Abstract
Aim
To evaluate patients’ experience of our established pharmacist-led supplementary prescribing hypertension clinic.
Design
A closed question, self-administered postal questionnaire.
Subjects and settings
Patients invited to attend a pharmacist-led supplementary prescribing hypertension clinic at Derwent Valley Medical Practice, Derby.
Outcome measures
Respondent’s views.
Results
83% of respondents attended the first clinic appointment. Of these, 91% continue to attend, 8% no longer attend and 1% decided against participating in the clinic. The reasons given for not attending or not continuing to attend the clinic were inconvenient appointment times, development of a new condition, prefer to continue with GP/ nurse led care, rather not see a pharmacist, invitation to attend not received and no longer registered with the surgery. 57% of respondents stated that the standard of care they received in clinic was better than they received previously. 86% stated that they understand more about their condition since attending clinic. 86% stated that they feel more involved in making decisions regarding their treatment since attending clinic. 86% stated that they could make an appointment for review easily. 92% stated that supplementary prescribing by pharmacists was a good idea.
Conclusions
Most patients were happy to attend our pharmacist-led supplementary prescribing hypertension clinic. These patients generally thought the standard of care was better and that their understanding about their condition and involvement in treatment decisions had improved since attending clinic. Overall patients stated that supplementary prescribing by pharmacists is a good idea.
In November 2002, the Department of Health announced that pharmacists would become eligible to train as supplementary prescribers1 and, in February 2004, the first pharmacist supplementary prescribers were registered with the Royal Pharmaceutical Society.2
The fundamental aim of supplementary prescribing is to provide patients with quicker and more efficient access to medicines and to make the best use of the skills of trained nurses and pharmacists.3
As with any new way of working, the evidence base regarding the success of supplementary prescribing is in its infancy. A study of patients attending a rheumatology supplementary prescribing outpatient clinic showed that patients are happy to be seen and have their medicines prescribed by a pharmacist,4 and the current work being undertaken at Sheffield and Bath universities will provide further information regarding patients’, pharmacists’ and doctors’ experiences of pharmacist supplementary prescribing.5,6
We have been operating our pharmacist supplementary prescribing hypertension clinic since May 2004, the structure of which has been described previously.7 The success of a pharmacist-led hypertension clinic has been reported previously.8,9 In this paper I explore quantitative evidence relating to our patients’ experience of supplementary prescribing in primary care. The practice will use this information to develop our service.
My aim was to evaluate patients’ experience of our established pharmacist-led supplementary prescribing hypertension clinic. Specific objectives were to determine why patients choose not to participate in the clinic and to investigate their perception of the benefits of supplementary prescribing.
Method
Anecdotal evidence from the first year of our clinic indicated patients were happy to participate and could identify benefits over other traditional models of health care. I designed a quantitative study to determine how widely this positive patient response was held by clinic participants. A quantitative method was chosen as it would allow me to ask a few key questions to all patients who had been invited to participate in the clinic, rather than exploring the views of a smaller group using qualitative methods. The primary purpose of the study was to identify general attitudes to the clinic that would allow me to ascertain how successful it had been and to identify whether any changes were needed. Further qualitative research could be used to explore any issues arising from the quantitative method in more detail.
A self-administered postal questionnaire was developed. The questions were designed to elicit the reasons for patients’ participation, and their perception of the benefits of attending the clinic. This method was chosen as it is a cost-effective method of collecting standardised data. In addition, postal surveys reduce interview bias compared with interviewer-administered questionnaires.10
Closed, multi-response questions were used because these provide responses that are relatively simple to analyse. However, the major limitation of this method is that predetermined responses may force respondents into selecting a response that is not entirely accurate.10 For this reason, an “other” category was included in each set of responses. The use of open questions can further reduce this bias, but this method is not suited to self-administered questionnaires because many respondents may not reply to open questions.10 The questionnaire was piloted on a small group of peers as a result of which minor amendments were made in order to aid patient comprehension.
A computer search was used to identify all patients with an appointment at our clinic between May 2004 and June 2005. This identified 127 patients who had been asked to participate in the clinic, either via letter or direct referral from another member of our clinical team, and included patients who had not attended the appointment. All patients were sent a questionnaire, together with a covering letter and a stamped addressed envelope to enhance the return rate. All questionnaires contained a serial number. This allowed identification of those patients who had not replied by the requested date. These patients were sent a further copy of the questionnaire with covering letter.
