between systolic blood pressure change between pharmacist-led and usual care
Source: Reproduced with permission
CI: confidence interval
Sources: Am J Manag Care
[59]; JAMA
[60],[125]
,[132]
; Circ Cardiovasc Qual Outcomes
[61]
,[121]
; J Am Pharm Assoc
[102],[129]
; Pharm World Sci
[104]
, Ann Pharmacother
[107],[142]
; J Manag Care Pharm
[111]
,[131]
;Saudi Med J
[113]
; Pharm Pract
[114] ,[141]
; J Gen Intern Med
[115],[128]
; Pharmacotherapy
[116],[118],[124],[133],[135],[137],[147]
; Arch Intern Med
[117],[148]
; J Clin Hypertens
[119]
; J Clin Pharm Ther
[121],[143]
; Diabetes Care
[122],[140]
; Diabetes Educ
[123],[144]
; Am J Med
[126]
; Clin Ther
[127]
; Int J Clin Pharm
[134],[136]
; J Young Pharm
[138]
; Eur J Intern Med
[139]
; Am J Hypertens
[145]
;Circulation
[146]
; J Clin Pharmacol
[149]
; African Journal of Pharmacy and Pharmacology
[150]
Other systematic reviews corroborate these findings, indicating that pharmacist-led interventions, alone or in collaboration with other healthcare professionals, can significantly reduce both systolic and diastolic BP across various healthcare settings[55],[56]
.
Self-monitoring and telemonitoring
NICE guidance supports the use of BP self-monitoring, or home BP monitoring, for both diagnosis and ongoing monitoring of hypertension[6],[16]
. Evidence from a systematic review and individual patient-data meta-analysis by Tucker et al. included data from 25 studies (n=10,487 patients) investigating the role of self-monitoring of BP in hypertension[57]
. Their meta-analysis showed that, when conducted alone, patient self-monitoring of BP had little or no effect on BP lowering over usual GP care (systolic BP –1mmHg; 95% CI –3.3 to 1.2)[57]
. However, when self-monitoring was combined with intensive co-interventions (e.g. pharmacists providing feedback on readings, ongoing patient education and dose titration), self-monitoring led to clinically significant BP changes of –6.1mmHg (95% CI –9.0 to –3.2) over usual clinical care. The opportunity for pharmacists to encourage patient self-monitoring of BP and provide the necessary aftercare could, therefore, be developed into a workable model of ongoing hypertension management.
BP telepharmacy can broadly be defined as a strategy that allows remote data transmission of BP from a patient’s home to the pharmacy[58]
. Some four RCTs were included in a meta-analysis reviewing the evidence for the use of telepharmacy in hypertension management, and included a combined total of 1,565 patients (787 usual care and 778 pharmacist’s intervention)[59],[60],[61],[62]
. Following 6–12 months of pharmacist telemonitoring, both BP reductions and proportions of patients achieving BP targets were significantly improved compared with usual care (see Figure 2). Improvements in medication intensification were identified as the main mechanism for improved BP outcomes in all four studies; however, these benefits were reduced or abolished in the months post follow-up, highlighting the importance of the delivery of sustained interventions in pharmacies. The remote nature of the monitoring, combined with alerting clinicians to dose intensification opportunities sooner, make telepharmacy BP services appealing. Triaging the self-monitoring data via pharmacies before referring to general practice is likely to ensure that the added workload associated with interpreting the data, and taking action based on their findings, is evenly allocated in primary care.
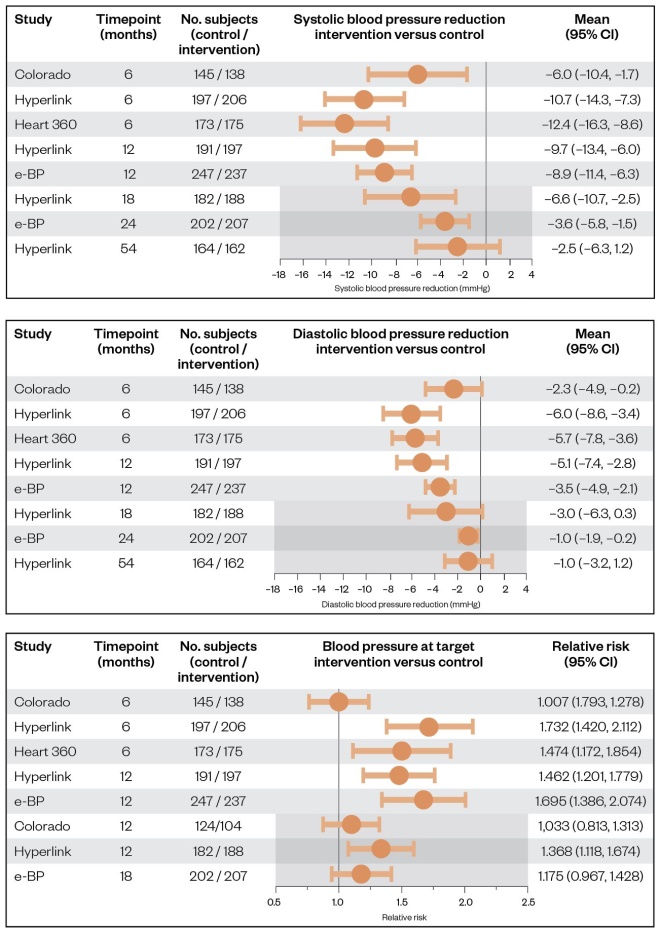
Figure 2: Mean changes from baseline between intervention and control groups for systolic boood pressure, diastolic blood pressure and relative risk
Source: Reproduced with permission
CI: Confidence interval
Source: J Hum Hypertens
[58]
With smartphone apps and wearable technologies increasingly becoming part of the evolving medical technology landscape, hypertension management is one area where future options may emerge. A 2015 review of smartphone apps for hypertension management analysed the content of the top 107 apps (by user rating) from Google Play and Apple iTunes that were available to download[63]
. The majority of apps aimed to facilitate self-management by recording and tracking BP over time, providing SMS text-message feedback on results, providing reminders to improve adherence and general education on hypertension[63]
. Around 14% of the apps utilised the phone’s camera to conduct a ‘cuffless’ BP reading; however, none of these reported any validation of their measurement technique against mercury sphygmomanometers. Nonetheless, this is an area where future developments in artificial intelligence, using pulse wave velocity, for example, could lead to cuffless BP readings and, therefore, the potential for improved self-monitoring of hypertension[64],[65]
.
