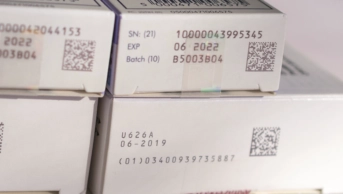
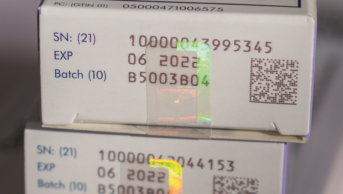
Courtesy of Raj Patel
Community pharmacists should not have to pay for scanners and other technology needed to implement the Falsified Medicines Directive (FMD) without government assurances on funding, the chair of the UK FMD working group for community pharmacy has said.
Raj Patel said existing financial pressures on community pharmacy made an outlay on FMD kit “hard to justify”, but added pharmacies were “mandated to comply” with the directive, which is due to come into force on 9 February 2019, and so they should proceed towards implementation “with caution”.
“In terms of costs, in an environment of attrition it’s too much to expect contractors to implement FMD without any assurances from the Department of Health and Social Care on funding,” he said.
“It’s a matter for the Pharmaceutical Services Negotiating Committee and its counterparts in the devolved nations to negotiate, but we are hopeful that the government will cover the full cost of this extra regulatory burden.”
Community pharmacists are still waiting for an official estimate of the cost of implementing FMD, with just six months until the go-live date.
The Medicines and Healthcare products Regulatory Agency (MHRA) published an assessment of the impact of FMD on wholesalers, parallel distributors and the so-called ‘Article 23 institutions’ — non-healthcare institutions who supply medicine to the public, such as care homes, opticians and prisons — in July 2018. But this assessment did not cover the potential costs to community or hospital pharmacists.
A spokesperson from the MHRA told The Pharmaceutical Journal on 2 August 2018 that “having produced a focused impact assessment for Article 23 of the Delegated Regulation, the MHRA has not published a UK-specific full impact assessment, and does not intend to publish one at this point in time”.
According to a 2015 assessment from the EU Commission, a pharmacy/retailer community pharmacist would be expected to face costs of around €530 per year to modify software for FMD compliance, purchase new barcode scanners and perform medicines authentication. A hospital pharmacy, the report said, would face annual costs of up to €750.
Patel said there is additional uncertainty on “just how long the FMD system will be needed for”. As it stands, the UK is expected to be able to access the European Medicines Verification System (EMVS) — also known as the EU Hub — during the Brexit transition period. In theory, under Article 7 of the Withdrawal Bill, the UK could lose access to all EU networks and information systems and databases post-transition. But the UK government is aiming for regulatory alignment on medicines policy that would allow for continued access.
Patel said that the group recommends that “whatever system pharmacies choose, they ensure that termination of the contract without penalties is possible, in the remote possibility there is no workable UK FMD repository”.