Aim
This study was primarily undertaken to explore patients’ attitudes and develop our clinic. I did not undertake statistical analysis as this would not have altered our application of the results. I acknowledge that this is a small study with a simple design.
Approvals
Research and development approval was sought and was granted. I contacted the Central Office for Research Ethics Committees regarding ethical approval and was informed that it was not required.
Results
The response rate at the reply date was 73 per cent (93/127) and this was increased to 87 per cent (111/127) following the second set of questionnaires.
During initial analysis, the returned questionnaires were reconciled against the EMIS computer records using serial numbers. Four respondents were found to have misinterpreted the questionnaire and were excluded from the analysis. The remaining 107 (84 per cent) were analysed as below.
When invited to attend the clinic, 18 respondents (17 per cent) chose not to attend the first appointment. Of these, 17 gave reasons, which were:
- Inconvenient appointment time (six respondents)
- Preference to continue with GP or nurse care (five respondents)
- Inconvenient appointment time and preference to continue with GP or nurse care (two respondents)
- Would rather not see a pharmacist (two respondents)
- Did not receive invitation to attend (one respondent)
Eighty-nine respondents (83 per cent) attended the first clinic appointment. Of these, 91 per cent continue to attend, 8 per cent no longer attend and 1 per cent decided against participating in the clinic. Seven respondents gave reasons for not continuing to attend the clinic:
- Development of a new condition (three respondents)
- Preference to continue with GP or nurse care (two respondents)
- Development of a new condition and a preference to continue with GP or nurse care (one respondent)
- Moved out of area (one respondent)
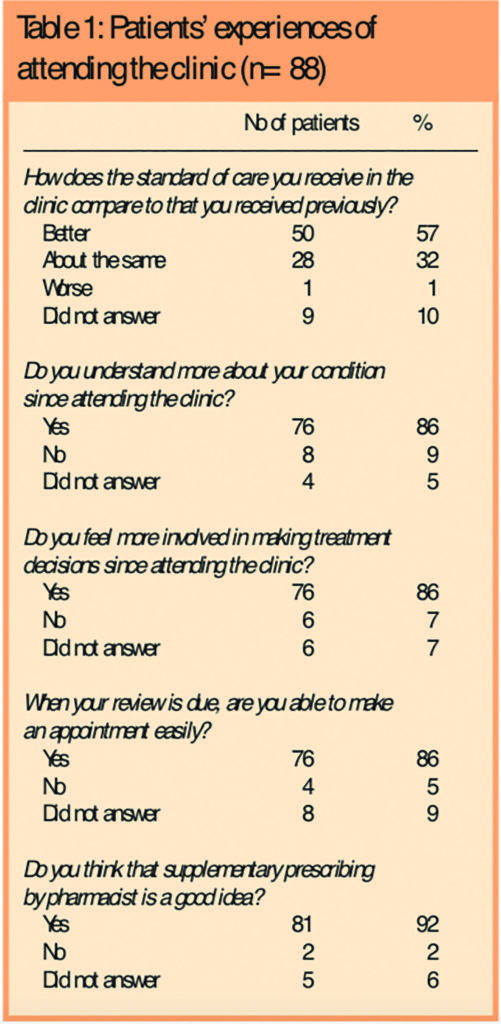
The remaining questions explored experiences of the 88 respondents who attended the clinic at least once and agreed to participate in supplementary prescribing. The responses are summarised in Table 1.
A space at the end of the questionnaire invited additional comments. Twenty-one respondents (20 per cent) added comments. Of these 17 were positive, and four offered suggestions for improvement. Some of the comments are given in the Panel.
Panel: Some respondents’ comments on the service
“After only three appointments I feel that the clinic is a great asset to our practice. I have benefited from a recent routine ECG, which showed that, unknowingly, I have had a slight heart attack. The proposed care plan has been explained in a most reassuring way.”
“Since attending the clinic I feel that someone cares about my health and has made me more aware of how to take care of myself.”
“I think the new system is first class. I, as a patient, can’t praise it enough.”
“I have been given lots of information and this has enabled me to make informed choices about my medication. I feel that I have some control and am pleased with the service.”
“Just thank you.”
