Abstract
Aim
To evaluate a pilot of a community pharmacy-based travel health and vaccination service.
Design
A self-completed questionnaire.
Subjects and settings
Two community pharmacy pilot sites: one in Aberdeen and one in Aberdeenshire. All patients who attended the pharmacies for travel advice and services were asked to participate.
Results
The median score for the overall service was 10 (interquartile range 9–10). 98% of respondents (n=84) would use the pharmacy service again and 81.4% thought the pharmacy service provided value for money. Most clients were travelling on holiday and some found the community pharmacy could provide a more convenient venue and appointment times. Only a small number of clients had needed to be referred to other travel health providers, eg, Grampian NHS Travel Clinic.
Conclusion
The pharmacy travel health service was well accepted by patients and met their needs. Most patients believed the community pharmacy service provided value for money.
In 2005, UK residents made a record 66.4 million visits abroad, up by 4 per cent on the number of visits made in 2004 and an increase of 14 per cent over the previous five years.1 Although Europe remains a popular choice for many holidaymakers,1 cheap flights and holiday programmes have prompted many travellers to seek more exotic destinations that pose greater risks to their health.
In 2005, more than 8.7 million journeys were made to “risky” destinations such as Asia, Africa and Central America.1 As many as one fifth of these travellers may be travelling to risky locations without receiving appropriate immunisations.2 Travellers are often confused about the vaccinations they need2 and may receive conflicting advice from different sources (eg, travel agent, travel brochure, internet). Currently travel immunisations are provided either by a traveller’s own GP, via NHS travel clinics (a service provided by some, but not all, health boards in Scotland) or via private travel clinics (often associated with work-related travel).3
Within the UK, travel medicine services can be delivered in a number of ways. Usually within a general medical practice it will be the role of the practice nurse to provide travel advice and administer the immunisations. The practice would be required to provide the appropriate prescription for any malaria prophylaxis or immunisation required.
Some vaccines are allowable on an NHS prescription (eg, typhoid, hepatitis A, poliomyelitis) and are subject to NHS standard prescription charges, although it is unclear how general practices choose to deliver travel medicine under the new general medical services contract. Other vaccines and prescription-only antimalarial prophylaxis are available privately through general practice and a fee may be charged. The NHS Grampian travel clinic also charges a fee for the provision of these travel vaccines.
Private health care companies may also provide travel medicines and will charge the full commercial cost of all the services provided (often associated with work-related travel).
The cost of travel health provision to the traveller can, therefore, vary from no payment required, if exempt from prescription charges and allowable on the NHS, to payment of full commercial prices, which may include a fee for the consultation.
The provision of immunisations from community pharmacies in the UK is a recent development although there are published reports of pharmacists offering immunisation services in the US and the Netherlands.4–12 The US was the first country to recommend the introduction of pharmacist administration of vaccines, in a 1971 report on the pharmacist’s clinical role.13 The role of US pharmacists in immunisations stemmed from a need to improve childhood immunisation rates but this later transformed into a primarily adult immunisation service. Grampian, in north-east Scotland, has led the way in the UK by offering influenza vaccinations from community pharmacies.14,15 Other areas of the UK are now providing influenza immunisation services using community pharmacists.16
Although some community pharmacists undertake immunisations such as influenza, pneumococcal and some childhood immunisations, there are no published data to indicate that community pharmacists are administering immunisations related to travel. However, they have for many years successfully provided advice and made recommendations for travel immunisations and supplied malaria prophylaxis,17,18 although some non-UK studies found that pharmacists’ knowledge of travel medicine was incomplete and could be improved.19,20 The logical extension is to combine both the advice and the immunisation functions within the community pharmacy setting supported by enhanced training.
An assessment of the public’s perceived need for a travel vaccine service from community pharmacies has been previously undertaken within NHS Grampian.21 This study showed that nearly three-quarters of respondents (74.8 per cent) agreed or strongly agreed that the community pharmacy would provide a convenient location from which to obtain travel services, and 70.2 per cent of respondents agreed that pharmacy could provide a one-stop shop for travel medicine services.