The ‘Medication adherence improvement support app for engagement — blood pressure (MedISAFE-BP)’ trial — one of the few RCTs of a standalone blood pressure/adherence app — was conducted in 2018[66]
. After 12 weeks’ follow-up, 210 patients of the 412 using the app had reduced their systolic BP by an average of 10.6mmHg; however, this was not significantly different to those receiving usual care (n=202) whose BP was reduced by 10.1mmHg. The results of the trial highlight the importance of RCTs when establishing the efficacy of new interventions and technologies. Future collaborations, at the development or pre-development stage, between the medical community, biomedical engineers and user-interface experts are also likely needed to increase the chances of future apps improving patient outcomes over current practice.
Discussion
This article has summarised the current evidence related to hypertension screening and management in community pharmacies. The strongest evidence in support of pharmacist involvement relates to their role in managing hypertension, where meta-analyses have suggested that BP can be significantly reduced by up to 7mmHg over usual GP care. Despite this, there are a lack of economic analyses and ‘hard outcomes’ (e.g. CV events) that would likely aid the translation of the existing evidence from trial settings into real-world practice.
Factors influencing the implementation of pharmacist-led hypertension services in practice
While this article has shown that there is evidence of effectiveness for the involvement of pharmacists with hypertension, few, if any, commissioned services currently exist that support this role in practice. The reasons for this are multifactorial and complex. However, they require acknowledgement and discussion for a balanced debate about the prospect of extended pharmacist roles, particularly in providing hypertension care in the community, and are elaborated on below.
Pharmacy infrastructure and staffing
Providing monthly follow-up appointments for hypertension monitoring is associated with improved BP outcomes over less frequent monitoring, and this has been consistently shown in the literature of community-based, general practice-based and secondary care-based pharmacist intervention trials[54],[56],[67]
. However, the effect of diverting a pharmacist’s time from other essential pharmacy tasks has not been well estimated (if at all) in previous RCTs, making the ease of implementing more intensive interventions difficult to ascertain. In a study of how other additional services have been embedded into everyday practice (in particular, medication-use reviews [MURs]), one pharmacist exemplified this point:
“You can’t switch off from the fact that you know that’s going on (prescriptions piling up while conducting an MUR in the consultation room). And that’s in the back of your mind when you know that you’re exceptionally busy. It puts you under pressure and you really just want to get through those questions (the MUR) as quickly as possible because you know you are going to go back to bedlam. You can’t switch off from that because that’s part of your responsibility as well[68]
.”
From the pharmacist perspective, dispensing involves clinically checking the drug and dose for the patient and accuracy-checking the dispensed label and item processed by the dispenser[69]
. This labour-intensive task accounts for around 80% of a community pharmacy’s income and, therefore, is vital to the viability of a pharmacy[70]
. The steady increase in prescription volumes from around 80 million items per year in England in 2011 to more than 90 million items per year in 2015, and falling prescription item income, has cemented this dispensing role for pharmacists[71]
. A possible consequence of diverting a pharmacist away from their medicine distribution/dispensing role may be to threaten the financial viability of the community pharmacy. A pharmacist’s work is diverse and includes involvement in the business operations, people management and advice on both prescribed and over-the-counter medications to the public, all of which need to be balanced[72]
. Evaluations are therefore required to mitigate such impact — for example, by evaluating the cost/benefit implications of introducing a second pharmacist in the pharmacy. This may improve the deliverability of hypertension interventions and other clinical services, while maintaining other essential pharmacy tasks, but increases staff costs. Upskilling other pharmacy workers, such as healthcare assistants and pharmacy technicians, has also been suggested as having the potential to rebalance pharmacist workload towards more patient-facing services[73]
. Furthermore, technological innovations in the pharmacy sector, namely hub-and-spoke models of dispensing (i.e. automated off-site dispensing), have also been proposed, developed and implemented in a limited capacity[74]
. However, the evidence demonstrating their ability to free up a pharmacist’s time to conduct patient-facing clinics is limited[74]
.
Scope of practice
Medico-legal constraints in the UK mean that pharmacists are unable to adapt existing prescriptions (change doses or strengths of medicines) or initiate new prescription medicines in community pharmacies without the approval and signature of a prescriber
[75]
. Other than independent prescribing pharmacists, who are currently too few to fulfil these roles on a national bases and do not typically operate in community pharmacies, strategies such as patient group directions (PGDs) could be used to enable a pharmacist to add or titrate anti-hypertensive medications[76]
. However, PGDs can take a significant amount of time and resource to develop and implement[77]
. Patient-specific directions (i.e. for the care of a named patient rather than a group of patients who fit a broader definition) could also be used to devolve management to a pharmacist on a case-by-case basis. In both circumstances, a pre-agreed protocol for both up- and down-titrations of treatments, such as those used in patient self-management trials, could be devised between GPs, pharmacists, patients and the required approving organisations[78]
. In addition to this, the ability of a pharmacist to order or view routine blood and urine markers relevant to hypertension are also barriers to independent, long-term, hypertension follow-up that require addressing[79]
.
Other countries have found solutions to these issues that could be used as a precedent for the UK. In Canada, for example, all ten provinces permit community pharmacists to re-authorise repeat prescriptions, and six of the provinces allow pharmacists to make dosage alterations
[80]
. Furthermore, six of the ten provinces allow pharmacists to order and access laboratory monitoring (e.g. urea and electrolyte levels) required for annual angiotensin-converting enzyme-inhibitor monitoring[80]
. For context, Nova Scotia, the first province to allow pharmacists to reissue prescriptions, did so in 2005[81]
. Compared with England, where such a policy would be managed nationally rather than devolved to specific regions of the country, Canadian provincial health authorities can make changes to legislation that affect their locality only[81],[82]
. Although this can lead to inconsistencies in service provision across a country, such devolution is argued to reduce bureaucracy in some instances, speeding up the implementation of services[83]
.
Further considerations, such as adequate training on hypertension guidelines and the practical skills needed to effectively manage hypertension, must also be guaranteed for consistency of service delivery and patient care. Accredited programmes could be established that take into account education of the above, fulfilling the licensing requirements, regulatory issues, defining the scope of practice and responsibilities that a pharmacist would be expected to cover[84]
.
Integration into the patient pathway, including communication and information sharing
Improving communication between pharmacy and general practice, and access to patient clinical records in pharmacy, are also areas that require further consideration. This has been recognised by the RPS, which stated in its 2015 ‘Shaping pharmacy for the future’ document, that:
“Access to the patient health record will allow pharmacists to make more informed clinical decisions, in partnership with patients and other health and social care professionals, about the pharmaceutical care that patients receive[85]
.”
