AIM
• To obtain information on levels of service provision for drug users in community pharmacies and to assess the need for further developments.
DESIGN
• A confidential questionnaire.
SUBJECTS AND SETTINGS
• 161 community pharmacies in Bro Taf, a health authority in South Wales.
RESULTS
• A response rate of 89% (161/180) was achieved. 55% (88/160) dispensed Controlled Drugs, most doing so daily. 25% (40/161) supervised methadone consumption. 23% (38/161) were currently involved in needle exchange, with a further 15% (24/161) willing to be involved. 55% (88/161) were prepared to sell needles.
CONCLUSIONS
• Levels of provision have stayed relatively constant over the past decade, despite the number of drug users presenting to services having increased. Fortunately, pharmacists still wish to be better informed and many are willing to expand their services to drug users.
Over the past 20 years, the spread of human immunodeficiency virus (HIV) and hepatitis among the injecting drug user population has been attributed to the communal use of a limited supply of needles and syringes, and ignorance about what constitutes high-risk behaviour. For example, many drug users are unaware of the risk of transmission of hepatitis C from shared spoons. This has prompted various harm-minimisation strategies to be adopted by the many services concerned. Needle and syringe exchange schemes (NES) were piloted in the United Kingdom in 19871 and have since been taken up nationwide as an effective means of supplying clean injecting equipment and providing safe disposal
points for contaminated equipment. The Royal Pharmaceutical Society recognised the importance of the community pharmacy’s role in this drive, issuing guidelines for those involved in NES2 and revoking restrictions on the sale of injecting equipment to drug misusers in 1986.3 Community pharmacies play a vital part in the provision of needle and syringe exchange,4 providing anonymity and accessibility that drug users in many areas would otherwise lack. Pharmacists also contribute to improving the health of drug users in other ways. Dispensing Controlled Drugs, notably methadone, is an essential component of any harm minimisation service5 and is frequently the primary responsibility of community pharmacists. Supervised consumption of methadone, to ensure compliance, reduce leakage to the black market and prevent accidental overdose among non-tolerant opiate users, is now seen as an
important element of any prescribing service, with community pharmacies being principally involved.6,7
Surveys of pharmacies across the UK have shown a trend towards the provision of more services for drug users. Cross-sectional surveys in England and Wales8,9 show that the number of pharmacies dispensing Controlled Drugs doubled, between 1988 and 1995 from 23 per cent to 50 per cent. The
provision of clean injecting equipment also increased from 28 per cent to 35 per cent of community pharmacies selling equipment, and from 3 per cent to 19 per cent of pharmacies involved in needle exchange. A survey of Scottish pharmacies found similar levels of provision.10 Pharmacist supervision
of methadone consumption is also expanding. Almost 20 per cent of pharmacists in Scotland currently supervise consumption, with a further 14 per cent willing to do so if there was demand.10 Two-fifths of pharmacies in England and Wales agree that this would be an acceptable role for them, but no data have been presented on those actually providing this service.11
The study reported here looks at provision within Bro Taf, a health authority in South Wales. Bro Taf was formed by the merger of South Glamorgan and three-fifths of Mid Glamorgan in 1997 and currently has a resident population of just less than 750,000. The main city of Cardiff is home to just over 320,000, with the remaining 418,000 spread through Merthyr and Rhondda Cynon Taf (RCT) in the north and the Vale of Glamorgan in the south.
In 1990 and 1991, two surveys, which included RCT and Merthyr, showed that 92 per cent of pharmacists were willing to participate in a four-tier, pharmacy-based harm reduction scheme, ranging from information and referral only, to formal needle exchanges.5 In RCT and Merthyr, a successful scheme of supervised methadone consumption was also established,7 but this has not been extended across the authority. The NES in the area now covered by Bro Taf Health Authority was established in 1989, following allocation of funds from the Welsh Office, and operated initially from the Community Drug Team premises. In 1993, as a response to a Welsh Office circular, community pharmacy based NES were established.12 The aim of this study is to revisit local services, reassess levels of provision for drug users in Bro Taf and discuss options for further development in the light of greater national recognition of the issues.