Members of the travelling public already visit community pharmacies and most of these are travelling for holiday purposes. The needs assessment study suggested that travellers would be prepared to use the community pharmacy to provide travel advice and immunisations.
This feasibility study explored uptake and acceptability of travel health and vaccination services delivered from community pharmacies. The main research questions addressed were:
- Could a “gold standard” service be developed?
- Would patients access such services from a community pharmacy?
- Did the patients find the service acceptable?
- Could the community pharmacist deliver the services to the necessary standard?
- How could the pilot of service delivery be implemented across other community pharmacies within Scotland?
Method
Development of the service
On the basis of the needs assessment study,19 the service currently provided by the NHS Grampian travel clinic and a literature review, a “gold standard” service was defined. All pharmacists providing influenza immunisation were given the opportunity to participate and were invited to attend a two-day travel medicine training course. Two pharmacies were chosen for their location, local need and ability to deliver a regular clinic. One was an urban community pharmacy in Aberdeen and the other was in rural Aberdeenshire.
Pharmacist interviews
Semi-structured interviews were undertaken with eight community pharmacists who currently provide influenza immunisation, who also had expressed an interest in developing travel health services and who attended the travel health training provided by NHS Grampian. The pharmacists were asked to consider the practicalities of delivering a “gold standard” service. Pharmacists identified training and resource issues and these were addressed in developing the training. All the pharmacists supported the idea of a pharmacy travel health service. They identified a need for further knowledge on co-administration of vaccines and undertaking a traveller health needs assessment.
Development of protocols and patient group directions
To allow pharmacists to provide immunisations and prescription-only medicine (POM) antimalarials, patient group directions (PGDs) were written and approved. These were then signed off by NHS Grampian. However, PGDs could not be written for Japanese B encephalitis vaccine (which is unlicensed) or for yellow fever vaccine (which must be given through registered centres). Pharmacists were provided with a resource pack (Panel 1) containing copies of the PGDs, protocols for administration of vaccines, appropriate documentation (assessment/recording forms, general practice notification forms, patient questionnaires) and references sources.
Panel 1: Travel medicine service — community pharmacy resource pack contents
Front
Outline of study
Section 1
Travel medicines risk assessment and vaccine record forms
Section 2
Travel query log
Section 3
- Useful contact numbers
- Materials required
- Referral criteria
- Preparation of vaccine
- Patient questions
- Needlestick injury protocol
- Vaccination protocol
- Pharmaceutical presentation
Section 4
Patient group directions:
- Adrenaline
- Vaccines
- Cholera (oral)
- Influenza Diphtheria/tetanus/IPV (Revaxis)
- Meningitis ACW135Y Vax
- Hepatitis A
- Pneumococcal
- Hepatitis B
- Rabies
- Hepatitis A and B
- Tick-borne encephalitis
- Hepatitis A and typhoid
- Typhoid
Section 5
Patient group directions: malaria haemoprophylaxis:
- Mefloquine
- Doxycycline
- Malarone
Section 6
Travel health products checklist
Section 7
Notification of immunisation to GP
Section 8
Leaflets
UK best practice guidance
Section 9
Patient information leaflet
Patient evaluation questionnaires
Section 10
Return envelopes for audit questionnaires
Pharmacist training
Pharmacists who would be providing the pilot travel immunisation clinic attended “The basic requirements”, which is a standard travel health course provided by Travel Health Related Education any health professionals who are involved or interested in the provision of travel health advice and vaccine administration. The course is aimed at those who are new to the field of travel medicine, but is also suitable for anyone wishing to update and expand their current knowledge.
The key principle underpinning the training was an understanding of the risk assessment aspect of travel medicine. The topics covered included:
- Principles of immunisation
- British schedule vaccines
- Travel vaccines
- Sources of information
- Travel health on the internet
- Risk assessment
- Food- and water-borne diseases
- Malaria
- Animal- and insect-borne diseases
In addition, NHS Grampian provided refresher anaphylaxis training and training on vaccine reconstitution and disposal, PGDs and relevant health and safety issues. Pharmacists were also provided with guidance on referral criteria (eg, for pregnant travellers and those requiring yellow fever vaccination, which can only be provided from specialist registered centres).
