Key points
- Medication-related osteonecrosis of the jaw (MRONJ) is a rare complication that typically presents following a dental extraction in some patients prescribed anti-resorptive or anti-angiogenic drugs.
- MRONJ is challenging to treat and can have a significant negative effect on quality of life; therefore, prevention of the condition is important.
- Patients should undergo remedial dental work prior to the initiation of implicated medicines and maintain good oral hygiene throughout treatment.
- A multidisciplinary team approach to the prevention of MRONJ is recommended, with pharmacists playing a vital role in the education of patients on appropriate preventative measures.
- Improved communication and interprofessional collaboration between medical and dental colleagues could improve patient outcomes.
Introduction
Oral health promotion has traditionally been the preserve of dental professionals; however, with the increasing recognition of the link between oral and general health, there is a greater importance in other healthcare professionals promoting oral health. In 2016, Wilson and Soni — the former presidents of the British Dental Association and Royal Pharmaceutical Society, respectively — published an opinion piece in the British Dental Journal emphasising the opportunities for pharmacy and dentistry to lead a new era of interprofessional healthcare and integrate dentistry in general healthcare provision[1]
. Opportunities discussed included collaboration to improve oral cancer screening, the management of diabetes and the oral health of patients in residential care homes
1.
A major area of overlap between the two professions relates to the adverse effects of medicines; there are several established adverse effects of medicines that can impact negatively on patients’ oral health. These include xerostomia (dry mouth), taste disturbances, increased salivation, gingival overgrowth and osteonecrosis of the jaw[2],[3],[4]
.
Case reports of osteonecrosis of the jaw linked to bisphosphonate therapy began to emerge in the early 2000s. Bisphosphonate-related osteonecrosis of the jaw is now well documented in the literature and has been subject to several prescribing safety alerts from the Medicines and Healthcare products Regulatory Agency and the European Medicines Agency[4],[5],[6]
. Although oral bisphosphonates remain the most commonly implicated prescribed agents, several other medicines that are used in the management of osteoporosis, Paget’s disease or in the treatment of cancer have subsequently been attributed to the potential development of osteonecrosis of the jaw (see Table 1). This has led to a change in the terminology used to describe the condition — it is now referred to as medication-related osteonecrosis of the jaw (MRONJ)[7]
.
| Drug class | Drug name | Trade name(s) | Indication(s) |
|---|---|---|---|
Anti-angiogenic drugs | Aflibercept | Zaltrap (Sanofi, Berkshire) | Cancer |
| Bevacizumab | Avastin (Roche, Hertfordshire) | Cancer | |
| Sunitinib | Sutent (Pfizer, Kent) | Cancer | |
| Bisphosphonates | Alendronic acid | Binosto (Internis Pharmaceuticals, West Yorkshire) Fosamax (Merck Sharp & Dohme, Hertfordshire) Fosavance (Merck Sharp & Dohme, Hertfordshire) | Osteoporosis |
| Ibandronic acid | Bondronat (Atnahs Pharma UK, Basildon) Bonviva (Atnahs Pharma UK, Basildon) Iasibon (Pharmathen SA, Greece) Quodixor (Aspire Pharma, Hampshire) | Osteoporosis Cancer | |
| Sodium clodronate | Bonefos (Bayer, Reading) Clasteon (Beacon Pharmaceuticals, Tunbridge Wells) Loron (Intrapharm Laboratories, Berkshire) | Bone pain Cancer | |
| Sodium pamidronate | Aredia (Novartis, Surrey) | Paget’s Disease Bone pain Cancer | |
| Sodium risedronate | Actonel (Warner Chilcott UK, Devon) Actonel Combi (Warner Chilcott UK, Devon) | Osteoporosis Paget’s Disease | |
| Zoledronic acid | Aclasta (Novartis, Surrey) Zometa (Novartis, Surrey) | Osteoporosis Paget’s Disease Cancer | |
| RANKL inhibitors | Denosumab | Prolia (Amgen, Cambridge) Xgeva (Amgen, Cambridge) | Osteoporosis Cancer |
RANKL: receptor activator of nuclear factor kappa-beta ligand. Data correct at the time of publication of source. This list is not exhaustive. Be aware that drug trade names can change and new drugs may be released that may be implicated in medication-related osteonecrosis of the jaw (MRONJ). Consult the Scottish Dental Clinical Effectiveness Programme website ( Source: reproduced with permission from the Scottish Dental Clinical Effectiveness Programme | |||
MRONJ is a complex phenomenon. The official definition provided by the American Association of Oral and Maxillofacial Surgeons is: “Exposed bone or bone that can be probed through an intra-oral or extra-oral fistula, in the maxillofacial region, that has persisted for more than eight weeks in patients with a history of treatment with anti-resorptive or anti-angiogenic drugs, and where there has been no history of radiation therapy to the jaw or no obvious metastatic disease to the jaws[7]
.”