METHOD
Between January and April 2000, copies of a confidential questionnaire asking pharmacists their opinions and involvement in a range of harm reduction strategies for drug users were hand-delivered to all 180 community pharmacies listed by the Bro Taf Health Authority. One questionnaire per pharmacy
was provided and was accompanied by a covering letter outlining the purpose and background of the research5 and a prepaid, addressed envelope for its return. The research questionnaire derived from the survey used by Sheridan and Strang,13 was modified to include more questions on the dispensing of Controlled Drugs and a short section on over-the-counter drugs misuse was added.14 From May 2000, those who had failed to return their responses were reminded by telephone and, if necessary, sent a second questionnaire and prepaid envelope.
RESULTS
Demographics
An 89 per cent (161/180) return rate was achieved after the allocated data collection period. Fifty-five per cent (87/161) of responses were from independent businesses. Seventy-seven per cent (125/161) of respondents were regular full time pharmacists. Eighty-six per cent (135/161) either had full or partial responsibility for making decisions regarding service provision to drug misusers. The average
number of years that respondents had practised as a community pharmacist in the UK was 15.5 years (SD = 10; range 0.5–40; 3 missing values).
Training
Forty per cent (64/161) of pharmacists reported having participated in previous training on drug misuse and 16 percent (25/161) on HIV/hepatitis prevention. Just over half of all drug misuse training had
been through distance learning (34/64). Eighty per cent (129/161) of pharmacists expressed an interest in receiving further training on both subjects.
Dispensing Controlled Drugs
Fifty-five percent (88/160) of pharmacists reported that they currently dispensed Controlled Drugs.
Forty-six per cent (73/160) dispensed opioid prescriptions to a total of 247 persons (mean = 3.4; SD = 3.4; range 1–20) and 10 per cent (16/160) dispensed amphetamine prescriptions to 19 individuals (mean = 1.2; SD = 0.4; range 1–2). Fourteen per cent (23/160) of pharmacists dispensed other drugs used for the treatment of addictions including benzodiazepines, disulfiram and acamprosate (n = 76; mean = 3.3; SD = 3; range 1–12). Twenty-seven per cent (44/161) of pharmacists stated that the main reason for not dispensing drugs for the treatment of addiction was the lack of such clients at the time. Only a small minority (5/161) expressed negative attitudes towards drug users, preferring not to have drug users in the pharmacy. Forty-two per cent (67/161) of the pharmacists dispensed regular prescriptions to a total of 200 clients on a daily basis (mean = 3; SD = 2.6; range 1–16) and 13 per cent
(21/161) of the pharmacists dispensed these prescriptions two to three times a week to 31 individuals (mean = 1.5; SD = 0.8; range 1–4). In the UK, these were usually Schedule 2 Controlled Drugs in relation to the Misuse of Drugs Act, 1971 (ie, methadone and dexamphetamine). Twenty-one per cent (33/161) of the pharmacists dispensed prescriptions weekly to 72 clients (mean = 2.2; SD = 1.9; range 1–10) and six per cent (10/161) of the pharmacists dispensed prescriptions for 19 people fortnightly or monthly (mean = 1.9; SD = 0.7; range 1–3). These were usually Schedule 3 Controlled Drugs, such as diazepam. Sixty-five per cent of prescriptions were provided by specialist addiction agencies (223/342) and 30 per cent (102/342) provided by GP’s (17 missing values). In England and Wales, a pink prescription form, FP10HP(AD), is used by doctors at addiction agencies to prescribe a total of 14 days’ treatment, to be dispensed in installments of any drug listed in Schedule 2. GPs tend to use the equivalent FP10(MDA) forms (blue).