Discussion
A recognised limitation of postal questionnaires is the response rate, although a response rate of 75 per cent is considered good. I achieved a response rate of 87 per cent, increasing the validity of the results by reducing the effect of non-respondent bias.10 When patients are identified as suitable for our clinic, an invitation to attend an appointment is sent, together with an information leaflet explaining supplementary prescribing. Seventeen per cent of respondents chose not to attend this initial appointment. The most frequent reason given for non-attendance was that the appointment time was inconvenient. The appointment letter does invite the patient to rearrange if the given time is inconvenient, but this may not be actioned, especially if the letter is read quickly. An alternative would be to invite patients to make an appointment at a time that suits them. This may increase the attendance rate, but reduces our ability to manage the clinic’s workload.
Currently the clinic is limited to two afternoons each week, so even altering the time of the appointment may prevent some patients from attending. I recognise that the timings of our clinic are restrictive, which is due to pharmacist availability, room availability and funding. Any future extension of the clinic should incorporate morning clinics, which may increase attendance of those patients for whom afternoon clinics are inconvenient.
The patient information leaflet that is sent with the invitation to attend the clinic briefly outlines the process of supplementary prescribing and includes the potential benefits of attendance. This may contribute to the number of respondents who cited that they did not attend the clinic because they preferred to continue with GP/nurse-led care or preferred not to see a pharmacist. However, I think it is appropriate for patients to receive written information relating to supplementary prescribing before they attend the clinic where they are asked to give their verbal consent to their care to be managed by another member of the health care team.
Nine respondents (8 per cent) stated that they did not attend or continue to participate in the clinic because they preferred to continue with GP/nurse-led care. This would be a useful area to explore further using qualitative methods and would then allow us to gain a greater understanding of our patients’ perception of the pharmacist’s position in primary care.
Another reason given for non-attendance was that the letter of invitation to attend an appointment was not received. The letter may have been lost in the post or the patient may not have recalled receiving it, especially as letter may have been sent up to a year previously. Sending a second letter to patients who do not attend may reduce the number of patients who do not attend for this reason.
Eighty-three per cent of respondents attended their first appointment, of whom 99 per cent agreed to participate in the clinic. Eight per cent have since dropped out. The main reason cited for no longer attending the clinic was the development of a new condition. This is largely due to the diagnosis of non-insulin dependent diabetes among clinic patients. Once diagnosed, patients are followed up by our nurse-led diabetes clinic and their hypertension care management plan suspended. This is because patients having to attend two separate chronic disease clinics may be time-consuming and potentially confusing for them. Other reasons given for not continuing with the clinic were moving out of the area and preferring to continue with GP/nurse-led care, as discussed above.
Of the respondents who attended the first clinic appointment, 91 per cent continue to attend. This is equivalent to 76 per cent of all respondents. As yet there is no similar work with which to compare these attendance rates. However, it is fair to say that they imply that our clinic has a good level of patient acceptability.
Fifty-seven per cent of patients who attended our clinic stated that they thought that the standard of care received was better and 32 per cent that it was about the same as that which they received previously. In addition, 86 per cent of respondents stated that they understand more about their condition and felt more involved in treatment decisions since attending the clinic. This is especially important in the management of long-term conditions such as hypertension, where patient compliance with lifestyle advice and medication is paramount. However, it should be remembered that how patients responded to these questions depends on their previous experience of GP/nurse-led care. For example, newly diagnosed patients who have limited knowledge of their condition may be more likely to state that the clinic has improved their knowledge than those who were diagnosed as hypertensive some years before. In addition, these findings concur with previously published work regarding a primary care pharmacist-led hypertension clinic, which reported that 76 per cent of patients said that their understanding of their condition had improved since attending the clinic.8
One of the Department of Health’s stated aims of supplementary prescribing was to provide patients with quicker and more efficient access to medicines.1 Eighty-six per cent of respondents stated that they are able to make appointments easily, which subsequently aids their access to medicines. As our clinics continue to develop we must continue to monitor our appointment availability, as lack of availability could be detrimental to patient satisfaction.
Ninety-two per cent of respondents who attended our clinic stated that supplementary prescribing by pharmacists is a good idea. This is remarkable considering this group of patients, many of whom were invited to attend as a result of a computer record search, have a maximum of one year’s experience of supplementary prescribing. This is similar to the University of Southampton’s research into the first two years of extended formulary nurse prescribing, which showed that independent nurse prescribing was viewed positively by patients.11 Although not directly comparable, both studies indicate a general acceptance of non-medical prescribing by patients.