See the Photoguide for the intra-oral appearance of a patient with MRONJ.
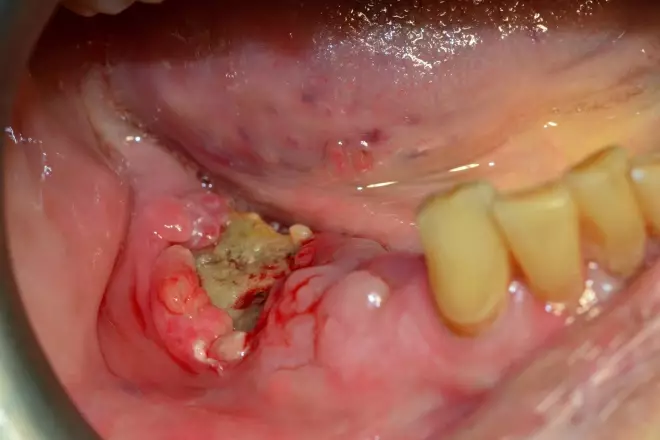
Photoguide: The intra-oral appearance of a patient with medication-related osteonecrosis of the jaw
Source: Dr F. Graziani and Dr Nisi
Exposed necrotic bone is evident in the lower right region of the mandible, following extraction of the posterior teeth
This article will provide an overview of the condition and discuss the evidence base for the role of pharmacists as part of a multidisciplinary team in preventing MRONJ, focusing on the different settings where they may interact with patients and people who are at risk.
Pathophysiology
The pathophysiology of MRONJ has not been fully determined. However, its occurrence is thought to be related to the unique nature of the blood supply, structure and function of the jaw bones, and the microbiology of oral plaque biofilm in contributing to lesion development. The jaw bones (maxilla and mandible) have a high blood supply, which may result in an increased concentration of implicated medicines in this area. Furthermore, in alveolar bone (the part of the jaw bone that supports the teeth) remodelling occurs at a much higher rate than elsewhere in the skeleton (likely as a result of forces related to chewing and the presence of teeth) and thus there is a higher uptake of implicated medicines in the alveolar bone compared with other bones in the body[8]
.
Epidemiology
It is difficult to provide precise prevalence rates for MRONJ, with varying reports published in the literature[9]
. The current consensus is that the estimated incidence of MRONJ in patients with cancer treated with anti-resorptive or anti-angiogenic drugs is 1%, and in patients with osteoporosis treated with anti-resorptive drugs it is 0.01–0.1%[9]
.
Risk factors
With an ageing population, and a specific focus on the prevention of skeletal-related events (SREs; e.g. bone fractures), the prescription of oral bisphosphonates has increased considerably over recent years: in England, prescribing data show 6,007,071 individual supplies of alendronic acid 70mg in 2018, compared with 2,841,358 supplies in 2006[10],[11]
. SREs resulting from cancer that has metastasised to the bone are associated with significant morbidity and reductions in quality of life. Intravenous (IV) bisphosphonates, such as zoledronic acid and the monoclonal antibody denosumab, are licensed for the prevention of SREs in osteoporosis and in patients with bone metastases.