Supervised consumption of daily methadone
Twenty-five per cent (40/161) of pharmacists reported that they currently supervised the consumption of a total of 107 methadone prescriptions (mean = 2.7; SD = 2.5; range = 1–14). Thirty-one percent (50/161) of pharmacists did not have methadone clients at the time of the survey. Twenty-one per cent (33/161) reported that they had not been requested to supervise consumption by GPs or specialist agencies. Fifteen per cent (24/161) gave no reason. Fourteen pharmacists (9 per cent) specified reasons for not participating in such a process, including lack of space, issues regarding company policy, staff shortages, absence of an agreed payment level and negative attitudes towards methadone clients.
Participation in harm reduction strategies
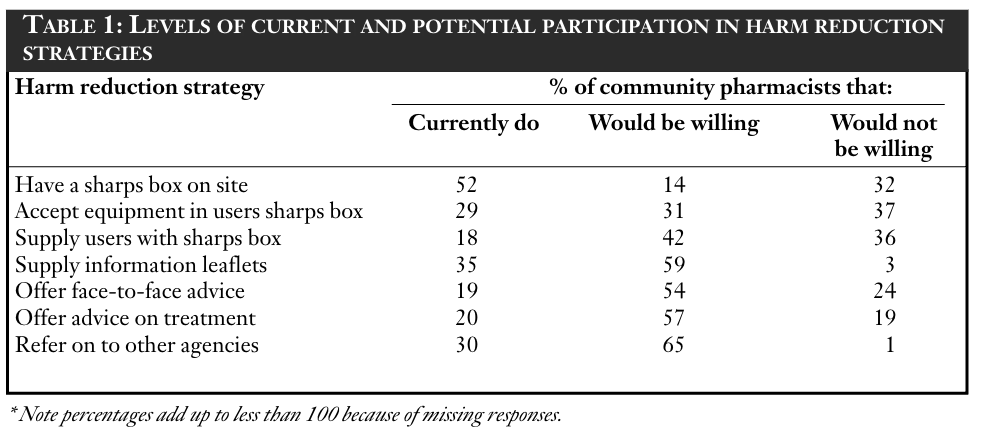
Pharmacists were asked to reflect on their personal position on a number of different harm reduction strategies. Respondents indicated their current participation and willingness or unwillingness to participate in various levels of harm reduction. Table 1 shows their levels of participation. Participation in an NES Twenty-three percent (38/161) of pharmacies are currently participating in an NES. Eight per cent (13/161) of pharmacies had previously participated in the scheme but had withdrawn. Reasons for stopping needle exchange included past problems with drug users (4/13), no demand (2/13), low needle return rate (2/13), fear of risk to staff (1/13) and detrimental effects to business (1/13). Fifteen per cent (24/161) of pharmacists were willing to consider joining the scheme. Fifty-three per cent (84/161) of pharmacists had never participated in the NES and were not currently considering doing so. The most frequent reason given for non-participation was the presence of a needle exchange facility nearby (10/84). Other reasons included risk to staff (8/84), worries about the effect on business (4/84),
company policy (9/84), perceived lack of request for participation (5/84) and practical concerns such as lack of sufficient space on the premises (3/84). Some doubts as to the effectiveness of the scheme were expressed (4/84), as well as the view that the community pharmacy was inappropriate for this type of scheme (2/84). Twenty-nine per cent (24/84) gave no reason for not participating.
Other local NES
Participants were asked if they knew of a needle exchange (pharmacy based, or other) or an organised facility for the disposal of used equipment within a 1 mile radius of their pharmacy (excluding their own). Forty-one per cent (64/156) of pharmacists said that there was a needle exchange facility nearby; a further 39 per cent (61/156) did not know. Twenty per cent of respondents (31/156) reported that there was not a needle exchange facility nearby (5 missing values).
Requests to purchase needles and syringes
During the past week, 65 requests to purchase injecting equipment were reported by 16 per cent (25/161) of the pharmacists (mean = 2.6; SD = 2.6; mode = 2; range 1–10). Two hundred and thirty-two requests were reported by 35 per cent (56/161) of pharmacists for the past month (mean = 4.1; SD = 6.8; mode = 2; range 1–40).