Pharmacists have stated that communication with GPs is often challenging, owing to a lack of collaboration between the professions, and previous literature has found that factors such as previous negative encounters and the high demand on both settings also contribute to poor interprofession communication[86]
. The consequences of poor communication between pharmacies and general practice risks duplicating work, as neither are up to date with the latest care given to the patient, potentially wasting resources. Poor communication has also been associated with a reduction in the ability of pharmacists to make timely clinical decisions and an increase in the number of patients who are lost to follow-up[85]
. Methods of communication between pharmacists and GPs were described in 11 out of 16 community pharmacy BP trials in the Cheema et al. systematic review[52]
. In those trials, pharmacists did not have access to the full clinical record, reflecting clinical practice in community pharmacies today[85]
. How pharmacists communicated results and recommendations to GPs ranged from written notes to the patient and letters directly sent to the practice, to periodic face-to-face meetings with the GP, phone calls or faxed letters. In England, pharmacists have access to a patient’s summary care records (SCR), which contains a full list of the patient’s prescribed medications, allergies and contact details, if the patient consents to sharing this information[87]
. However, further information, such as comorbidities, the content of previous consultations with the GP, laboratory results and secondary care letters, are not present. While pharmacists currently have read access to the SCR, they cannot write in the records after consultations with patients, potentially limiting their use in the context of assisting clinical service delivery.
To combat this shortcoming in access to clinical records, some areas of Europe have introduced fully integrated primary care records, such as in Valencia, Spain, where both GPs and pharmacists have combined their records into a shared system[88]
. These shared data have allowed for the better monitoring of patient concordance, for instance, whereby the prescriber can view whether the patient has collected their prescription in a given month[89]
. In addition, community pharmacists in Valencia are able to view the full clinical data needed to deliver clinical services, as well as make consultation entries into the record[89]
. An integrated computer system in England is likely to lead to similar benefits and could facilitate the delivery of pharmacist-led hypertension services. However, the bureaucracy and permissions required to set up and deliver such a system in the UK makes this approach unfeasible at present.
Policy and commissioning landscape
In 2016, the PSNC and Pharmacy Voice published the ‘Community pharmacy forward view’ in response to the ‘NHS five-year forward view’ that outlined pharmacy’s intention to be “the facilitator of personalised care and support for people with long-term conditions”[90]
. To achieve this, one of the NHS’s recommendations stated that patients could register with a specific pharmacy in order to facilitate continuity of care and a higher quality service for the management of long-term conditions in the future. Other reports and recommendations have been published by the RPS and the chief pharmaceutical officer in England, advocating a greater clinical role for community pharmacy
[90]
,[91]
. However, no specific plan, timeline or funding stream for implementing this vision has been outlined.
In 2016/2017, NHS England and the then Department of Health implemented a 6% drop in funding for the community pharmacy sector (£170m), followed by a further 6% cut in 2017/2018[92]
. At time of writing, this has resulted in 140 pharmacy closures, as well as reductions in service provision, such as free medication deliveries to older people by some pharmacies[93]
. The ‘NHS long-term plan’, published in January 2019, provided little detail with regard to the future of community pharmacies in providing clinical services[94]
. These factors have cumulatively meant that the status of future service development related to long-term condition management in pharmacies is unclear. It should also be noted that the number of pharmacists working in GP surgeries has expanded rapidly since the introduction of the NHS England clinical pharmacists in general practice programme in 2015, and has meant a growth in pharmacy services delivered in general practice — this appears to be favoured over clinical services delivered in pharmacies from a commissioning perspective[95]
.
Community pharmacy’s identity
A further challenge to delivering extended services in community pharmacies is the ‘commercial versus healthcare’ identity problem that the setting faces. In a survey of all primary care trusts (now clinical commissioning groups) in England, engagement with extended pharmacy services occurred disproportionately more in larger pharmacy chains than independent or small chain pharmacies; this was primarily driven by commercial and corporate pressures to achieve financial targets[96]
. Bush et al. referred to this as the ‘corporatisation’ of community pharmacy, whereby the needs of the business are put ahead of patient or wider NHS priorities[97]
. This has the potential to create a conflict between the role of pharmacists as healthcare professionals and the assumed business priorities of those who own the pharmacy chain. In the past, pharmacists have reported feeling pressurised to conduct services, such as MURs, to meet targets, and this can result in lower quality patient care and inappropriate use of resources if abused
[68]. However, the need for adequate funding is crucial for the development and sustainability of hypertension services in pharmacies, and so payment by quality (i.e. proportion of patients achieving BP targets) rather than quantity (number of BP readings taken) may help overcome this.
Conclusion and recommendations
This review of current evidence supports the involvement of community pharmacists in hypertension management and the following recommendations can be used during stakeholder management related to developing, implementing and sustaining a future hypertension management service in pharmacies:
- Practising community pharmacists should understand the evidence supporting their involvement in hypertension management;
- In the absence of national commissioning, community pharmacists and local pharmaceutical committees could use these data to engage with local GP surgeries and commissioning groups to discuss how such interventions can be developed into services at a local level.
NHS England and service commissioners should review the available evidence, particularly with regards to the improved BP outcomes. This will allow them to actively engage with pharmacists regarding how such services can be further evaluated in practice via pilot schemes, for example, and gather data regarding implementation and feasibility in local contexts. Future studies are also needed to determine the cost-effectiveness of pharmacist-led care and team-based approaches when compared with GP- or nurse-led care alone for the detection and ongoing management of hypertension.
There is also an absence of hard outcome data, so longer-term follow-up of interventions and further evaluation of intervention delivery methods are needed in determining the way forward for pharmacists to provide effective hypertension care. The wider operational, financial and legal factors also need to be taken into consideration before hypertension management services can be implemented, and crucially, maintained, in community pharmacies in the UK. Nonetheless, the currently available evidence from RCTs is vast, and strongly suggest that pharmacist-led hypertension management results in superior BP lowering than usual GP-led care. These data should not be ignored while further improvement in the evidence-base are sought.
Financial and conflict of interest disclosures
CEC has received honoraria from Medtronic and Bayer (unrelated to pharmacy and blood pressure [BP] work) and has been loaned bilateral BP monitors by Microlife and Jawon Medical for unrestricted evaluation.
SO is scientific consultant of Biotechmed, providing telemedicine services to Italian pharmacies.
RJM has received BP monitors from Omron for research purposes.
The authors have no other relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in this manuscript. No writing assistance was used in the production of this manuscript.