The course provided pharmacists with a comprehensive list of recommended travel health publications and resources. Travax, the Malaria Reference Laboratory, and the National Travel Health Network and Centre (NaTHNaC), ‘Immunisation against infectious disease’ (the “green book”) are just a few of the resources used by the pharmacists when providing the service. Support and advice was also available from the NHS Grampian travel clinic staff.
Pilot service
Both pharmacy services started in late summer 2006. Publicity was organised by the NHS Grampian corporate communications team. The service was self-funding, with patients paying a private fee for the service provided.
The fees were mutually agreed between the individual pharmacies and NHS Grampian and depended on the service or vaccine provided. The fees were generally greater than that charged by the NHS travel clinic, but less than local non-NHS private travel medicine providers.
Evaluation of the service
Development of questionnaire
A questionnaire was developed to evaluate the pharmacy service from the perspective of the patient. It was based on an audit of patient satisfaction conducted by the NHS Grampian travel clinic a few years earlier, with additional questions relevant to the pharmacy service following a review of the literature and after discussion among the authors. The local research ethics committee advised that formal ethical review was not required for this evaluation of a service development.
The questions covered:
- Demography
- How the patient heard about the serviceand reasons for choosing pharmacy
- Ease of making an appointment andmethod of transport
- Opinions about the pharmacy providingthe service, eg, professional attitude, standard of premises and usefulness of advice
- Services and advice provided
- The pharmacy attended
- Value for money
- Whether the patient would use the phamacy again for travel medicine services