Willingness to sell needles and syringes to drug misusers
Fifty-five per cent (88/161) of pharmacists responded that they currently do, or were willing to, sell injecting equipment to drug misusers. Of these, some pharmacies did not report current sales due to “lack of demand”. Among the 45 per cent who were not willing to sell equipment, the main reason, given by 17 per cent (28/71) of pharmacists, was concern about the disposal of used needles. Other reasons given included company policy 7 per cent (5/71), past problems with drug misusers 4 per cent (3/71) and the view that it is inappropriate for needles to be supplied by community pharmacies 6 per cent (4/71).
Patterns of sale among those pharmacists selling injecting equipment
All pharmacists sold either 1ml or 0.5ml injecting equipment. Eighty-nine per cent (35/38) of pharmacists sold either Microfine 1ml or 0.5ml or both, while others sold other brands. The 1ml syringes were more commonly sold. A total of 371 “injecting sets” (an “injecting set” denotes equipment purchased for one injection: a needle, a needle and barrel or a complete syringe) were estimated to be sold each week by the 31 relevant pharmacists (mean = 12; SD = 29.6; mode = 1; range 1–100). Twenty-nine per cent (9/31) of pharmacists commented that they only made “occasional” sales. Sixty-six per cent (20/31) of those who sold injecting equipment sold packs of 10 syringes, while the remaining 11 sold single “injecting sets”.
DISCUSSION
Hand delivery of the questionnaires and personal contact with the participating pharmacists led to a high response rate. This provides a representative sample from which conclusions about local developments can reasonably be drawn. Despite differences in the area covered and the details of the questionnaire, it is instructive to discuss the results in relation to previous studies.5,13 This survey differs from surveys conducted in 1990 and 19915 in that it was not anonymous, but confidential, enabling non-respondents to be traced, and the results will be used for service development.
In 1991, 30 (27 per cent) pharmacists were willing to participate in the NES and 37 (33 per cent) were willing to sell injecting equipment in Mid Glamorgan.5 Four years later, 31 per cent (43/137) of pharmacies from across Wales were operating an NES and a further 26 per cent (35/137) were willing to set up a scheme in their area, 34 percent (46/137) of pharmacies currently sold injecting equipment to known or suspected drug users, and another 42 per cent (58/137) were willing to sell kits if there was the demand.13 This survey’s findings show that 23 per cent (38/161) of pharmacies are participating in the NES and 55 per cent (88/161) of pharmacies are willing to sell needles. Comparing current levels of NES in Bro Taf with those found in Mid Glamorgan in 1991 and across Wales in 1995, it can be seen that there has been little growth in the past decade.
In 1996/1997, 24 “active” sites out of 49 pharmacies in Bro Taf supplied 12,975 kits (each kit contains 10 needle/syringe combinations). In 1999/2000, 23 “active” sites out of 37 pharmacies supplied only 12,668.15 In 1996, the Welsh Drug Misuse Database16 (DMD; now the National Drug Treatment Monitoring System, NDTMS) reported 648 notifications of drug users in Bro Taf. Opioid-based substances accounted for 15 per cent of new cases and stimulants 20 per cent.16 By 1999, the number of notifications had doubled (n = 1,425). Opioid-based substances accounted for 28 per cent and stimulants 16 per cent.17 The Welsh DMD17 showed that the levels of injecting by new cases throughout Wales had increased by 20 per cent from 466 in 1996 to 560 in 1999. Moreover in 1999, 22.4 per cent of these cases had shared within the previous month, almost reaching the level for 1992. Such statistics suggest that levels of provision have failed to keep up with increasing need.