References
[1] Hobbs FDR, Bankhead C, Mukhtar T et al. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet 2016;387(10035):2323–2330. doi: 10.1016/S0140-6736(16)00620-6
[2] Bodenheimer T & Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood) 2010;29(5):799–805. doi: 10.1377/hlthaff.2010.0026
[3] Kringos D, Boerma W, Bourgueil Y et al. The strength of primary care in Europe: an international comparative study. Br J Gen Pract 2013;63(616):e742–750. doi: 10.3399/bjgp13X674422
[4] CINDI & EuroPharm Forum. Pharmacy-based hypertension management model: protocol and guidelines. Copenhagen: 2005. Available at: http://apps.who.int/iris/bitstream/handle/10665/107638/E85730.pdf (accessed March 2020)
[5] Department of Health and Social Care. The community pharmacy contractual framework for 2019/20 to 2023/24: supporting delivery for the NHS long term plan. 2019. Available at: https://www.gov.uk/government/publications/community-pharmacy-contractual-framework-2019-to-2024 (accessed March 2020)
[6] National Institute for Health and Care Excellence. Hypertension: management of hypertension in adults in primary care. [CG127]. 2011. Available at: https://www.nice.org.uk/guidance/cg127 (accessed March 2020)
[7] World Health Organization. Noncommunicable diseases country profiles 2014. 2014. Available at: http://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf (accessed March 2020)
[8] Kjeldsen SE, Aksnes TA, Fagard RH et al. Hypertension. In: Camm AJ, Lüscher TF & Serruys PW. The ESC Textbook of Cardiovascular Medicine. 2nd edn. Oxford: Oxford University Press; 2009. p. 437–463
[9] Johansson BB. Hypertension mechanisms causing stroke. Clin Exp Pharmacol Physiol 1999;26(7):563–565. doi: 10.1046/j.1440-1681.1999.03081.x
[10] Law MR, Morris JK & Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338:b1665. doi: 10.1136/bmj.b1665
[11] Onat A, Ceyhan K, Erer B et al. Systolic, diastolic, and pulse pressures as coronary risk factors in a population with low cholesterol levels: a prospective 10-year evaluation. Clin Cardiol 2003;26(2):91–97. doi: 10.1002/clc.4960260209
[12] Lichtenstein MJ, Shipley MJ & Rose G. Systolic and diastolic blood pressures as predictors of coronary heart disease mortality in the Whitehall study. Br Med J (Clin Res Ed) 1985;291(6490):243–245. doi: 10.1136/bmj.291.6490.243
[13] World Health Organization. A global brief on hypertension — silent killer, global public health crisis. 2013. Available at: http://apps.who.int/iris/bitstream/handle/10665/79059/WHO_DCO_WHD_2013.2_eng.pdf (accessed March 2020)
[14] NatCen Social Research. Health Survey for England 2016 Adult health trends. 2017. Available at: https://www.gov.uk/government/statistics/health-survey-for-england-2016-findings-and-trend-tables (accessed March 2020)
[15] British Heart Foundation. England’s CVD challenge. 2018. Available at: https://www.bhf.org.uk/for-professionals/healthcare-professionals/data-and-statistics/the-cvd-challenge/the-cvd-challenge-in-england (accessed March 2020)
[16] National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. NICE guideline [NG136]. 2019. Available at: https://www.nice.org.uk/guidance/ng136 (accessed March 2020)
[17] Carretero O & Oparil S. Essential hypertension. Part I: Definition and Etiology. Circulation 2000;101(3):329–335. doi: 10.1161/01.CIR.101.3.329
[18] National Institute for Health and Care Excellence. Type 2 diabetes in adults: management. NICE guideline [NG28]. NICE 2015. Available at: https://www.nice.org.uk/guidance/ng28/chapter/1-recommendations#blood-pressure-management-2 (accessed March 2020).
[19] ACCORD Study group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362(17):1575–1585. doi: 10.1056/NEJMoa1001286
[20] Whelton PK, Committee W, Carey RM et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol 2018;71(6):e127–e248. doi: 10.1016/j.jacc.2017.11.006
[21] Williams B, Mancia G, Spiering W et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339
[22] SPRINT Research Group, Wright JT Jr, Williamson JD et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2016;373(22):2103–2116. doi: 10.1056/NEJMoa1511939
[23] Ettehad D, Emdin CA, Kiran A et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016(10022);387:957–967. doi: 10.1016/S0140-6736(15)01225-8
[24] Brunström M & Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels. JAMA Intern Med 2018;178(1):28–36. doi: 10.1001/jamainternmed.2017.6015
[25] Royal Pharmaceutical Society. Monitoring Blood Pressure — a quick reference guide. London: Pharmaceutical Press; 2011
[26] Pickering TG, Gerin W & Schwartz AR. What is the white-coat effect and how should it be measured? Blood Press Monit 2002;7(6):293–300. doi: 10.1097/01.mbp.0000053044.16575.8b
[27] Albasri A, OʼSullivan JW, Roberts NW et al. A comparison of blood pressure in community pharmacies with ambulatory, home and general practitioner office readings. J Hypertens 2017;35:1919–1928. doi: 10.1097/HJH.0000000000001443
[28] Clark CE, Horvath IA, Taylor RS et al. Doctors record higher blood pressures than nurses: systematic review and meta-analysis. Br J Gen Pr 2014;64(621):e223–e232. doi: 10.3399/bjgp14X677851
[29] NHS. NHS health check. 2019. Available at: https://www.nhs.uk/conditions/nhs-health-check/ (accessed March 2020)
[30] NHS. NHS Health Checks Best practice Guidance. 2019. Available at: https://www.healthcheck.nhs.uk/commissioners-and-providers/national-guidance/ (accessed March 2020)
[31] Corlett SA & Krska J. Evaluation of NHS health checks provided by community pharmacies. J Public Health (Oxf) 2015;38:516–523. doi: 10.1093/pubmed/fdv153
[32] McNaughton RJ, Oswald NTA, Shucksmith JS et al. Making a success of providing NHS Health Checks in community pharmacies across the Tees Valley: a qualitative study. BMC Health Serv Res 2011;11:222. doi: 10.1186/1472-6963-11-222
[33] Robson J, Dostal I, Sheikh A et al. The NHS health check in England: an evaluation of the first 4 years. BMJ Open 2015;6(1):e008840. doi: 10.1136/bmjopen-2015-008840