- Overall rating of service on a Likert scale from 1 to 10
The questions were a mixture of open, closed, Likert scale and multiple choice questions. Respondents were also asked for any additional general comments on the service. Pharmacists invited all patients attending the service to complete a questionnaire, either in the pharmacy, preferably during the 10-minute post-immunisation wait, or later at home, and to return it direct to the researcher in a stamped, addressed envelope. All forms were anonymous. There was no mechanism to identify non-responders for reminders to be sent or for other follow-up.
Pharmacy patient records
A clinical record was made for every patient consulting the community pharmacist for travel health advice. The record comprises patient data (age, sex, relevant medication and immunisation history), travel destination(s), immunisations and antimalarial medicines provided by the pharmacy service. This information was also used by the researchers to describe the patient population receiving the service.
Data management and analysis
Results from the questionnaire were entered into an SPSS database, which was used to determine frequencies and for statistical analysis.
Results
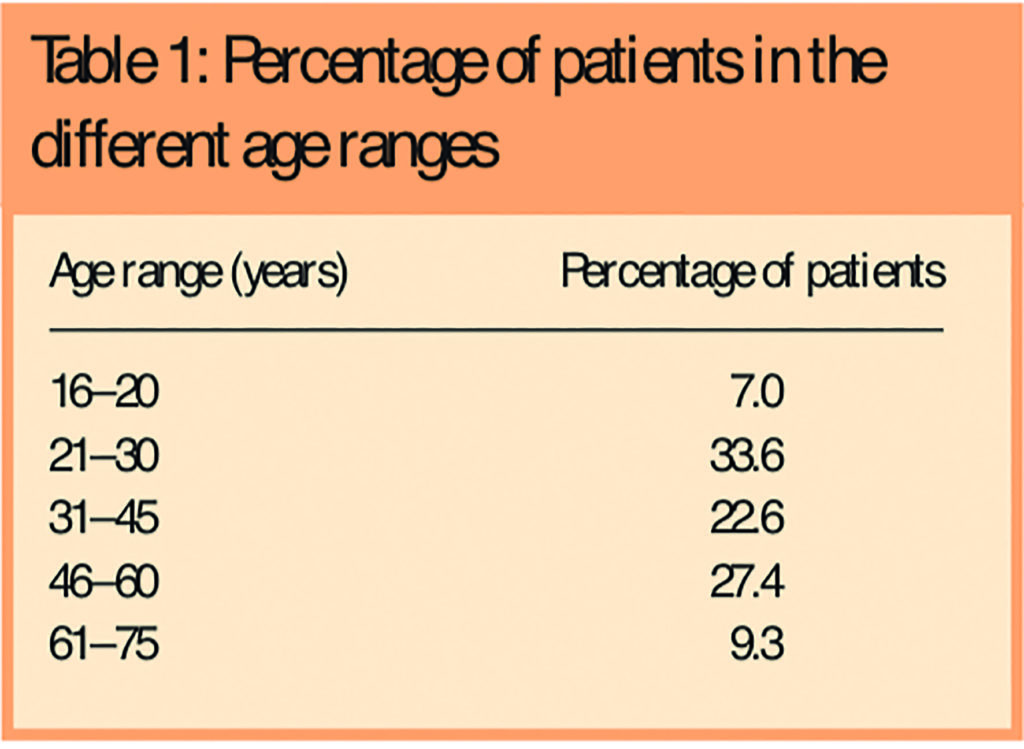
The two pharmacies saw 137 patients between August 2006 and March 2007 (Aberdeen 107, Aberdeenshire 30). The pharmacists reported that 125 questionnaires were issued (families/couples only received one questionnaire between them in Aberdeenshire). Eighty-nine questionnaires were returned (response rate 71.2 per cent). There was an even split between the number of male and female patients. The age range distribution can be seen in Table 1.
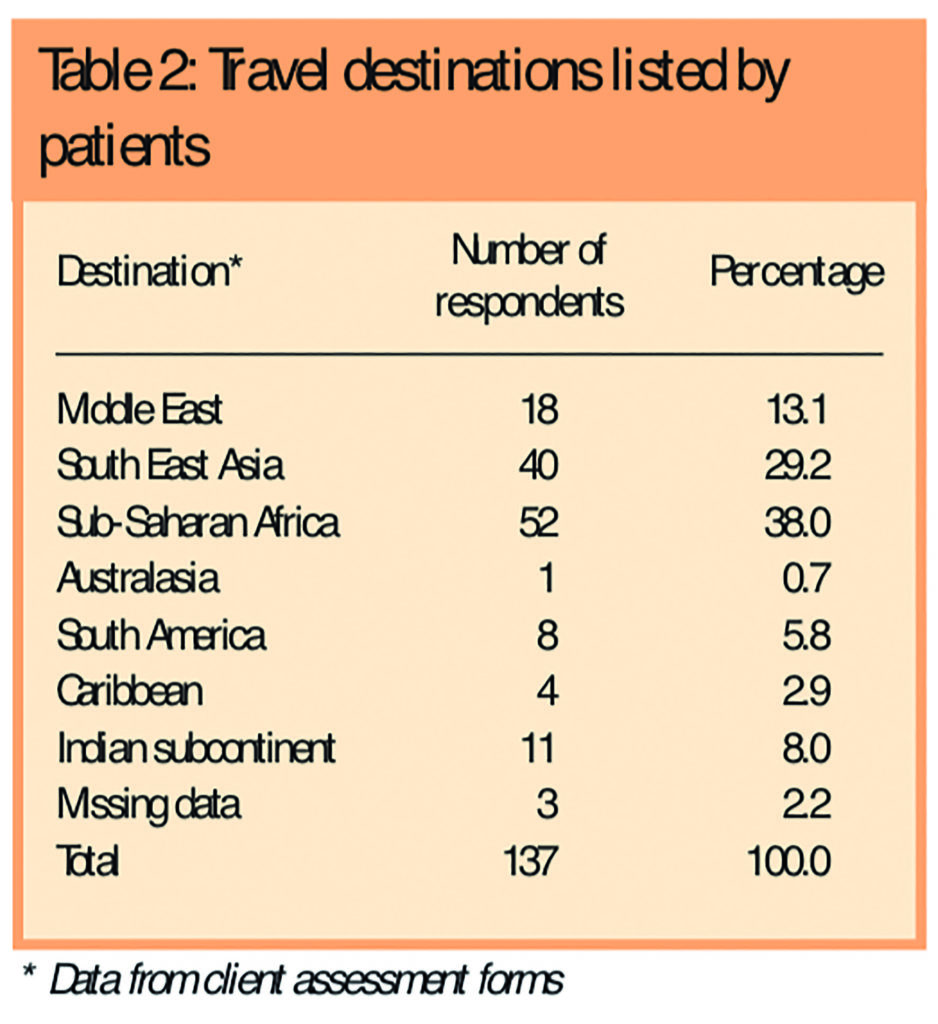
Thirty-eight per cent (n=52) of patients who attended the pharmacy travel clinics were intending to travel to sub-Saharan Africa and 29.2 per cent (n=40) to South-East Asia. Other destinations are listed in Table 2.