When invited to make further comments the majority were positive. Four patients offered suggestions for service improvement. Two patients asked for the clinic to be extended to allow morning appointments. This has been noted by the practice, but is not currently possible as discussed above. One patient had asked for his annual blood tests for hypertension and another condition to be synchronised. The situation described by the patient was the result of an administrative error, because the practice aims to synchronise all blood tests whenever practical. One patient requested that a reminder is sent when the six-monthly review is due. This has since been implemented in the practice.
The study demonstrates a positive patient experience. However, our clinic operates using 20-minute appointments, rather than the practice standard of 10 minutes. This positive patient experience may therefore be, at least in part, due to the extended contact time with a health professional. This potential bias could have been excluded if the clinic had used the practice standard of 10-minute appointments. However, 20-minute appointments were chosen to allow the patient to participate fully in the consultation, thus allowing a prescribing partnership, one of the key principles of supplementary prescribing, to develop.
As supplementary prescribing and, therefore, research relating to supplementary prescribing are still in their infancy, the evidence base is limited. My study strengthens the results recent work investigation patient experience of a supplementary prescribing rheumatology outpatient clinic4 and suggests that patient acceptance of supplementary prescribing extends across the primary/secondary care interface and across different chronic diseases. Further work would be useful to determine if these levels of patient satisfaction extend across all chronic diseases and if certain patient characteristics leads them to be more accepting of supplementary prescribing.
Although this study has produced favourable results, its limitations should not be ignored. The non-response rate, although low at 13 per cent, builds a degree of bias into the results. In addition, all questionnaires suffer from a degree of recall bias, and it could be argued that those patients who are satisfied with the clinic are more likely to respond to the survey. Another limitation is the study design. Asking all those invited to the clinic to comment on their experience includes those who have attended several clinics and those who have attended just once. Those who have limited experience of the clinic may have refrained from answering certain questions, which would increase the proportion of questions the remained unanswered. This would be a useful area to explore using a qualitative approach to explore patients’ beliefs in more detail. A more comprehensive study could have been achieved by using both qualitative and quantitative methods.
Conclusion
This study has shown that patients are generally happy to attend pharmacist-led supplementary prescribing hypertension clinics. Patients generally believed that the standard of care was better and that their understanding about their condition and involvement in treatment decisions had improved. Overall patients stated that supplementary prescribing by pharmacists is a good idea.
Acknowledgements
I thank Derwent Valley Medical Practice, particularly Dr Anna Frain and Dr John Frain for giving me the opportunity to prescribe, and Marian Bradley for her support and comments.
This paper was accepted for publication on 19 March 2006.
About the author
Lorna Smalley, BPharm, MRPharmS, is practice pharmacist at Derwent Valley Medical Practice, 20 St Marks Road, Derby DE21 6AT (e-mail lorna.smalley@nhs.net)
References
- Department of Health. Pharmacists to prescribe for the first time. Nurses will prescribe for chronic illness (Press Release 2002/0488). November 2002
- First pharmacist prescribers registered by Society. Pharmaceutical Journal 2005;272:235.
- Department of Health. Supplementary prescribing by nurses and pharmacists within the NHS in England. A guide for implementation. London: The Department; 2003.
- Thomas M, Motion M. Setting up supplementary prescribing clinics can be rewarding and exciting. Pharmacy in Practice 2005;15:319–22.
- Pharmacist prescribing evaluation to begin. Pharmaceutical Journal 2005;275:4.
- Bath University to investigate supplementary prescribing. Pharmaceutical Journal 2004;273:371.
- Smalley L. Supplementary prescribing in action — an example from primary care. Pharmaceutical Journal 2005;274:213–4.
- Reid F, Murray P, Storrie M. Implementation of a clinic for pharmacist review of hypertensive patients in primary care. International Journal of Pharmacy Practice 2003;11(Suppl):R74.
- Vivian EM. Improving BP control in a pharmacist managed hypertension clinic. Pharmacotherapy 2000;22:1533–40.
- Bowling A. Research methods in health. Investigating health and health services (2nd edition). Philadelphia: Open University Press; 2002.
- Department of Health. Patients positive about nurse prescribing (Press Release 2005/0223). June 2005