The provision of harm minimisation services implies the safe disposal of used injecting equipment as well as ease of access to supply. With only 29 per cent of community pharmacists currently accepting equipment in users’ own sharps boxes and 18 per cent supplying users with sharps boxes, there is a discrepancy between the availability of injecting equipment, particularly through sales, and the facilities for safe disposal. However, Table 1 shows high levels of willingness by pharmacists to provide this service. If all these pharmacies began providing facilities for safe disposal, the level of provision in Bro Taf would be more than doubled.
It was always hoped that pharmacy-based needle exchange would expand organically from small beginnings, and that those not actively taking part would, as a minimum, be able to direct people to the nearest site. The service has not developed as anticipated. Those who have left the scheme give
a few reasons, but several other factors may be of relevance. Ten years ago it was not clear that the war against HIV would be as successful as it has been and the epidemic of hepatitis C among IDUs has failed to motivate new services in the same way. The success of the HIV campaign may have led to
some misplaced complacency among those who should be co-ordinating NES. Locally, cuts to specialist services and seemingly endless reorganisation of institutions at all levels may well have distracted attention from this essential task. The good news is that there is a body of pharmacists who
report being willing to provide needle exchange services waiting to be enrolled, which would increase provision levels to higher than in 1995.13
In 1995, two-thirds of pharmacists in Wales expressed a need for further training in drug misuse and HIV/hepatitis prevention, and 80 per cent of pharmacists in Bro Taf expressed such a need in this survey.13 This level is comparable with that found in RCT and Merthyr 10 years ago.5 The seeming enthusiasm may simply reflect the naivety of the question, but again needs a positive local response.
That almost four in 10 pharmacists did not know the whereabouts of the nearest needle exchange supports the self-reported need for further training. A pharmacist has recently been appointed to the new post of needle exchange co-ordinator by Bro Taf Health Authority, following recommendations made in a review of NES in 1999.18 The co-ordinator will have primary responsibility for community pharmacy-based NES and for liaising with the Community Drug and Alcohol Team in RCT and Merthyr, the Community Addiction Unit in Cardiff and the Vale of Glamorgan, and voluntary services. The central co-ordination of services will secure appropriate recruitment, training, continuing professional support and remuneration for all the community pharmacists willing to contribute.
The percentage of pharmacies dispensing Controlled Drugs in Bro Taf in 2000 (55 per cent) is higher than levels across Wales in 1995 (41 per cent).13 Supervised consumption of methadone in Bro Taf is available in 25 per cent of dispensing pharmacies, but it is important to note that 31 of the 40 (70 per cent) are based in only one of the four areas. A scheme for supervised consumption of methadone was introduced in RCT and Merthyr in 1994, before the establishment of Bro Taf and has continued successfully despite early reservations. Until 1997, most methadone prescribed in Cardiff and the Vale of Glamorgan was dispensed in-house from a satellite hospital pharmacy in Cardiff. Hence, little co-operation from community pharmacists was needed.
Plans are in hand to formalise a scheme across Bro Taf, with pharmacists being paid for this additional service, in line with other areas of the UK. The survey again finds evidence of untapped willingness on the part of a number of pharmacists to engage in this essential work, and this number increases if you add those pharmacists that gave “no payment” as the reason for not wanting to supervise consumption of methadone. Unfortunately, in 2000 the proportion of pharmacies in Bro Taf that were currently involved or willing to become involved in service provision for drug users was lower than the reported levels for Wales in 1995.13 It is regrettable that 17 pharmacies (9.5 per cent) in Bro Taf had previously provided these services, but were no longer willing to do so.
CONCLUSION
There has been little change in the level of pharmacy based service provision for drug users in Bro Taf over the past decade. This study highlights current levels of provision and similarities to earlier findings. 5,13. Community pharmacies are often the best placed outlets to operate harm reduction measures for drug users. Linking up the many pharmacists who report being willing to expand their services with funding, training and support from the new needle exchange co-ordinator, offers the best opportunity to improve services for many years. Another survey measuring levels of service provision for drug users in community pharmacies in the future may be useful in assessing the effect of these new developments. Acknowledgement of the spread of hepatitis C through injecting drug users
should also be a stimulus for growth in services.