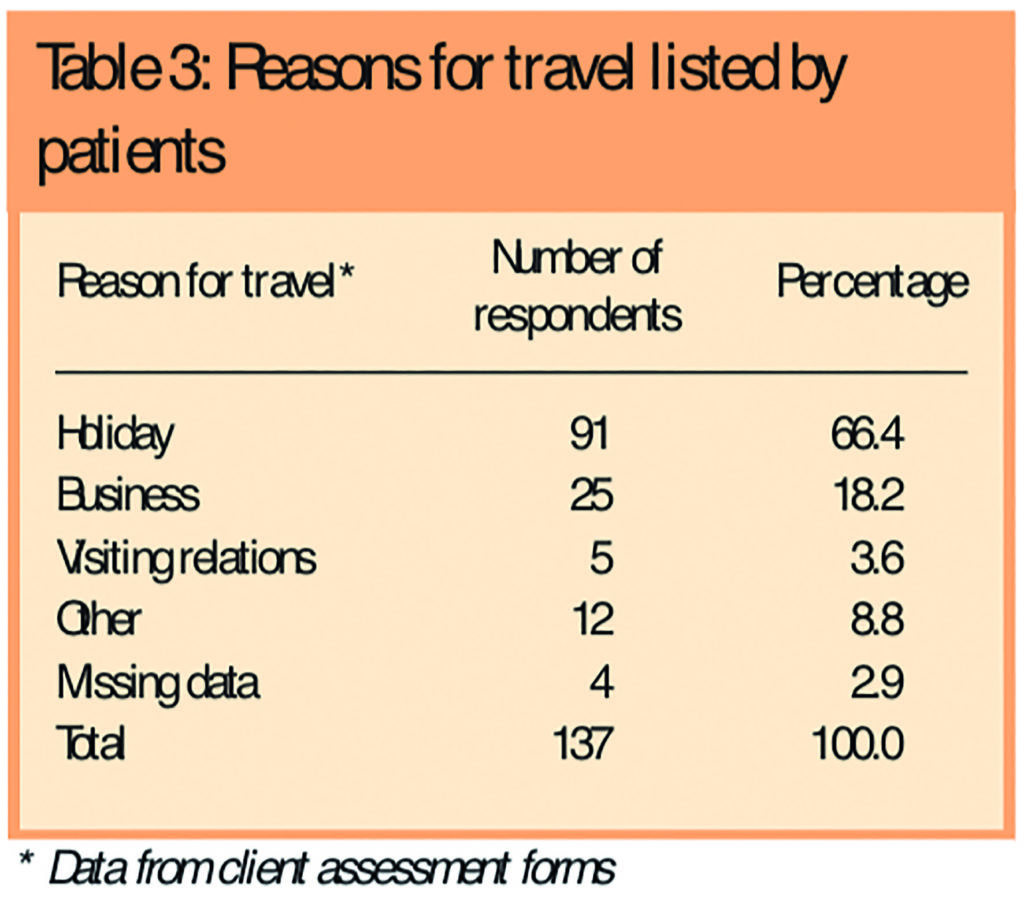
Sixty-six per cent (n=91) of respondents were going abroad on holiday and 18.2 per cent (n=25) on business (Table 3).