Prescribing rates of other drugs implicated in the development of MRONJ have also risen significantly in recent years and are expected to rise further. The prescription of denosumab has increased, with 52,210 individual supplies in England during 2018 compared with 43,063 supplies in 2017[10],[11]
. The introduction of IV bisphosphonates in the treatment of early breast cancer has also been described as a risk for MRONJ development and equates to a further 20,000 patients per year being prescribed bisphosphonates in the UK[12]
. The overall increase in the prescription of implicated medicines is therefore likely to result in more patients becoming at risk of developing osteonecrosis of the jaw, making this rare condition a greater issue of concern in the context of clinical practice.
Invasive dentoalveolar surgery, which includes commonly performed procedures such as tooth extractions, is a major risk factor in the development of MRONJ, with studies reporting that around 50–60% of patients with MRONJ identified tooth extraction as a specific precipitating event[7]
. The evidence supporting other risk factors is limited, but these include concomitant corticosteroid use, having poor oral hygiene, wearing ill-fitting dentures, tobacco use and having comorbid conditions, such as diabetes and anaemia[7]
. Patients with a previous diagnosis of MRONJ are at a higher risk of developing the condition again[9]
.
Diagnosis
The main symptoms of MRONJ include:
- Pain;
- Exposed necrotic bone in the oral cavity;
- Signs of infection, such as fistula, swelling, cellulitis and pus exudation;
- Tingling and numbness/pins and needles (hypoesthesia or paraesthesia) in the chin or lower lip;
- Loosening of teeth (mobility);
- Bad breath (halitosis)[13]
.
However, diagnosis of MRONJ can be challenging — particularly for non-specialists. Therefore, at-risk patients should be referred for general dental assessment, and specific diagnosis and treatment intervention where necessary, as specified in the summary of product characteristics (SPC) for the major implicated drugs.
Management
MRONJ is difficult to treat, can cause significant morbidity and affects quality of life. A small study of 34 patients with MRONJ using the Oral Health Impact Profile (known as OHIP-14) — a validated and widely used oral health-related quality-of-life indicator — found that the condition significantly (P <0.001) affects quality of life[14]
. Furthermore, a qualitative study of patients diagnosed with MRONJ highlighted significant quality-of-life implications, particularly the physical, psychological and social impacts of the condition[15]
. This includes significant pain, regular use of analgesic medicines and antibiotics, the need for invasive surgery and the social anxiety of eating awkwardly in public.
The elimination or stabilisation of oral disease before initiating anti-resorptive agents is recommended as a preventative strategy for MRONJ in clinical guidelines, owing to the significant morbidity associated with MRONJ and the limited treatment options available[9]
. Therefore, it is important that patients are fully informed about the risk of MRONJ and the appropriate preventative strategies, and are signposted to dental services in case of emergency before these drugs are commenced. Studies have identified that dental screening and preventative strategies reduce the risk of osteonecrosis of the jaw. Dimopoulos et al. reported a statistically significant reduction in the incidence of MRONJ among multiple patients with myeloma that were prescribed zoledronic acid following the implementation of preventative measures: the incidence rate before the implementation of preventative measures was 0.671/100 person-months and 0.230/100 person-months afterwards (information ratio 2.92; 95% confidence interval 1.06–8.03; P =0.029)[16]
. Vandone et al. reported a 50% reduction in the incidence rate after screening and pre-treatment preventative dental care in patients with bone metastases from solid tumours who were prescribed IV bisphosphonates: osteonecrosis of the jaw was observed in 5.5% of patients (n=11/200) not receiving preventative dental measures and 2.8% (n=6/211) in those receiving preventative dental care before and during treatment with bisphosphonates[17]
.