[34] Martin A, Saunders CL, Harte E et al. Delivery and impact of the NHS health check in the first 8 years: a systematic review. Br J Gen Pract 2018;68:e449–459. doi: 10.3399/bjgp18X697649
[35] Willis A, Rivers P, Gray LJ et al. The effectiveness of screening for diabetes and cardiovascular disease risk factors in a community pharmacy setting. PLoS One 2014;9(4):e91157. doi: 10.1371/journal.pone.0091157
[36] Anderegg MD, Gums TH, Uribe L et al. Physician-pharmacist collaborative management: Narrowing the socioeconomic blood pressure gap. Hypertension 2016;68(5):1314–1320. doi: 10.1161/HYPERTENSIONAHA.116.08043
[37] Kennelty KA, Polgreen LA & Carter BL. Team-based care with pharmacists to improve blood pressure: a review of recent literature. Curr Hypertens Rep 2018;20(1):1. doi: 10.1007/s11906-018-0803-0
[38] Horgan JMP, Blenkinsopp A & McManus RJ. Evaluation of a cardiovascular disease opportunistic risk assessment pilot (‘Heart MOT’ service) in community pharmacies. J Public Health (Oxf) 2010;32(1):110–116. doi: 10.1093/pubmed/fdp092
[39] Rohla M, Haberfeld H, Sinzinger H et al. Systematic screening for cardiovascular risk at pharmacies. Open Heart 2016;3(2). doi: 10.1136/openhrt-2016-000497
[40] Pappaccogli M, Ravetto Enri L, Perlo E et al. Assessment of a non-physician screening program for hypertension and cardiovascular risk in community pharmacies. Nutr Metab Cardiovasc Dis 2019;29(12): 1316–1322. doi: 10.1016/j.numecd.2019.07.009
[41] Pharmaceutical Services Negotiating Committee. PSNC services database. 2020. Available at: https://psnc.org.uk/services-commissioning/services-database/ (accessed March 2020)
[42] Buchan R. The blood pressure drop in. 2014. Available at: http://www.cpwy.org/doc/508.pdf (accessed March 2020)
[43] Northamptonshire and Milton Keynes LPC. Screening for hypertension and atrial fibrillation in community pharmacy and providing signposting to appropriate lifestyle advice. 2018. Available at: http://psnc.org.uk/northamptonshire-and-milton-keynes-lpc/detection-of-hypertension-and-atrial-fibrillation-in-community-pharmacies-pilot/ (accessed March 2020)
[44] Company Chemists’ Association. Combating high blood pressure in the community - Practice-based Audit Report 2017–18. London: 2019. Available at: https://thecca.org.uk/wp-content/uploads/2019/02/Combatting-high-blood-pressure-in-the-community-Jan-2019.pdf (accessed March 2020)
[45] Albasri A, Prinjha S, McManus RJ et al. Hypertension referrals from community pharmacy to general practice: multivariate logistic regression analysis of 131,419 patients. Br J Gen Pract 2018;68(673):e541–e550. doi: 10.3399/bjgp18x697925
[46] Blood Pressure UK. ‘Know your Numbers!’ blood pressure testing campaign. 2008. Available at: http://www.bloodpressureuk.org/HealthProfessionals/KnowyourNumbersWeek (accessed March 2020)
[47] Poulter NR, Schutte AE, Tomaszewski M et al. May measurement month: a new joint global initiative by the International Society of Hypertension and the World Hypertension League to raise awareness of raised blood pressure. J Hypertens 2017;35(5):1126–1128. doi: 10.1097/hjh.0000000000001346
[48] Public Health England. Healthy living pharmacy level 1 quality criteria. 2016. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/743128/HLP-quality-criteria-and-self-assessement-process.pdf (accessed March 2020)
[49] Pharmacy Voice. Tackling high blood pressure through community pharmacy. 2017. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/693902/PV_Blood_Pressure_Report.pdf (accessed March 2020)
[50] Padwal RS, Townsend RR, Trudeau L et al. Comparison of an in-pharmacy automated blood pressure kiosk to daytime ambulatory blood pressure in hypertensive subjects. J Am Soc Hypertens 2015;9(2):123–129. doi: 10.1016/j.jash.2014.11.004
[51] Tompson AC, Schwartz CL, Fleming S et al. Patient experience of home and waiting room blood pressure measurement: a qualitative study of patients with recently diagnosed hypertension. Br J Gen Pract 2018;68(677):e835–843. doi: 10.3399/bjgp18X699761
[52] Cheema E, Sutcliffe P & Singer DR. The impact of interventions by pharmacists in community pharmacies on control of hypertension: a systematic review and meta-analysis of randomized controlled trials. Br J Clin Pharmacol 2014;78(6):1238–1247. doi: 10.1111/bcp.12452
[53] Clark CE, Smith LF, Glynn LG et al. Allied health professional-led interventions for improving control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2011;11:CD009410. doi: 10.1002/14651858.CD009410
[54] Clark C, Smith L, Cloutier L et al. Interventions to improve control of hypertension; what works (and what doesn’t): systematic review and meta-regression. Can J Cardiol 2018;34(10 Suppl 1):S130–S131. doi:10.1016/j.cjca.2018.07.211
[55] Tan ECK, Stewart K, Elliott RA et al. Pharmacist services provided in general practice clinics: a systematic review and meta-analysis. Res Soc Adm Pharm 2014;10(4):608–622. doi: 10.1016/j.sapharm.2013.08.006
[56] Santschi V, Chiolero A, Colosimo AL et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc 2014;3(2):e000718. doi: 10.1161/JAHA.113.000718
[57] Tucker KL, Sheppard JP, Stevens R et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med 2017;14(9):e1002389. doi: 10.1371/journal.pmed.1002389
[58] Omboni S, Tenti M & Coronetti C. Physician–pharmacist collaborative practice and telehealth may transform hypertension management. J Hum Hypertens 2019;33(3):177–187. doi: 10.1038/s41371-018-0147-x
[59] Magid DJ, Ho PM, Olson KL et al. A multimodal blood pressure control intervention in 3 healthcare systems. Am J Manag Care 2011;17:e96–103. PMID: 21774100
[60] Margolis KL, Asche SE, Bergdall AR et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control. JAMA 2013;310(1):46–56. doi: 10.1001/jama.2013.6549
[61] Magid DJ, Olson KL, Billups SJ et al. A pharmacist-led, American Heart Association Heart360 web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes 2013;6:157–163. doi: 10.1161/CIRCOUTCOMES.112.968172
[62] Green BB, Ralston JD, Fishman PA et al. Electronic communications and home blood pressure monitoring (e-BP) study: design, delivery, and evaluation framework. Contemp Clin Trials 2008;29:376–395. doi: 10.1016/J.CCT.2007.09.005