Respondents chose the pharmacy service over other providers because the venue was convenient (23 per cent; n=32), the time was convenient (16 per cent; n=22) and they were able to get an early appointment (15 per cent; n=20). Fourteen per cent of respondents (n=19) stated that their general practice did not provide a travel medicine service.
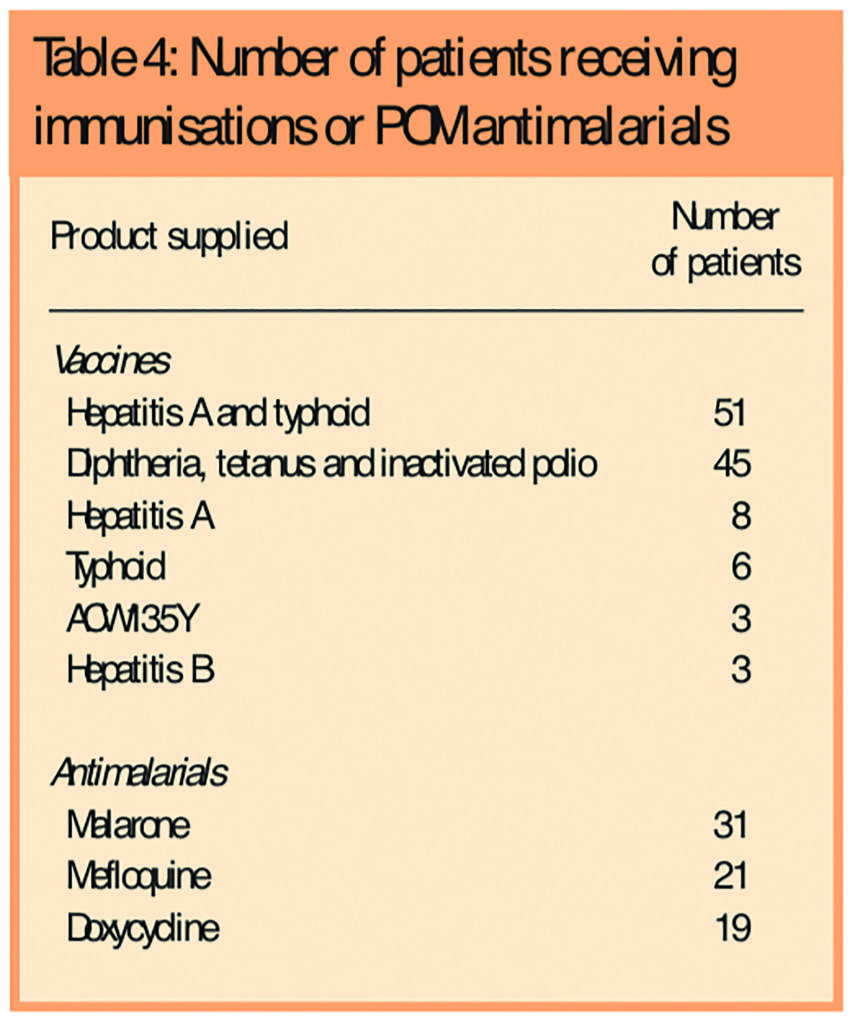
Seventy-two per cent of respondents (n=62) received an immunisation and 50 per cent (n=43) received malaria prophylaxis from the pharmacy service. Only 18.6 per cent (n=16) required referral to their general practice or NHS Grampian travel clinic (eg, for yellow fever vaccine or Japanese B encephalitis vaccine, which can only be provided from specialist centres).
Table 4 details the vaccines administered and POM antimalarials supplied, identified using the patient records.
All questionnaire respondents thought that the pharmacist had explained clearly the options for treatment and what they were doing. Additionally, all respondents thought that the pharmacist had provided all the information and service required. No questionnaire respondent stated that the consultation was not polite, professional or confidential. Ninety-eight per cent of respondents (n=84) would use the pharmacy service again and 81.4 per cent (n=70) thought the pharmacy service provided value for money.