Role of the pharmacist
There is an important opportunity for pharmacists in different settings to provide information to patients and healthcare professionals about the risk and prevention of MRONJ. Evidence to support the current role of pharmacists in this regard is limited: a questionnaire of healthcare professionals in North Wales identified that just 11.8% of GPs (n=120) and 9.7% of pharmacists (n=60) advised patients to alert their dentist to their use of bisphosphonates[18]
. A second small study (n=55) found that the majority of patients acquired knowledge about the drug they were prescribed from the patient information leaflets that are supplied with the medicine (62%), with few patients (13%) receiving this information directly from their GP. When asked to identify adverse effects of bisphosphonate therapy, only 32% of patients receiving IV bisphosponates and 17% of patients receiving oral bisphosphonates were aware of the potential risk of developing MRONJ[19]
.
In a qualitative study of patients diagnosed with MRONJ, participants described a perceived hierarchy in relation to the management of their health; they expected prescribers to utilise professional judgement on the suitability of the medicine for them and to provide information related to the adverse effects of medicines. However, participants highlighted the importance of the pharmacist in reinforcing advice and were positive towards the pharmacist’s role in providing information on medicines and conducting medicine reviews[15]
.
However, a qualitative study of GPs and pharmacists in North East England indicated that both professional groups had limited knowledge of MRONJ and limited awareness of the recommended preventative strategies. Participants overlooked advice related to the risk and prevention of MRONJ, describing instead the often complex histories of patients’ medication history and prioritising other aspects of patient care[20]
. This suggests that patient safety is being compromised as patients are not receiving the appropriate oral health advice or required preventative dental treatment before taking these implicated medicines.
There is, however, a significant challenge in effectively engaging patients in recognising the need for dental care; the most recent Adult Dental Health Survey in 2009 identified that 23% of dentate adults do not attend the dentist at least every two years[21]
. One qualitative study identified several barriers to dental care, including a low priority of oral healthcare, patient phobia of dental treatment and the financial implications of dental care[15]
.
While there is significant literature supporting the role of the pharmacist in relation to the appropriate use of medicines and in multidisciplinary working[22]
, it is limited in relation to the role of the pharmacist in the delivery of oral health advice, particularly working interprofessionally with dental professionals. The prevention of MRONJ necessitates effective multidisciplinary working and represents an opportunity for pharmacists in all settings to provide integrated patient-centred care.
As medicine experts, a major component of pharmacists’ role should include education of other healthcare professionals on the safe and effective use of medicines and the risks of MRONJ — this includes the provision of clinical and medicine advice to dentists, who receive limited pharmacology- and medicine safety-related education compared with pharmacists. This role not only relates to the prevention of MRONJ, but to the management of other new or established medicines that can have an impact on oral health or the safe provision of dental treatment.
Furthermore, it is important that adverse drug reactions are reported, particularly now that MRONJ is associated with medicines other than bisphosphonates. Areas where pharmacists and other healthcare professionals could improve prevention strategies of MRONJ are listed in Table 2.
| Evidence base | Considerations for clinical practice |
|---|---|
| Medication-related osteonecrosis of the jaw (MRONJ) is a rare adverse effect that affects around 1% of patients with cancer who are prescribed anti-resorptive and anti-angiogenic medicines and 0.1% of patients with osteoporosis who are prescribed anti-resorptive medicines for osteoporosis*. |
|
Patients are at highest risk of developing MRONJ following a dental extraction*†. |
|
| MRONJ is difficult to treat; therefore, patients should undergo remedial dental treatment prior to initiating implicated medicines*†. |
|
| Implicated medicines, such as bisphosphonates, have several complicated and important counselling points‡. |
|
| Sources: *Scottish Dental Clinical Effectiveness Programme [9]; †J Oral Maxillofac Surg [7]; ‡ eMC [26] | |
Community pharmacists
These healthcare providers are generally regarded as being easily accessible and, in many cases, provide the most frequent opportunity for patients to access a healthcare professional. Pharmacists in community settings have demonstrated an acceptance that oral healthcare can be part of their professional role and that simple educational interventions can influence positive intentions in relation to the oral health habits of patients[23],[24]
.
