To view the full infographic, click here.
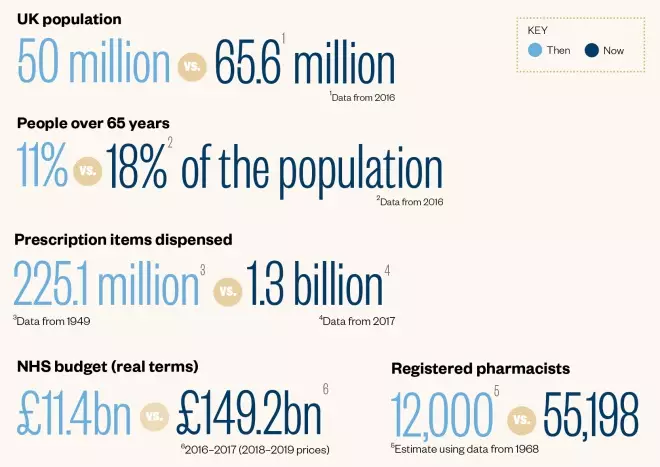
The big numbers
1948 versus 2018
1948: Health secretary, Aneurin Bevan (pictured), launches the National Health Service (NHS) entitling people to free prescriptions and therefore drastically increasing dispensing volumes within community pharmacies

Source: PA Images
1953: A wider role for hospital pharmacists is recognised in the Linstead Report, including greater involvement on the wards, in medical education in teaching hospitals and in making medical decisions alongside prescribers
1958: Pharmacists become responsible for the safe and secure handling of medicines within a whole hospital, not just the pharmacy department, following a government inquiry and the subsequent publication of the Aitken Report

Source: Alamy Stock Photo
1963: A committee on safety of drugs is set up to try to avoid another disaster like that of thalidomide (pictured), which was withdrawn in 1961 after suspicions it caused birth defects. The committee creates a system of reporting adverse drug reactions that becomes known as the ‘Yellow Card Scheme’
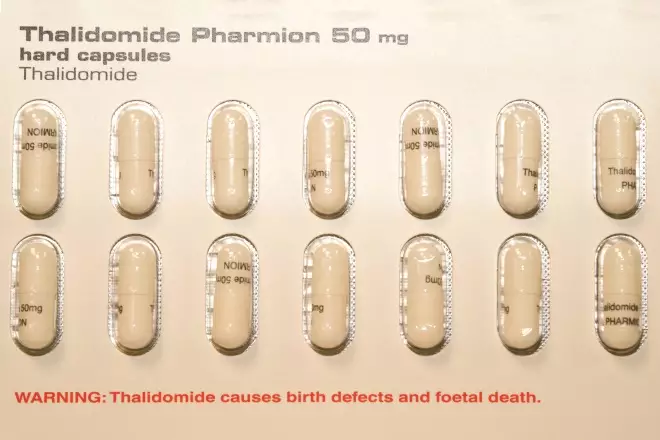
Source: Science Photo Library
1968: The Medicines Act 1968 brings together existing medicines legislation and establishes a licensing system for medicines. It also introduces the concept of pharmacy (P) medicines
1971: The hospital pharmacy service is reorganised on the back of a report from Sir Noel Hall, which suggests restructuring the service to increase career prospects and making better use of resources and expertise
1981: The Conservative Party’s Minister for Health, Gerard Vaughan, admits to the 1981 British Pharmaceutical Conference that he cannot see a future for community pharmacists. This leads to the Nuffield inquiry report of 1986, which, for the first time, recognises a wider role for community pharmacists
1983: First switches from prescription-only medicines to P medicines occur, including ibuprofen, loperamide and terfenadine, widening pharmacists’ role and increasing access for patients

Source: Science Photo Library
1985: The number of medicines prescribable on the NHS is reduced to exclude many cough remedies, digestives, laxatives and analgesics, creating a renewed demand for over-the-counter medicines

Source: Alamy Stock Photo
1986: A pharmacy on-call system is introduced in hospitals after the Nuffield Report describes hospital pharmacy as a “clinical pharmacy service” and recommends 24-hour cover
1987: Regulations restricting the opening of new pharmacies are introduced in the UK, with new pharmacies having to prove that their NHS service is “necessary and desirable”
1991: Nicotine gum becomes the first form of nicotine replacement therapy to be made available from pharmacies, paving the way for NHS pharmacy-based smoking cessation services