ACKNOWLEDGEMENTS
Many thanks to Jan Wichter who drove SL to every pharmacy in Bro Taf, to all the pharmacists who completed questionnaires, and to Janie Sheridan and John Strang for allowing us to adopt and adapt their questionnaire.
REFERENCES
- Stimson GV, Alldritt L, Dolan K, Donoghoe M. Syringe
exchange schemes for drug users in England and Scotland.
BMJ 1988;296:1717–9. - Council of the Royal Pharmaceutical Society of Great
Britain. Guidelines for pharmacists involved in schemes to
supply clean needles and syringes. Pharm J 1989;251:20. - Council of the Royal Pharmaceutical Society of Great
Britain. Sale of hypodermic needles and syringes. Council
Statement. Pharm J 1986;236:205. - Sheridan J, Lovell S. Turnbull P, Parsons J, Stimson G,
Strang J. Pharmacy-based needle exchange (PBNX) schemes
in South East England: A survey of service providers. Addic-
tion 2000;9510:1551-1560. - McBride AJ, Meredith-Smith P, Davies ME. Helping inject-
ing drug users: a role for community pharmacists. Pharm J
1993;250:708–9. - Greater Glasgow Health Board. Guidelines for supervision of
methadone consumption in pharmacies. 3rd Ed. Glasgow:
The Health Board; 2000. - McBride AJ, Ali MI, Atkinson R. Supervised administration
of methadone by pharmacies. BMJ 1994;309:1234. - Glanz A, Byrne C, Jackson P. Role of community pharmacies
in prevention of AIDS among injecting drug misusers: Find-
ings of a survey in England and Wales. BMJ 1989;299:
1076–9. - Sheridan J, Strang J, Barber N, Glanz A. Role of community
pharmacies in relation to HIV prevention and drug misuse:
Findings from the 1995 national survey in England and
Wales. BMJ 1996;313:272–4. - Matheson C, Bond C. Community pharmacists’ involvement
with drug misusers: a Scottish national survey of pharmacists’
attitudes and practices. Report to chief scientist office, Scot-
tish Office Department of Health. Aberdeen: Department of
General Practice and Primary Care, University of Aberdeen;
1997. - Sheridan J, Strang J, Taylor C, Barber N. HIV prevention
and drug treatment services for drug misusers; A national
study of community pharmacist’s attitudes and their involve-
ment in service specific training. Addiction 1997;92:1737–48. - Review of needle and syringe exchange scheme — South
Glamorgan 1989–1993. Report to South Glamorgan Health
Authority. Cardiff: South Glamorgan Health Authority;1993. - Sheridan J, Strang J. Community pharmacy in Wales: 1995
data on HIV prevention and drug misuse services. J Mental
Health 1998;7:203–10. - Pates R, McBride AJ, Li S, Ramadan R. Misuse of over-the-
counter drugs: a survey of pharmacies in a South Wales
Health Authority. Pharm J. In press.
15 Bro Taf Health Authority. Community pharmacy needle
exchange scheme: annual report for 1999/ 2000. Report to
Bro Taf Health Authority. Cardiff: Bro Taf Health Authority;
2000. - Welsh Drug and Alcohol Unit. Welsh Drug Misuse Data-
base: Report for the year 1 January to 31 December 1996.
Report to Welsh Office. Cardiff: Welsh Drug and Alcohol
Unit; 1997. - Welsh Drug and Alcohol Unit. Drug misuse in Wales: a
report from the Drug Misuse Database for the years 1998 and - Report to the National Assembly for Wales. Cardiff:
Welsh Drug and Alcohol Unit; 2000. - Walker M. A review of the Bro Taf community pharmacy
needle exchange scheme. Report to Bro Taf Health Authori-
ty. Cardiff: Bro Taf Health Authority; 1999.