Although community pharmacists are unlikely to regularly work with the IV medicines implicated in MRONJ, they dispense millions of prescriptions for oral bisphosphonates nationwide each year. The new medicine service (NMS) is an advanced service within the UK’s NHS ‘Community pharmacy contractual framework’ that supports patients newly prescribed medicines for long-term conditions; however, the service specification does not currently include bisphosphonates[25]
. This is a missed opportunity; leaving the issue of MRONJ aside, this group of medicines has several issues that patients could benefit from being counselled on through an extended discussion and follow-up with their pharmacist. The list of counselling points listed in the SPC for alendronic acid, for example, is extensive and includes the following[26]
: “Take once per week; take on an empty stomach; take with a full glass of plain water; take 30 minutes before food, drink or medicine; avoid coffee, mineral water or juice; swallow whole; do not crush or chew; stay upright; do not lie down until you have eaten a meal; when to take your calcium supplements; oesophageal adverse effects; and use in caution with poor dental health, gum disease or if requiring a dental extraction.”
The NMS could provide the pharmacist and the patient time to have a thorough discussion related to the numerous administration instructions of the drug, facilitate an important discussion on the need to maintain good oral hygiene and oral health, encourage a visit the dentist before initiation and empower patients to make informed decisions.
Like the NMS, the medicines use review (MUR) service does not specifically include bisphosphonates in the service specification[27]
. MURs are also part of the current ‘Community pharmacy contractual framework’ and provide patients with structured, adherence-centred polypharmacy reviews. Although many patients prescribed bisphosphonates have complex needs and may be eligible for an MUR owing to polypharmacy considerations, the fact that bisphosphonates are not included in the service specification is again a potential lost opportunity to reinforce preventative advice to patients.
GP pharmacist
The growth of the pharmacist’s role in general practice also represents a significant opportunity to utilise the extensive knowledge base and skill set in relation to the effective management of medicines. The Primary Care Pharmacy Association’s job description for clinical pharmacists in general practice details examples of duties and responsibilities for pharmacists in this setting[28]
. It includes managing long-term conditions, performing medication reviews, implementing medicine safety guidance, supporting public health campaigns and signposting to appropriate healthcare professionals.
Patients prescribed medicines implicated in the development of MRONJ fall into many of these categories. Pharmacists in this role have access to full medical records, and often co-ordinate discharges from secondary care and the transfer of information between healthcare settings. They are experienced at taking medicine histories and have a major role in ensuring accurate documentation.
Medicines may also be initiated by pharmacist independent prescribers. Patients can have their medicines reviewed as part of a chronic disease management clinic or they can be specifically identified as part of a targeted intervention.
An evaluation of GP pharmacists in pilot studies by the University of Nottingham found that patients benefited from the provision of increased lifestyle advice, and advice that improves medicines adherence and reduces adverse effects[29]
. However, the delivery of oral healthcare education in this setting has not been particularly explored. Pharmacists, commissioners and researchers should be encouraged to be innovative and incorporate oral health advice as an integral part of their current roles; for example, as part of the lifestyle advice that already forms part of medication reviews and chronic disease management clinics.
Secondary care pharmacist
Many of the more recent medicines to be implicated in the development of MRONJ are prescribed, dispensed and administered in secondary care settings[30]
. A referral service for dental screening from haematology and oncology clinics in Wales was established, with more than 90% of the patients referred for screening reporting satisfaction with the service[31]
. Such referral pathways could, and should, naturally incorporate specialist pharmacists involved in the care of higher risk oncology patients or those prescribed IV bisphosphonates or denosumab.