[63] Kumar N, Khunger M, Gupta A & Garg N. A content analysis of smartphone-based applications for hypertension management. J Am Soc Hypertens 2015;9(2):130–136. doi: 10.1016/j.jash.2014.12.001
[64] Puke S, Suzuki T, Nakayama K et al. Blood pressure estimation from pulse wave velocity measured on the chest. Conf Proc IEEE Eng Med Biol Soc 2013;6107–6110. doi: 10.1109/EMBC.2013.6610946
[65] Gribbin B, Steptoe A & Sleight P. Pulse wave velocity as a measure of blood pressure change. Psychophysiology 1976;13(1):86–90. doi: 10.1111/j.1469-8986.1976.tb03344.x
[66] Morawski K, Ghazinouri R, Krumme A et al. Association of a smartphone application with medication adherence and blood pressure control: the MedISAFE-BP randomized clinical trial. JAMA Intern Med 2018;178(6):802–809. doi: 10.1001/jamainternmed.2018.0447
[67] Zillich AJ, Sutherland JM, Kumbera PA & Carter BL. Hypertension outcomes through blood pressure monitoring and evaluation by pharmacists (HOME study). J Gen Intern Med 2005;20(12):1091–1096. doi: 10.1111/j.1525-1497.2005.0226.x
[68] Latif A, Pollock K & Boardman HF. The contribution of the medicines use review (MUR) consultation to counseling practice in community pharmacies. Patient Educ Couns 2011;83(3):336–344. doi: 10.1016/J.PEC.2011.05.007
[69] Royal Pharmaceutical Society. Clinical checks: quick reference guide. 2017. Available at: https://www.rpharms.com/resources/quick-reference-guides/clinical-checks (accessed March 2020)
[70] NHS Digital. General Pharmaceutical Services in England - 2007/8 - 2016/7. 2007. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/general-pharmaceutical-services/general-pharmaceutical-services-england-2007-08-to-2016-17 (accessed March 2020)
[71] NHS Business and Services Authority. Prescription volume and prescription cost. 2015. Available at: https://www.nhsbsa.nhs.uk/prescription-data/prescribing-data/prescription-volume-and-prescription-cost (accessed March 2020)
[72] West R & Isom M. Management of patients with hypertension: general practice and community pharmacy working together. Br J Gen Pract 2014;64(626):477–478. doi: 10.3399/bjgp14X681553
[73] Braund R, Chesney KM, Keast EP et al. Are all pharmacy staff interested in potential future roles? Int J Pharm Pract 2012;20(6):417–421. doi: 10.1111/j.2042-7174.2012.00216.x
[74] Elvidge S. Automated hub-and-spoke dispensing: technology set to transform the business model of community pharmacy. Pharm J 2016;296(7888):205–208. doi: 10.1211/PJ.2016.20200976
[75] UK government. Medicines Act 1968: chapter 67. 1968. http://www.legislation.gov.uk/ukpga/1968/67/pdfs/ukpga_19680067_en.pdf (accessed March 2020)
[76] Robinson J. The trials and triumphs of pharmacist independent prescribers. Pharm J 2018;300(7911):149–152. doi: 10.1211/PJ.2018.20204489
[77] Medicines and Healthcare products Regulatory Agency. Patient group directions: who can use them. 2017. Available at: https://www.gov.uk/government/publications/patient-group-directions-pgds/patient-group-directions-who-can-use-them (accessed March 2020)
[78] McManus RJ, Mant J, Haque MS et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA 2014;312(8):799–808. doi: 10.1001/jama.2014.10057
[79] Clark CE & Sims L. Hypertension care: sharing the burden with pharmacists. Br J Gen Pract 2018;68(675):458–459. doi: 10.3399/bjgp18X698573
[80] Bhatia S, Simpson SH & Bungard T. Provincial comparison of pharmacist prescribing in Canada using Alberta’s model as the reference point. Can J Hosp Pharm 2017;70(5):349–357. doi: 10.4212/cjhp.v70i5.1696
[81] Law MR, Ma T, Fisher J et al. Independent pharmacist prescribing in Canada. Can Pharm J (Ott) 2012;145(1):17–23.e1. doi: 10.3821/1913-701X-145.1.17
[82] NHS England. Pharmacy. 2019. Available at: https://www.england.nhs.uk/commissioning/primary-care/pharmacy (accessed March 2020).
[83] NHS England. Devolution. 2015. Available at: https://www.england.nhs.uk/commissioning/devolution (accessed March 2020)
[84] Dunn SP, Birtcher KK, Beavers CJ et al. The role of the clinical pharmacist in the care of patients with cardiovascular disease. J Am Coll Cardiol 2015;66(19):2129–2139. doi: 10.1016/J.JACC.2015.09.025
[85] Royal Pharmaceutical Society. Shaping pharmacy for the future: pharmacist access to the patient health record. 2015. Available at: http://www.rpharms.com (accessed March 2020)
[86] Kelly D V, Bishop L, Young S et al. Pharmacist and physician views on collaborative practice: findings from the community pharmaceutical care project. Can Pharm J (Ott) 2013;146(4):218–226. doi: 10.1177/1715163513492642
[87] NHS Digital. Summary care records. 2020. Available at: https://digital.nhs.uk/summary-care-records (accessed March 2020)
[88] De Rosa Torner A. The King’s Fund international integrated care summit — lessons from Spain: the Alzira model. 2012. Available at: https://www.kingsfund.org.uk/sites/default/files/alberto-roso-torner-integrated-care-spain-alzira-model-kings-fund-may12.pdf (accessed March 2020)
[89] Redon J, Orozco D, Navarro J et al. Impact on mortality of the gap in the use of cardiovascular preventing drugs in diabetes: a population study. J Hypertens 2018;36:e10. doi: 10.1097/01.hjh.0000538988.02599.7e
[90] Royal Pharmaceutical Society. Frontline pharmacists: making a difference for people with long term conditions. 2016. Available at: https://www.rpharms.com/resources/reports/making-a-difference-for-people-with-ltcs (accessed March 2020)
[91] Murray R. Community pharmacy clinical services review. 2016. Available at: https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2016/12/community-pharm-clncl-serv-rev.pdf (accessed March 2020)
[92] Cavendish W & Ridge K. Community pharmacy in 2016/17 and beyond. 2015. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/486941/letter-psnc.pdf (accessed March 2020)
[93] Finch I. Department of Health ‘closely monitoring’ pharmacy closures in light of funding cuts. Chemist and Druggist 2018. Available at: https://www.chemistanddruggist.co.uk/news/dh-closely-monitors-pharmacy-closures-light-funding-cuts (accessed March 2020)