When asked about the overall rating of the service, questionnaire respondents were asked to rate this on a scale of 1 to 10, with 10 indicating an excellent service. The median response was 10 (interquartile range 9–10).
Many patients provided positive comments about the service, as the following quote from the open-ended questions illustrates:
A very worthwhile service which should be extended to other pharmacies. Service was informative, patient and I received excellent customer service from the pharmacist prior to my vaccinations and after.
Some especially valued the personal touch of the community pharmacy, for example:
As I frequently travel to inhospitable parts it’s comforting, reassuring and more enjoyable to return to my home city and see an established company keeping up with modern times yet still providing a personal touch to a great level of service. The travel clinic will be invaluable in the future.
One respondent appreciated the thoroughness of the pharmacist, but commented that it took some time:
My only very small complaint is that the pharmacist took a long time to sort me out — partly because they were checking something they did not know: where the low risk areas in India were.
Discussion
Overall, the pharmacy travel health service from the two pharmacies appears to meet patient need. Most clients were travelling on
holiday and some found the community pharmacy could provide a more convenient venue and appointment times. Only a few clients needed to be referred to other travel health providers such as their general practice or the NHS Grampian travel health clinic for yellow fever and Japanese B encephalitis immunisations.
The two-day training course provided pharmacists with a basic grounding in travel health issues and risk assessment skills to support their existing knowledge base. Pharmacists participating in the scheme have continued to develop their skills in this area as part of their continuing professional development.
The evaluation has shown that a “gold standard” service, acceptable to patients, can be developed and delivered through community pharmacies. The service was only delivered through two community pharmacies and evaluated for a relatively small number of patients and hence extrapolation to the wider pharmacy community cannot be assured. Longer-term follow-up of these patients would be valuable to determine if they returned to community pharmacy for further consultations.
In most cases, the questionnaire was completed in the community pharmacy following the consultation and this may have resulted in a slightly biased response. However, the patients did respond anonymously, directly to the researcher and the response rate was good.
Patients did raise the issue that some of the immunisations provided by the pharmacist would have been free, or at the cost of a prescription charge, if they could have obtained these from their GP. However, many travel health medicines, including all antimalarials, are not allowable on the NHS. Most patients believed the community pharmacy service provides value for money.
The community pharmacists participating in the pilot scheme from both pharmacies are enthusiastic to continue with the service and believe they are providing a service that their patients need. The numbers of patients accessing the service is currently manageable, but still increasing.
Further development of other community pharmacy travel health centres is planned to meet future demand and we realise it is important to replicate the enthusiasm of the community-pharmacy pioneers in rolling out the programme.
Travel medicine services within medical practices are reimbursed as part of their general immunisation service provision, which also includes non-travel immunisations. In developing the service further consideration will be given to integrating the pharmacy service closer with other NHS providers.
Conclusion
The pharmacy travel health service appears to be well accepted by patients and can meet their needs. The community pharmacist has been identified as one of the key providers of public health advice and this project has shown that they can provide an accessible travel health service on the high street. Patients will be more likely to be better prepared before travelling abroad and there will be clear benefits to both the NHS and patients. The project empowers patients by offering a choice between providers and reflects the NHS priorities to increase access to service and increase patient choice. The project allowed the development of an evidence base within pharmacy practice to support a new clinical role for pharmacists. There is now a need to consider the long-term delivery of the service and its closer integration with other NHS travel health services.
Acknowledgements
This project was supported by a Chief Scientist Office, Scottish Executive Health Department Primary Care Research Career Award. Thanks are given to Charles Michie, FRPharmS, and Mhairi Brand, MRPharmS, for their participation.