Other roles in an acute setting include the management of patients after falls and fractures, medicine reviews and discharge planning, and deprescribing medicines in line with clinical guidelines to reduce adverse drug effects. Long-term therapy with bisphosphonates represents a potential target for intervention. For example, an interesting finding from one qualitative study was that many patients were unclear on the duration of treatment with bisphosphonates, with some patients having taken these medicines for many years[15]
.
Other collaborative opportunities
The prevention of MRONJ represents just a small proportion of the potential collaborative opportunities for pharmacists and dental professionals. Pharmacists already play a vital role in the prevention of the oral adverse effects of inhaled medicines, such as oral candidiasis and in the provision of smoking cessation services.
There is increasing evidence of a two-way relationship between periodontitis (gum disease) and diabetes. Periodontitis is a chronic inflammatory disease caused by bacterial infection of the supporting tissues surrounding the teeth, which is usually painless and is often left untreated until it reaches an advanced stage[32]
. The Cochrane Collaboration published a review in 2015, highlighting that randomised controlled trials have demonstrated that periodontal therapy is associated with around a 3–4 mmol/mol (0.3–0.4%) reduction in HbA1c levels after three months[33]
; this is a clinical impact equivalent to adding a second drug to a pharmacological regimen[34]
. In most settings, pharmacists regularly see patients who have diabetes, and this represents an opportunity to target patients who can benefit significantly from oral health education.
Mouth and oropharyngeal cancer rank as one of the most common cancers globally, with the highest incidence rates in males aged over 60 years and patients living in deprived areas[35]
. A recent study of oral cancer in Scotland found that in the majority of diagnosed cases, no contact had been made with a dentist in the two years preceding the diagnosis; the study concluded that early detection strategies in alternative settings should be explored, representing another opportunity to involve pharmacists[36]
.
Conclusion
MRONJ is a rare complication that typically presents following a dental extraction in some patients prescribed anti-resorptive or anti-angiogenic drugs. It is difficult to treat and can result in significant negative effects on quality of life. Pharmacists should be aware of this risk and the recommended preventative advice, which could be incorporated into current roles across pharmacy sectors. Further research and exploration of the pharmacist’s role and interprofessional collaboration with medical and dental colleagues may also provide significant benefits to other patient groups in which oral heath advice or interventions could potentially improve patient outcomes.
Financial and conflicts of interests disclosure
The authors have no relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. No writing assistance was used in the production of this manuscript.
Peer review notice
This article has been peer reviewed by relevant subject experts prior to acceptance for publication. The reviewers declared no relevant affiliations or financial involvement with any organisation or entity with a financial interest in or in financial conflict with the subject matter or materials discussed in this article.
References
[1] Wilson N & Soni A. Interprofessional working: a spearhead opportunity for dentistry and pharmacy. Br Dent J 2016;221(10):607–608. doi: 10.1038/sj.bdj.2016.853
[2] Cockburn N, Pradhan A, Taing MW et al. Oral health impacts of medications used to treat mental illness. J Affect Disord 2017;223:184–193. doi: 10.1016/j.jad.2017.07.037
[3] Trackman PC & Kantarci A. Molecular and clinical aspects of drug-induced gingival overgrowth. J Dent Res 2015;94(4):540–546. doi: 10.1177/0022034515571265
[4] McLeod N, Brennan P & Ruggiero S. Bisphosphonate osteonecrosis of the jaw: a historical and contemporary review. Surgeon 2012;10(1)36–42. doi: 10.1016/j.surge.2011.09.002
[5] European Medicines Agency. CHMP Assessment report on bisphosphonates and osteonecrosis of the jaw. 2009. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Report/2010/01/WC500051428.pdf (accessed August 2019)
[6] Medicines and Healthcare products Regulatory Agency. Drug Safety Update: Bisphosphonates: osteonecrosis of the jaw. 2009. Available at: https://www.gov.uk/drug-safety-update/bisphosphonates-osteonecrosis-of-the-jaw (accessed August 2019).