Source: Science Photo Library
1992: Pharmacies in Scotland start to offer supervised methadone consumption services; English pharmacies follow from 1996
Source: Alamy Stock Photo
1997: The Yellow Card Scheme is extended to hospital pharmacists, and to community pharmacists two years later. A four-year Master of Pharmacy course is introduced to prepare pharmacists for their extended NHS roles
1999: The National Institute for Clinical Excellence is established, with the aim of creating consistent guidelines and ending the ‘treatment postcode lottery’. The Scottish Medicines Consortium follows in 2001, and the All Wales Medicines Strategy Group in 2002
2001: Schering launches Levonelle, the first emergency hormonal contraception available as a P medicine, widening pharmacists’ role in women’s health

Source: Science Photo Library
2003: Supplementary prescribing for pharmacists is introduced following publication of the NHS Plan 2000, which set out a policy on non-medical prescribing to improve patient care
2005: A new community pharmacy contract is introduced in England and Wales, which rewards provision of high-quality NHS services as well as dispensing volume. Exemptions to the “necessary and desirable” test for market entry are introduced in England, including supermarket, 100-hour, primary care centre and distance-selling pharmacies. The electronic prescription service is launched in England, although implementation is slow

Source: Alamy Stock Photo
2006: Pharmacist independent prescribing is introduced. A new community pharmacy contract is launched in Scotland that moves away from payment by prescription volume for the first time and includes a national minor ailment scheme
Source: Alamy Stock Photo
2009: The Royal Pharmaceutical Society introduces mandatory continuing professional development for pharmacists
2011: New market entry arrangements come into force in Scotland. Regulations in England follow in 2012, implementing market entry tests based on pharmaceutical needs assessments and removing existing exemptions for 100-hour, primary care centre and supermarket pharmacies. Regulations are amended in Wales in 2015
2013: Primary care trusts in England are abolished and replaced by clinical commissioning groups as commissioners of NHS pharmacy services. Local authorities become commissioners of NHS public health services from community pharmacies. A national minor ailment scheme is launched in Wales
2014: Primary care clusters are established in Wales, expanding the role of pharmacists in general practice
2015: Community pharmacists in England are granted access to a summary of patient records and a pilot of pharmacists in GP practices is funded by the government. An NHS seasonal influenza vaccination service is introduced in England

Source: Science Photo Library
2016: An overhaul of community pharmacy funding in England is announced by the government, including cutting the total budget by 4% for 2016/2017 and a further 3.4% for 2017/2018, scrapping establishment payments and introducing a new quality payment scheme
2017: NHS England publishes national guidance on a range of medicines that should no longer be routinely prescribed in primary care, with the aim of saving £140m a year
2018: Revalidation for pharmacists and registered pharmacy technicians is introduced. Inadvertent dispensing errors are decriminalised, ending a ten-year battle to remove the threat of criminal prosecution for community pharmacists

Source: Shutterstock.com
References
Sources: 1948: National Archives; 1953–1958: Making Medicines: A Brief History of Pharmacy and Pharmaceuticals; 1963: Medicines and Healthcare products Regulatory Agency; 1968: Royal Pharmaceutical Society; 1971: Making Medicines: A Brief History of Pharmacy and Pharmaceuticals; 1981: prescriber.co.uk; 1983: Proprietary Association of Great Britain; 1985: The Pharmaceutical Journal; 1986: Making Medicines: A Brief History of Pharmacy and Pharmaceuticals; 1987: National Archives; 1991: The Pharmaceutical Journal; 1992: BMJ; 1997: Medicines and Healthcare products Regulatory Agency and The Pharmaceutical Journal; 1999: National Institute for Health and Care Excellence, Scottish Medicines Consortium & All Wales Medicines Strategy Group; 2001: The Pharmaceutical Journal; 2003: National Archives; 2004–2018: The Pharmaceutical Journal.
Information for the data panels was gathered from: UK population: Office for National Statistics; people over 65 years: Office for National Statistics & Office of Health Economics; prescription items dispensed: Office of Health Economics, Welsh Government, NHS National Services Scotland, The Pharmaceutical Journal & HSC Business Services Organisation; registered pharmacists: Royal Pharmaceutical Society & General Pharmaceutical Council; NHS budget: Institute for Fiscal Studies & House of Commons Library.
Infographic: MAG.