[94] NHS. NHS long term plan. 2019. Available at: www.longtermplan.nhs.uk (accessed March 2020)
[95] NHS England. Clinical Pharmacists in General Practice Pilot. 2015. Available at: https://www.england.nhs.uk/commissioning/primary-care-comm/gp-workforce/cp-gp-pilot/ (accessed March 2020)
[96] Bradley F, Wagner AC, Elvey R et al. Determinants of the uptake of medicines use reviews (MURs) by community pharmacies in England: a multi-method study. Health Policy 2008;88(2–3):258–268. doi: 10.1016/j.healthpol.2008.03.013
[97] Bush J, Langley CA & Wilson KA. The corporatization of community pharmacy: implications for service provision, the public health function, and pharmacy’s claims to professional status in the United Kingdom. Res Soc Adm Pharm 2009;5(4):305–318. doi: 10.1016/j.sapharm.2009.01.003
[98 ] Mc Kenney JM, Slining JM, Henderson HR et al. The effect of clinical pharmacy services on patients with essential hypertension. Circulation 1973;48(5):1104–1111. doi:10.1161/01.CIR.48.5.1104
[99] McKenney JM, Brown E & Necsary R. Effect of pharmacist drug monitoring and patient education on hypertensive patients. Contemp Pharm Pract 1978;1:50–56
[100] Park JJ, Kelly P, Carter BL & Burgess PP. Comprehensive pharmaceutical care in the chain setting. J Am Pharm Assoc 1996;36(7):443–451. doi: 10.1016/s1086-5802(16)30099-7
[101] Blenkinsopp A, Phelan M, Bourne J et al. Extended adherence support by community pharmacists for patients with hypertension: A randomised controlled trial. Int J Pharm Pract, 2000;8(3):165–175. doi: 10.1111/j.2042-7174.2000.tb01002.x
[102] Garção JA & Cabrita J. Evaluation of a pharmaceutical care program for hypertensive patients in rural Portugal. J Am Pharm Assoc 2002;42(6):858–864. doi: 10.1331/108658002762063691
[103] Sookaneknun P, Richards RME & Teerasut C. Pharmacist involvement in primary care improves hypertensive patient clinical outcomes. Ann Pharmacother 2004;38:2023–2028. doi: 10.1345/aph.1D605
[104] Fornos JA, Andrés NF, Andrés JC et al. A pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in Spain. Pharm World Sci 2006;28(2):65–72. doi: 10.1007/s11096-006-9003-0
[105] Krass I, Armour CL, Mitchell B et al. The Pharmacy Diabetes Care Program: assessment of a community pharmacy diabetes service model in Australia. Diabetic Medicine 2007;24(6):677–683. doi: 10.1111/j.1464-5491.2007.02143.x
[106] McLean DL, McAlister FA, Johnson JA et al. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: study of cardiovascular risk intervention by pharmacists-hypertension (SCRIP-HTN). Arch Intern Med 2008;168(21):2355–2361. doi: 10.1001/archinte.168.21.2355
[107] Doucette WR, Witry MJ, Farris KB & McDonough RP. Community pharmacist-provided extended diabetes care. Ann Pharmacother 2009;43(5):882–889. doi: 10.1345/aph.1L605
[108] Planas LG, Crosby KM, Mitchell KD et al. Evaluation of a hypertension medication therapy management program in patients with diabetes. J Am Pharm Assoc 2009;49(2):164–170. doi: 10.1331/JAPhA.2009.08164
[109] Santschi V, Lord A, Berbiche D et al. Impact of collaborative and multidisciplinary care on management of hypertension in chronic kidney disease outpatients. Journal of Pharmaceutical Health Services Research 2011;2(2):79–87. doi: 10.1111/j.1759-8893.2011.00038.x
[110] Ali M, Schifano F, Robinson P et al. Impact of community pharmacy diabetes monitoring and education programme on diabetes management: a randomized controlled study. Diabet Med 2012;29(9):e326–e333. doi: 10.1111/j.1464-5491.2012.03725.x
[111] Amariles P, Sabater-Hernández D, GarcÃa-Jiménez E et al. Effectiveness of dader method for pharmaceutical care on control of blood pressure and total cholesterol in outpatients with cardiovascular disease or cardiovascular risk: EMDADER-CV randomized controlled trial. J Manag Care Pharm 2012;18(4):311–323. doi: 10.18553/jmcp.2012.18.4.311
[112] Svarstad BL, Kotchen JM, Shireman TI et al. Improving refill adherence and hypertension control in black patients: Wisconsin TEAM trial. J Am Pharm Assoc 2013;53(5):520–529. doi:10.1331/JAPhA.2013.12246.
[113] Albsoul-Younes AM, Hammad EA, Yasein NA & Tahaineh LM. Pharmacist-physician collaboration improves blood pressure control. Saudi Med J 2011;32(3): 288–292. PMID: 21384066
[114] Bajorek B, Lemay KS, Magin P et al. Implementation and evaluation of a pharmacist-led hypertension management service in primary care: Outcomes and methodological challenges. Pharm Pract 2016;14(2):723. doi: 10.18549/PharmPract.2016.02.723
[115] Bogden PE, Abbott RD, Williamson P et al. Comparing standard care with a physician and pharmacist team approach for uncontrolled hypertension. J Gen Intern Med, 1998;13(11):740–745. doi: 10.1046/j.1525-1497.1998.00225.x
[116] Borenstein JE, Graber G, Saltiel E et al. Physician-pharmacist comanagement of hypertension: A randomized, comparative trial. Pharmacotherapy 2003;23(2):209–216. doi: 10.1592/phco.23.2.209.32096
[117] Carter BL, Ardery G, Dawson JD et al. Physician and pharmacist collaboration to improve blood pressure control. Arch Intern Med 2009;169(21):1996–2002. doi: 10.1001/archinternmed.2009.358
[118] Carter BL, Barnette DJ, Chrischilles E et al. Evaluation of hypertensive patients after care provided by community pharmacists in a rural setting. Pharmacotherapy 1997;17(6):1274–1285. PMID: 9399611
[119] Carter BL, Bergus GR, Dawson JD et al. A cluster randomized trial to evaluate physician/pharmacist collaboration to improve blood pressure control. J Clin Hypertens 2008;10(4):260–271. doi: 10.1111/j.1751-7176.2008.07434.x
[120] Carter BL, Coffey CS, Ardery G et al. Cluster-randomized trial of a physician/pharmacist collaborative model to improve blood pressure control. Circ Cardiovasc Qual Outcomes 2015;8(3):235–243. doi: 10.1161/CIRCOUTCOMES.114.001283
[121] Chiu CC, Wu SS, Lee PY et al. Control of modifiable risk factors in ischemic stroke outpatients by pharmacist intervention: an equal allocation stratified randomized study. J Clin Pharm Ther 2008;33(5):529–535. doi: 10.1111/j.1365-2710.2008.00940.x