[7] Ruggiero SL, Dodson TB, Fantasia J et al. American Association of Oral and Maxillofacial Surgeons position paper on medicationâ€related osteonecrosis of the jaw – 2014 update. J Oral Maxillofac Surg 2014;72(10):1938–1956. doi: 10.1016/j.joms.2014.04.031
[8] Otomo-Corgel J. Osteoporosis and osteopenia: implications for periodontal and implant therapy. Periodontol 2000 2012:59;111–139. doi: 10.1111/j.1600-0757.2011.00435.x
[9] Scottish Dental Clinical Effectiveness Programme. Oral health management of patients at risk of medication-related osteonecrosis of the jaw. Dental Clinical Guidance. 2017. Available at: http://www.sdcep.org.uk/wp-content/uploads/2017/04/SDCEP-Oral-Health-Management-of-Patients-at-Risk-of-MRONJ-Guidance-full.pdf (accessed August 2019)
[10] NHS Digital. Prescription cost analysis — England, 2017. 2018. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/prescription-cost-analysis/prescription-cost-analysis-england-2017 (accessed August 2019)
[11] NHS Digital. Prescription cost analysis —England 2018. 2019. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/prescription-cost-analysis/2018 (accessed August 2019)
[12] Patel V, Mansi J, Ghosh S et al. MRONJ risk of adjuvant bisphosphonates in early stage breast cancer. Br Dent J 2018;224(2):74–79. doi: 10.1038/sj.bdj.2017.1039
[13] Otto S, Pautke C, Wyngaert T et al. Medication-related osteonecrosis of the jaw: prevention, diagnosis and management in patients with cancer and bone metastases. Cancer Treat Rev 2018;69:177–187. doi: 10.1016/j.ctrv.2018.06.007
[14] Miksad RA, Lai K-C, Dodson TB et al. Quality of life implications of bisphosphonate-associated osteonecrosis of the jaw. Oncologist 2011;16(1):121–132. doi: 10.1634/theoncologist.2010-0183
[15] Sturrock A, Preshaw PM, Hayes C & Wilkes S. Perceptions and attitudes of patients towards medication-related osteonecrosis of the jaw (MRONJ): a qualitative study in England. BMJ Open 2019;9:e024376. doi: 10.1136/bmjopen-2018-024376
[16] Dimopoulos MA, Kastritis E, Bamia C et al. Reduction of osteonecrosis of the jaw (ONJ) after implementation of preventative measures in patients with multiple myeloma treated with zolendronic acid. Ann Oncol 2009;20(1):117–120. doi: 10.1093/annonc/mdn554
[17] Vandone AM, Donadio M, Mozzati M et al. Impact of dental care in the prevention of bisphosphonate-associated osteonecrosis of the jaw: a single-center clinical experience. Ann Oncol 2012;23(1):193–200. doi: 10.1093/annonc/mdr039
[18] Masson D, O’Callaghan E & Seager M. The knowledge and attitudes of North Wales healthcare professionals to bisphosphonate associated osteochemonecrosis of the jaws. Journal of Disability and Oral Health 2009;10:175–183
[19] Bauer JS, Beck N, Kiefer J et al. Awareness and education of patients receiving bisphosphonates. J Craniomaxillofac Surg 2012;40(3):277–282. doi: 10.1016/j.jcms.2011.04.011
[20] Sturrock A, Preshaw P, Hayes C & Wilkes S. Attitudes and perceptions of GPs and community pharmacists towards their role in the prevention of bisphosphonate-related osteonecrosis of the jaw: a qualitative study in the North East of England. BMJ Open 2017;7:e016047. doi: 10.1136/bmjopen-2017-016047
[21] Morris J, Chenery V, Douglas G & Treasure E. Service considerations—a report from the Adult Dental Health Survey 2009. 2011. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/adult-dental-health-survey/adult-dental-health-survey-2009-summary-report-and-thematic-series (accessed August 2019)