About the authors
Caroline Hind, PhD, MRPharmS, is pharmacist facilitator in the NHS Grampian pharmacy medicines unit at Woodend Hospital, Aberdeen; Christine Bond, PhD, FRPharmS, is professor of primary care pharmacy, and Amanda J. Lee, MSc, PhD, is professor of medical statistics, in the academic centre for primary care, University of Aberdeen; and Edwin van Teijlingen, MEd, PhD, is reader in public health in the university’s department of population health.
Correspondence to: Caroline Hind, Pharmacist Facilitator, Pharmacy Medicines Unit, Westholme, Woodend Hospital, Queen’s Road, Aberdeen AB15 6LS (e-mail caroline.hind2@nhs.net)
References
- Office for National Statistics. Travel trends: A report on the 2005 International PassengerSurvey. Basingstoke: Palgrave Macmillan; 2006.
- Travellers to exotic places risk illness by not having vaccinations. Pharmaceutical Journal 2001;267:182.
- Burnett JCD, Buchan F, Mackenzie AR. Review of 1 year’s activity in the Grampian travel clinic:importance of the oil industry. Journal of Travel Medicine 2005;12:122–6.
- Davidse W, Perenboom RJ. Increase of degree of vaccination against influenza in at-riskpatients by directed primary care invitation [in Dutch]. Nederlands Tijdschrift voor Geneeskunde 1995;139:2149–52.
- Madhavan SS, Rosenbluth SA, Amonkar M, Borker RD, Richards T. Pharmacists andimmunizations: a national survey. Journal of the American Pharmaceutical Association 2001;41:32–45.
- Grabenstein JD, Guess HA, Hartzema AG. People vaccinated by pharmacists: descriptiveepidemiology. Journal of the American Pharmaceutical Association 2001;41:46–52
- Smith C. Pharmacy-based immunizations. US Pharmacist. 1999;24(8):38–47.
- Sokos DR. Pharmacists role in increasing pneumococcal and influenza vaccination. AmericanJournal of Health-System Pharmacy 2005;62:367–77.
- Ndiaye SM, Madhavan S, Washington ML, Shui L, Tucker J, Rosenbluth S, Richards T. The use ofimmunisation services in rural communities. Public Health 2003;117:88–97.
- Tarleton Landis, N. More pharmacists administering vaccines. American Journal of Health-System Pharmacy 1997;54:490–3.
- Weitzel KW, Goode JVR. Implementation of a pharmacy-based immunisation programme in a supermarket chain. Journal of the American Pharmaceutical Association 2000;40:252–6.
- Ernst ME, Bergus GR, Sorofman BA. Patients’ acceptance of traditional and nontraditional immunisation providers. Journal of the American Pharmaceutical Association 2001;41:53–9.
- Hind CA, Peterkin GSD, Downie G, Michie CA, Chisholm E. Provision of flu immunisation from a community pharmacy in Aberdeen. Pharmaceutical Journal 2004;273:194–6.
- Hind CA, Downie G. Vaccine administration in pharmacies – a Scottish success story. Pharmaceutical Journal 2006;277:134–6.
- Report of the Task Force on the Pharmacist’s Clinical Role. Journal of the American Pharmaceutical Association. 1971;NS11:482–5.
- Pharmacists trained to give flu vaccines. Pharmaceutical Journal 2005:275:328.
- Jackson AB, Humphries TL, Nelson KM, Heiling DK. Clinical pharmacy travel medicines services: a new frontier. Annals of Pharmacotherapy 2004;38:2160–5.
- Mason, P. What advice can pharmacists offer travellers to reduce their health risks? Pharmaceutical Journal 2005:273;651–6.
- Toovey S. Malaria chemoprophylaxis advice: survey of South African community pharmacists’ knowledge and practices. Journal of Travel Medicine 2006:13(3):161–5.
- Teodósio R, Gonçalves L, Imperatori E, Atouguia J. Pharmacists and travel advice for tropics in Lisbon (Portugal). Journal of Travel Medicine 2006:13(5):281–7.
- Hind CA, Bond CB, Lee AJ, van Teijlingen E. Needs assessment study for community pharmacy travel medicine services. Journal of Travel Medicine 2008;15:328–34.