[122] Clifford RM, Davis WA, Batty KT et al. Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the Fremantle diabetes study. Diabetes Care 2005;28(4):771–776. doi: 10.2337/diacare.28.4.771
[123] Cohen LB, Taveira TH, Khatana SA et al. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ 2011;37(6):801–812. doi: 10.1177/0145721711423980
[124] Evans CD, Eurich DT, Taylor JG & Blackburn DF. The collaborative cardiovascular risk reduction in primary care (CCARP) study. Pharmacotherapy 2010;30(8):766–775. doi: 10.1592/phco.30.8.766
[125] Green BB, Cook AJ, Ralston JD et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA 2008;299(24):2857–2867. doi: 10.1001/jama.299.24.2857
[126] Hedegaard U, Kjeldsen LJ, PottegÃ¥rd A et al. Improving medication adherence in patients with hypertension: a randomized trial. Am J Med, 2015;128(12):1351–1361. doi: 10.1016/j.amjmed.2015.08.011
[127] Hirsch JD, Steers N, Adler DS et al. Primary care-based, pharmacist-physician collaborative medication-therapy management of hypertension: a randomized, pragmatic trial. Clin Ther 2014;36(9):1244–1254. doi: 10.1016/j.clinthera.2014.06.030
[128] Hunt JS, Siemienczuk J, Pape G et al. A randomized controlled trial of team-based care: impact of physician-pharmacist collaboration on uncontrolled hypertension. J Gen Intern Med 2008;23(12):1966–1972. doi: 10.1007/s11606-008-0791-x
[129] Jacobs M, Sherry PS, Taylor LM et al. Pharmacist assisted medication program enhancing the regulation of diabetes (PAMPERED) study. J Am Pharm Assoc 2012;52(5):613–621. doi: 10.1331/JAPhA.2012.10183
[130] Jamieson LH, Scally AJ & Chrystyn H. A randomised comparison of practice pharmacist-managed hypertension providing Level 3 Medication Review versus usual care in general practice. Journal of Applied Therapeutic Research 2010;7(3):77–86
[131] Jarab AS, Alqudah SG, Mukattash TL et al. Randomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J Manag Care Pharm 2012;18(7):516–526. doi: 10.18553/jmcp.2012.18.7.516
[132] Lee JK, Grace KA & Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA 2006;296(21):2563–2571. doi: 10.1001/jama.296.21.joc60162
[133] Mehos BM, Saseen JJ & MacLaughlin EJ. Effect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertension. Pharmacotherapy 2000;20(11):1384–1389. doi: 10.1592/phco.20.17.1384.34891
[134] Morgado M, Rolo S & Castelo-Branco M. Pharmacist intervention program to enhance hypertension control: a randomised controlled trial. Int J Clin Pharm 2011;33(1):132–140. doi: 10.1007/s11096-010-9474-x
[135] Murray MD, Harris LE, Overhage JM et al. Failure of computerized treatment suggestions to improve health outcomes of outpatients with uncomplicated hypertension: results of a randomized controlled trial. Pharmacotherapy 2004;24(3):324–337. doi: 10.1592/phco.24.4.324.33173
[136] Obreli-Neto PR, Guidoni CM, De Oliveira Baldoni A et al. Effect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patients. Int J Clin Pharm 2011;33(4):642–649. doi: 10.1007/s11096-011-9518-x
[137] Okamoto MP & Nakahiro RK. Pharmacoeconomic evaluation of a pharmacist-managed hypertension clinic. Pharmacotherapy 2001;21(11):1337–1344. doi: 10.1592/phco.21.17.1337.34424
[138] Ramanath KV, Balaji DBSS, Nagakishore CH et al. A study on impact of clinical pharmacist interventions on medication adherence and quality of life in rural hypertensive patients. J Young Pharm 2012;4(2):95–100. doi: 10.4103/0975-1483.96623
[139] Santschi V, Rodondi N, Bugnon O & Burnier M. Impact of electronic monitoring of drug adherence on blood pressure control in primary care: A cluster 12-month randomised controlled study. Eur J Intern Med 2008;19(6):427–434. doi: 10.1016/j.ejim.2007.12.007
[140] Simpson SH, Majumdar SR, Tsuyuki RT et al. Effect of adding pharmacists to primary care teams on blood pressure control in patients with type 2 diabetes: a randomized controlled trial. Diabetes Care 2011;34(1):20–26. doi: 10.2337/dc10-1294
[141] Skowron A, Polak S & Brandys J. The impact of pharmaceutical care on patients with hypertension and their pharmacists. Pharm Pract 2011;9(2):110–115. doi: 10.4321/s1886-36552011000200009
[142] Sookaneknun P, Richards RM, Sanguansermsri J et al. Pharmacist Involvement in primary care improves hypertensive patient clinical outcomes hypertension. Ann Pharmacother 2004;38(12):2023–2028. doi: 10.1345/aph.1D605
[143] Stewart K, George J, Mc Namara KP et al. A multifaceted pharmacist intervention to improve antihypertensive adherence: A cluster-randomized, controlled trial (HAPPy trial). J Clin Pharm Ther 2014;39(5):527–534. doi: 10.1111/jcpt.12185
[144] Taveira TH, Friedmann PD, Cohen LB et al. Pharmacist-led group medical appointment model in type 2 diabetes. Diabetes Educ 2010;36(1):109–117. doi: 10.1177/0145721709352383
[145] Tobari H, Arimoto T, Shimojo N et al. Physician-pharmacist cooperation program for blood pressure control in patients with hypertension: A randomized-controlled trial. Am J Hypertens 2010;23(10):1144–1152. doi: 10.1038/ajh.2010.127
[146] Tsuyuki R, Houle SK, Charrois TL et al. Randomized trial of the effect of pharmacist prescribing on improving blood pressure in the community: the Alberta clinical trial in optimizing hypertension (RxACTION). Circulation 2015;132(2):93-100. doi: 10.1161/CIRCULATIONAHA.115.015464
[147] Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy 2002;22(12):1533–1540. doi: 10.1592/phco.22.17.1533.34127
[148] Weber CA, Ernst ME, Sezate GS et al. Pharmacist-physician comanagement of hypertension and reduction in 24-hour ambulatory blood pressures. Arch Intern Med 2010;170(18):1634–1639. doi: 10.1001/archinternmed.2010.349
[149] Wong MCS, Liu KQL, Wang HHX et al. Effectiveness of a pharmacist-led drug counseling on enhancing antihypertensive adherence and blood pressure control: A randomized controlled trial. J Clin Pharmacol 2013;53(7):753–761. doi: 10.1002/jcph.101
[150] Zhao PX, Wang C, Qin L et al. Effect of clinical pharmacist’s pharmaceutical care intervention to control hypertensive outpatients in China. African Journal of Pharmacy and Pharmacology 2012;6(1):48–56. doi: 10.5897/AJPP11.633