[22] Tan ECK, Stewart K, Elliott RA & George J. Pharmacist services provided in general practice clinics: a systematic review and meta-analysis. Res Social Adm Pharm 2014;10(4);608–622. doi: 10.1016/j.sapharm.2013.08.006
[23] Mann RS, Marcenes W & Gillam DG. Is there a role for community pharmacists in promoting oral health? Br Dent J 2015;218(5):E10. doi: 10.1038/sj.bdj.2015.172
[24] Sturrock A, Cussons H, Jones C et al. Oral health promotion in the community pharmacy: an evaluation of a pilot oral health promotion intervention. Br Dent J 2017;223(7):521–525. doi: 10.1038/sj.bdj.2017.784
[25] Pharmaceutical Services Negotiating Committee. New Medicines Service. 2011. Available at: http://psnc.org.uk/services-commissioning/advanced-services/nms/ (accessed August 2019)
[26] eMC. Alendronic acid 70mg tablets. Available at: https://www.medicines.org.uk/emc/product/5206/smpc#POSOLOGY (accessed August 2019)
[27] Pharmaceutical Services Negotiating Committee. Medicines Use Review. 2019. Available at: http://psnc.org.uk/services-commissioning/advanced-services/murs (accessed August 2019)
[28] Primary Care Pharmacy Association. Primary care networks clinical pharmacists job descriptions. 2018. Available at: https://www.pcpa.org.uk/454kgekwj545c87as234lg/PrimaryCareNetworksClinicalPharmacistsJDs-V3.pdf (accessed August 2019)
[29] Mann C, Anderson C, Avery A et al. Clinical Pharmacists in general practice: pilot scheme — independent evaluation report. 2018. Available at: https://www.nottingham.ac.uk/pharmacy/documents/generalpracticeyearfwdrev/clinical-pharmacists-in-general-practice-pilot-scheme-full-report.pdf (accessed August 2019)
[30] NHS Digital. Prescribing costs in hospitals and the community, England 2017/18. 2018. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/prescribing-costs-in-hospitals-and-the-community/2017-18 (accessed August 2019)
[31] Muthukrishnan A, Al-ismail S, Bertelli G et al. MRONJ risk reduction pathway — 360 degree survey. Br Dent J 2017:222:386–390. doi: 10.1038/sj.bdj.2017.225
[32] Bissett SM, Stone KM, Rapley T et al. An exploratory qualitative interview study about collaboration between medicine and dentistry in relation to diabetes management. BMJ Open 2013;3:e002192. doi: 10.1136/bmjopen-2012-002192
[33] Simpson TC, Weldon JC, Worthington HV et al. Treatment of periodontal disease for glycaemic control in people with diabetes mellitus. Cochrane Database Syst Rev 2015;11:CD004714. doi: 10.1002/14651858.CD004714.pub3
[34] Chapple IL & Wilson NH. Manifesto for a paradigm shift: periodontal health for a better life. Br Dent J 2014;216:4. doi: 10.1038/sj.bdj.2014.97
[35] Purkayastha M, McMahon A D, Gibson J & Conway DI. Trends of oral cavity, oropharyngeal and laryngeal cancer incidence in Scotland (1975–2012) – a socioeconomic perspective. Oral Oncol 2016;61:70–75. doi: 10.1016/j.oraloncology.2016.08.015
[36] Purkayastha M, McMahon AD, Gibson J & Conway DI. Is detecting oral cancer in general dental practices a realistic expectation? A population-based study using population linked data in Scotland. Br Dent J 2018;225(3);241–246. doi: 10.1038/sj.bdj.2018.544
You may also be interested in

GPhC writes to pharmacy teams after methotrexate dispensed with instruction to take once daily
Medicines commission calls for greater clarity on risk of suicidal behaviour from antidepressants
